How to Confirm Whether a Payer Accepts e-Bills for Workers' Comp

Far too often, we hear from providers who were told that a given claims administrator “doesn’t accept” e-bills.
Erroneously (or downright falsely; we can’t say for sure), some claims administrators or their vendors insist that e-billing is not an option — even when state law mandates the claims administrator accept e-bills.
It’s time to end the confusion.
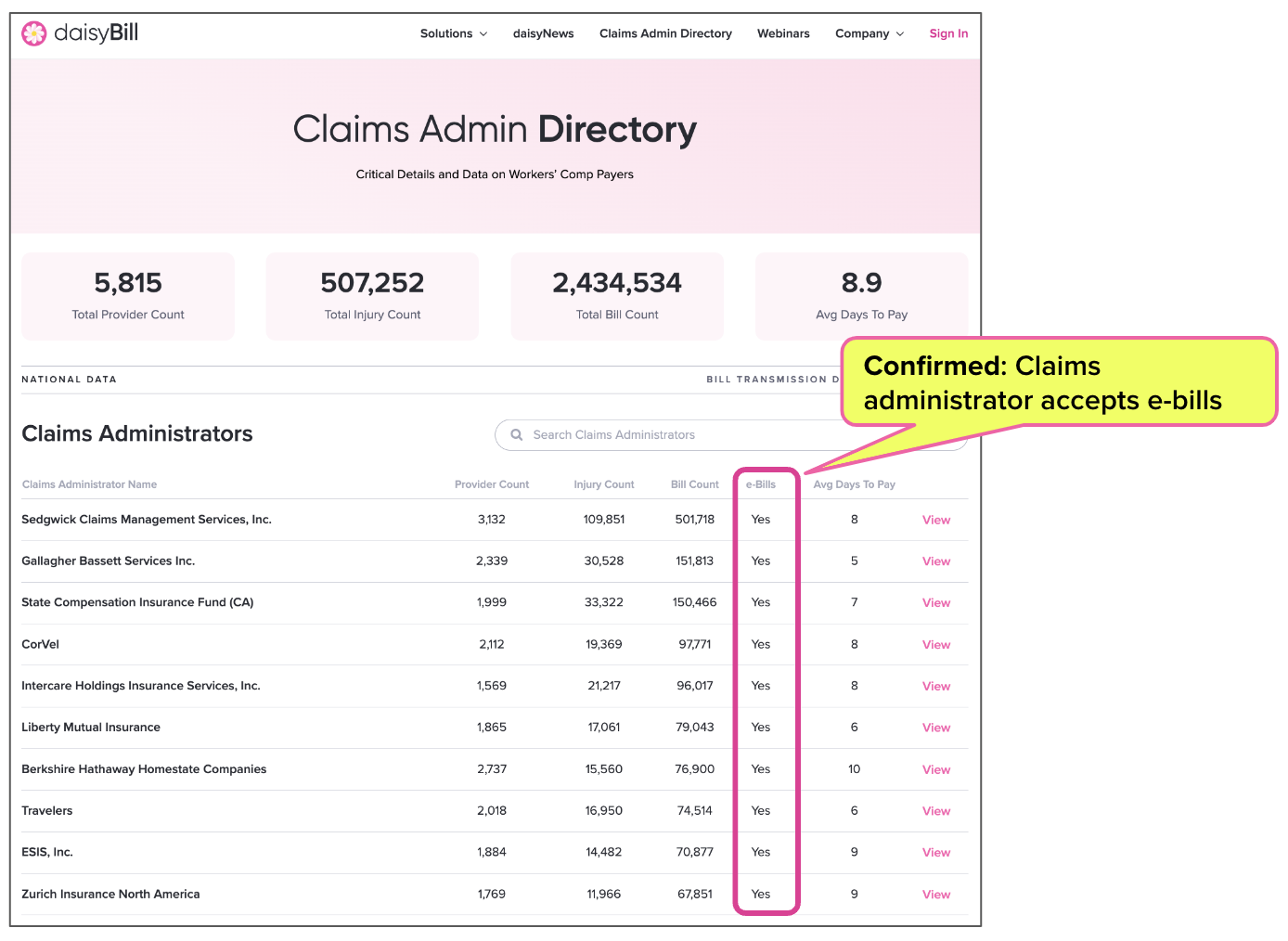
daisyBill’s free, public Claims Administrator Directory now lists whether or not each of the 697 claims administrators in our system is confirmed to accept e-bills. When in doubt, don’t take their word for it — head to the Directory and find out for yourself.
Check e-Billing Status: daisyBill Claims Administrator Directory
The Claims Administrator Directory has a wealth of information on each claims administrator, including contact information, compliance data, and more. Enter the claims administrator’s name into the search field to find the information you need.
The Directory home page answers a simple question for each claims administrator: do they accept e-bills? The answer is yes in most cases, as indicated in the ‘e-Bills’ column.
This means that daisyBill has confirmed that practices can e-bill the claims administrator — no matter who tells you otherwise (including the claims administrator).
