CA: CorVel Increases PR-2 Payments Following daisyBill Webinar
Workers’ comp is messy. But it works much better when providers, claims admins, employers, and all other stakeholders understand that we’re in this mess together — and are willing to learn from each other.
A perfect example: representatives of Third-Party Administrator (TPA) CorVel attended our recent webinar on updates to the 2024 Physician Fee Schedule (available to stream here), and learned something that allowed CorVel to correct erroneous bill adjustments.
During the webinar, daisyBill demonstrated that CorVel was not paying providers the increased reimbursement of $15.19 for Primary Treating Physician’s Progress Reports (aka PR-2s). To CorVel’s credit, the TPA moved quickly and decisively to correct the problem and is currently reimbursing providers at the updated rates.
CorVel Discovers, Fixes Outdated Reimbursement Rate
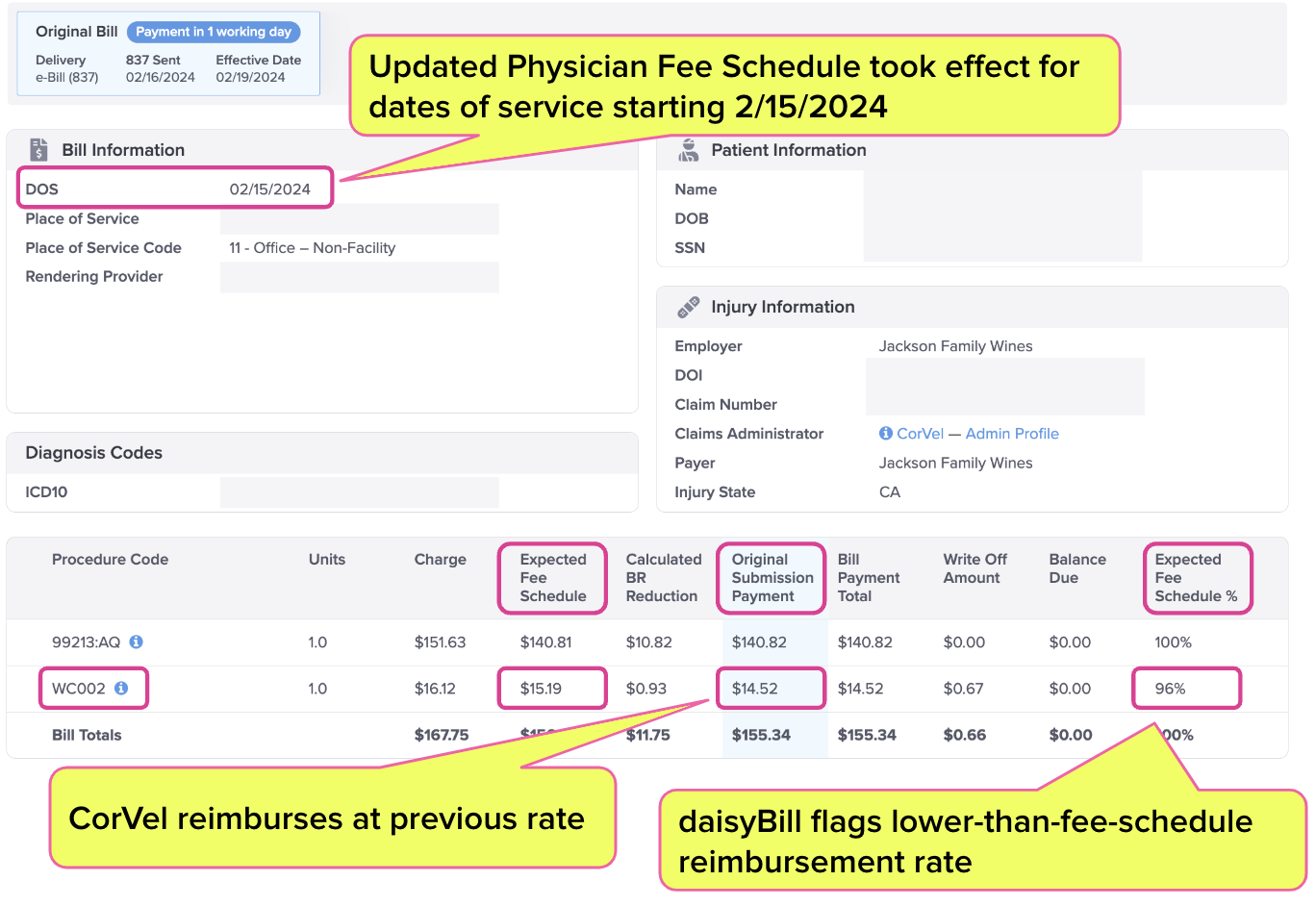
To underscore the importance of checking reimbursements against the latest fee schedule updates, our webinar included an example of a bill CorVel erroneously adjusted, which included a PR-2 report.
Providers bill for PR-2s using California-specific billing code WC002 — reimbursement for which increased to $15.19 for dates of service on or after February 15, 2024.
The daisyBill screenshot below highlights the discrepancy between the ‘Expected Fee Schedule’ payment and CorVel’s payment for a February 15 service date. By applying the previous reimbursement rate, CorVel mistakenly paid WC002 at only 96% of the new rate.
