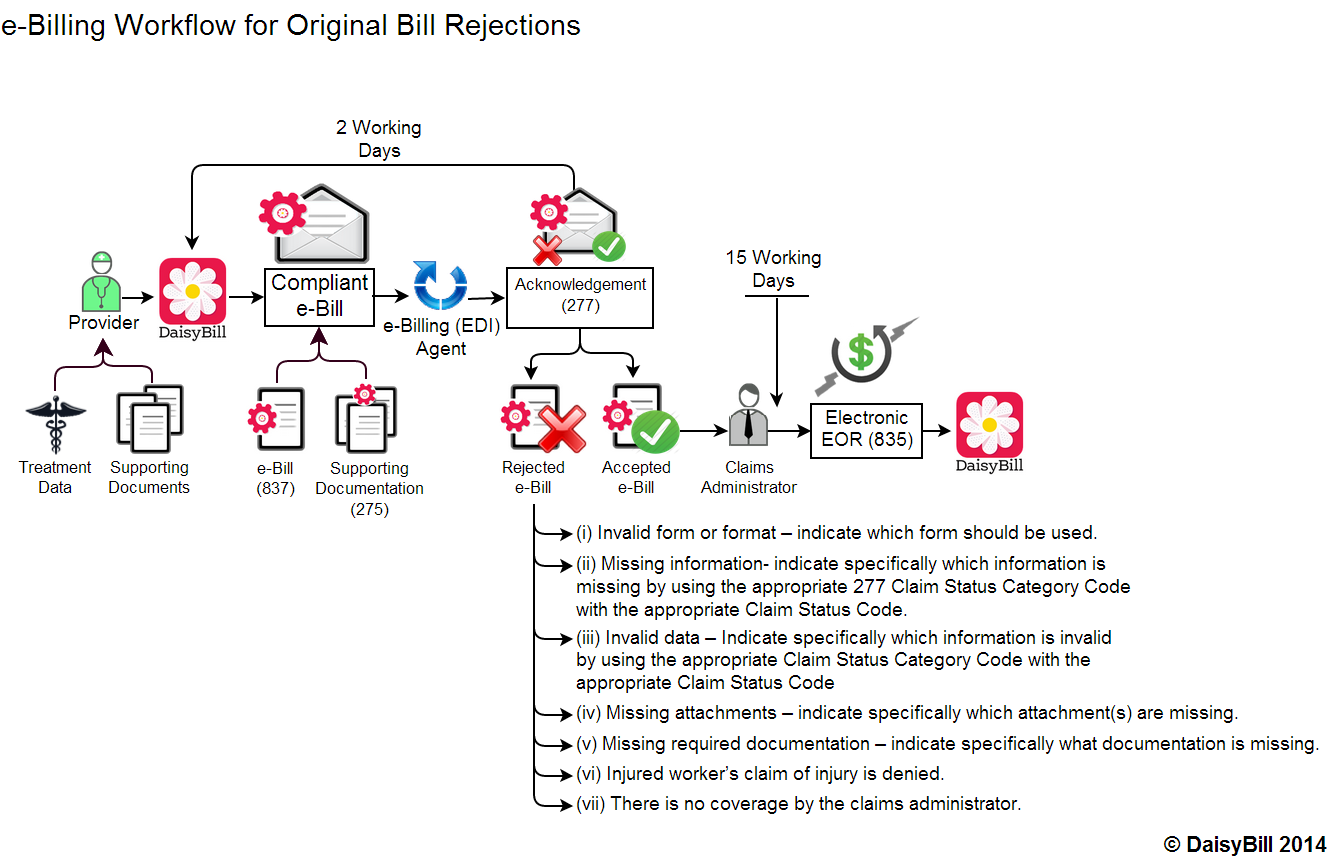
Electronic Billing Workflow with Rejection Information
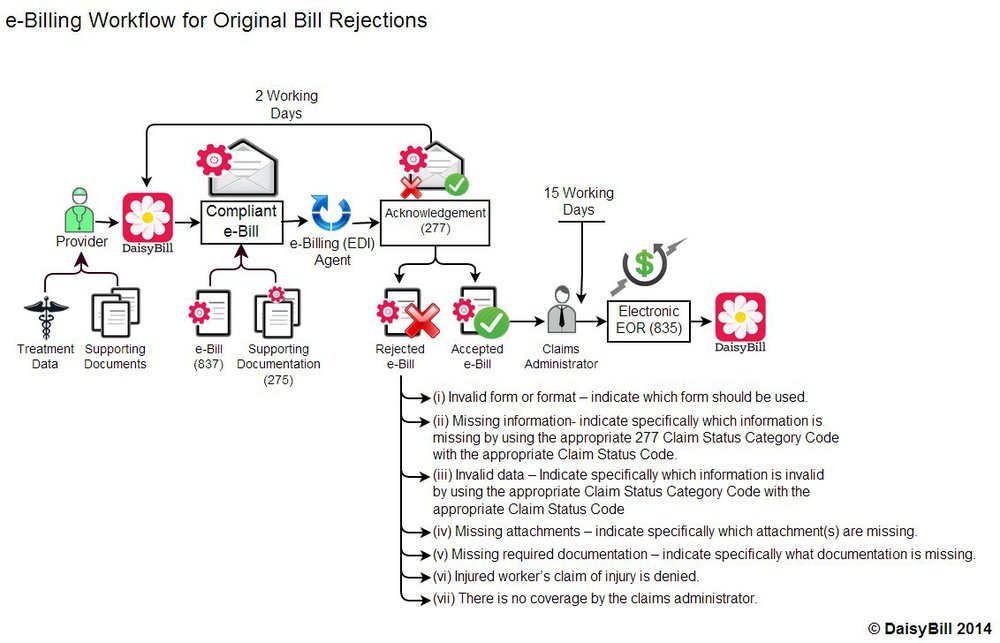
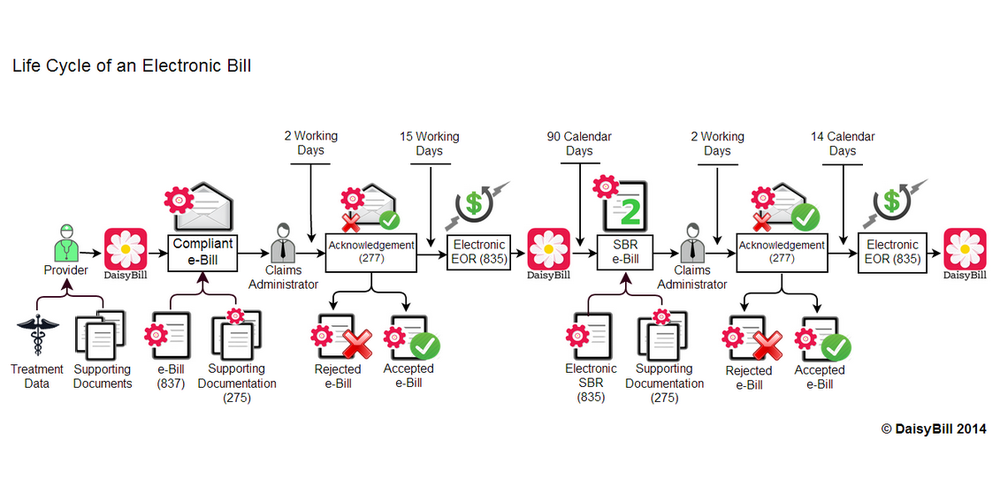
Last week I posted the first of several workflows (I’ll post the rest this week and next week) showing how a workers’ comp electronic bill progresses through its journey from provider to claims administrator and back. Today I’m adding details to the workflow, explaining the specific information that must accompany a rejected electronic bill.
Electronic Billing Tip
For electronic billing purposes, it is important to understand the difference between a rejection and a denial.
- A rejection happens within the first two days and signals that the bill is somehow not eligible for adjudication by the claims administrator, such as when there is missing information.
- A denial happens when the claims administrator received all the required information for adjudication, and has weighed the merits of the bill and decided not to pay it. An example of the latter is a denial based on lack of authorization.
The regulations specify that:
“the claims administrator shall send a Health Care Claim Acknowledgement ASC X12N 277 electronic notice of whether or not the bill submission is complete. The ASC X12 N 277 details what errors are present, and if necessary, what action the submitter should take... Such notice ...must include specific information setting out the reason for rejection.”
California Division of Workers’ Compensation Medical Billing and Payment Guide, 7.0 Bill Processing and Payment Requirements for Electronically Submitted Treatment Bills; 7.1 Timeframes; (a) Acknowledgements (3)
Want more information about electronic billing? Visit our Webinar Library, a free workers' comp resource:
WEBINAR LIBRARY
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.