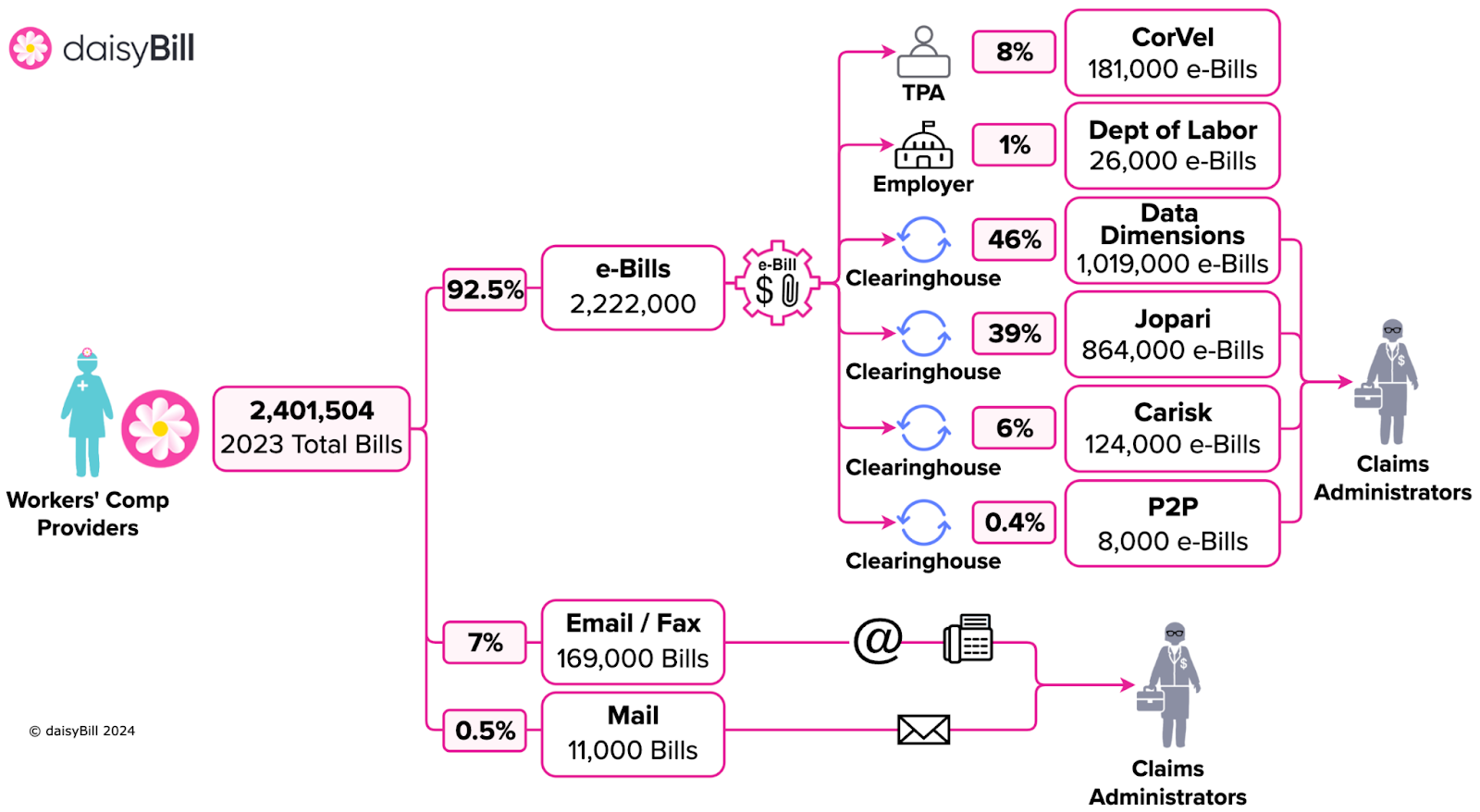
As shown below, daisyBill delivers over 92% of our clients’ bills electronically as e-bills, with a small percentage sent via email or fax (and half a percent sent through the mail). That’s because our software connects directly to each clearinghouse* hired by claims administrators to accept e-bills.
*daisyBill also delivers e-bills directly to the two claims administrators, CorVel and the federal Department of Labor, that do not require a clearinghouse.
Take advantage of the Claims Administrator Directory, and reach out to us via chat (bottom right corner of this page) or email with any questions. We’re here to help.
Nationwide, daisyBill increases revenue and decreases hassle for providers who treat injured workers. Get a free demonstration below.
SCHEDULE DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.
Just because a claim admin "accepts e-bills" does not always guarantee they have access to their clearing house. It also does not guarantee that the clearing house forwarded the e-bills to bill review. I have ran into this issue several times with certain claim admins.
We had PhysNet tell us they only accepted claims by fax or US mail. They gave us this ridiculous list of protocols they wanted us to abide by. Then only paid a small fraction of what we are entitled to. We stopped doing business with them. Recently they contacted us to try to get an injured worker on our schedule. We said no. They kept emailing us offering to pay us more money. We still said no. Then they wanted to know what they could do to get the injured worker on our schedule. So, I told them. 1. You do not accept bills electronically. (they are required to by law) 2. You don't compensate us correctly. 3. You take forever to pay us. 4. You have too many demands for scheduling. 5. You want reports the same day as treatment. 6. Your EOB's are always off on the amounts paid, they don't add up. Sent that to them. They emailed again saying they now accept claims electronically via Jopari and they could go up on the amount paid and wanted to know what that amount would need to be. I responded saying for the Initial Eval alone we need to get 162.18. (thanks to Daisybill fee calculator) then told them how much the rest of our payments should be. They said, okay thanks we can't meet that amount. No problem with that on our end. Then what happens? The insurance carrier contacts us directly about getting that patient on our schedule cutting out the middle-man. We have them sign an auth for out of network provider, and we get what we are entitled to in every aspect. Thank you Daisybill for giving our office the power to say no to these TPA's that were draining our practice of valuable resources and paving the way for us to take charge of treating injured workers and getting them back to work in our community from the skilled treatment they get in our clinic. Say No to PPO's. TPA's go away! It's not your Day! Regarding Mia's comment, they don't need to have access their clearinghouse but I'm sure they do have access. The clearinghouse generates the 277 info in their system allowing you to follow the claim yourself. That shows you everything related to each claim sent from your end.