As it happened, CorVel representatives attending the webinar saw this example and immediately reached out to daisyBill to identify the bill in question. Once CorVel found the source of the problem, the TPA updated its systems to ensure that providers were paid correctly.
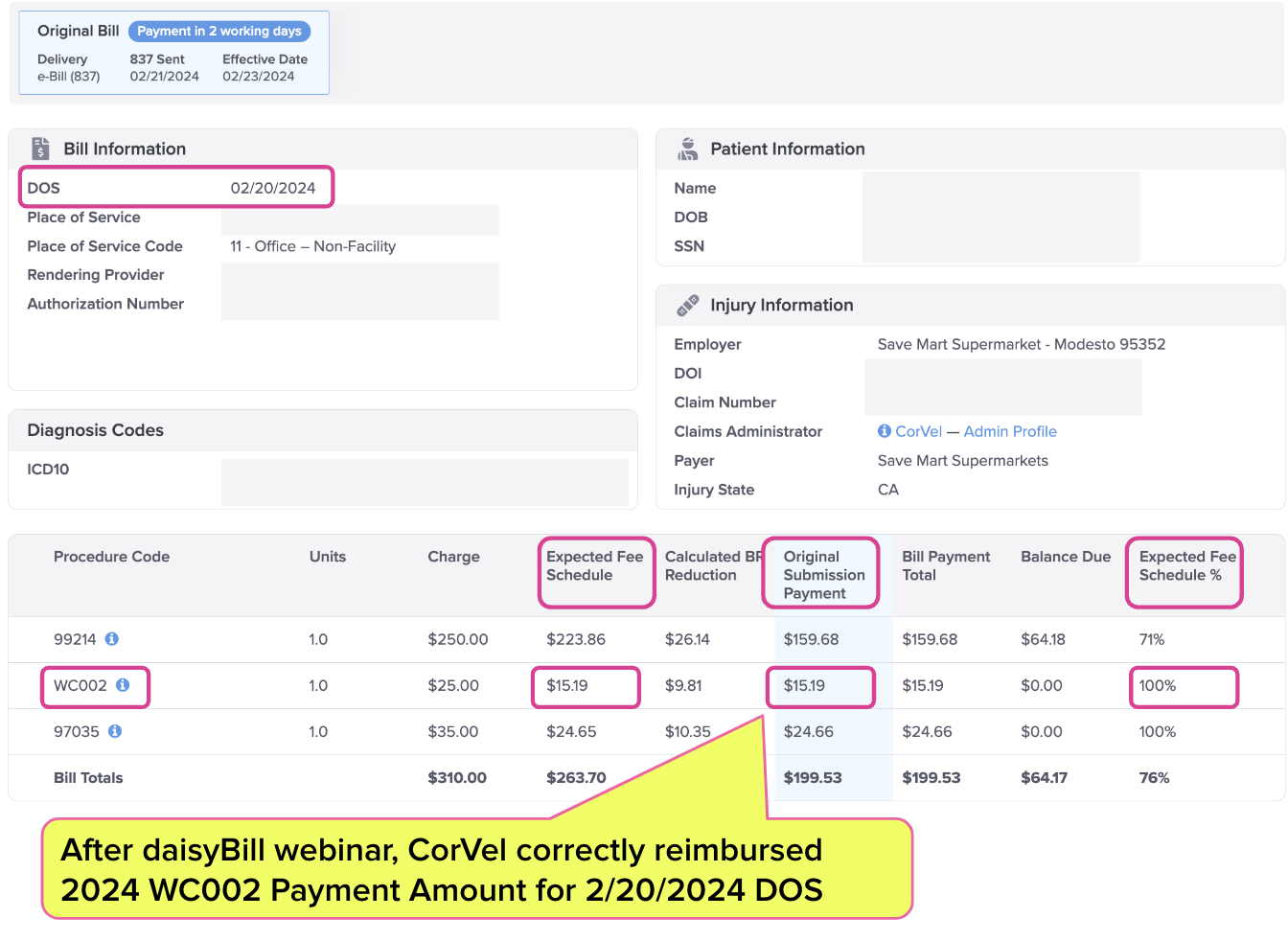
Since CorVel addressed the mistake, reimbursement rates for WC002 are up to date, as shown below.
The difference between reimbursement rates for WC002 before and after February 15 is a matter of cents (a 4.6% increase) — but outdated reimbursement rates across countless bills and billing codes can add up to significant revenue loss.
Fortunately (in addition to mastering technology to the point of not requiring a clearinghouse to accept e-bills), CorVel takes its obligations to providers seriously enough to immediately tackle an error when they see one. That’s a compliment we can’t give to every claims administrator in the game.
More importantly, this story demonstrates how technology is the answer to the inevitable missteps that occur in the deeply complex world of workers’ comp billing.
By instantly recognizing discrepancies (and patterns of incorrect payments or non-compliance), e-billing doesn’t make billing challenges magically disappear. However, it makes those problems much more easily detectable and solvable.
When both sides of the billing and payment equation act in good faith (as CorVel did) and apply the right tech (as daisyBill did), the result is a workers’ comp system that can actually function well for all concerned — especially injured workers.
Know (and get) exactly what you’re owed for treating injured workers. Get instant, accurate fee schedule calculations with daisyWizard’s OMFS Calculator.
TRY THE CALCULATOR
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.
.gif)