NYSIF Switches Bill Review and Clearinghouse
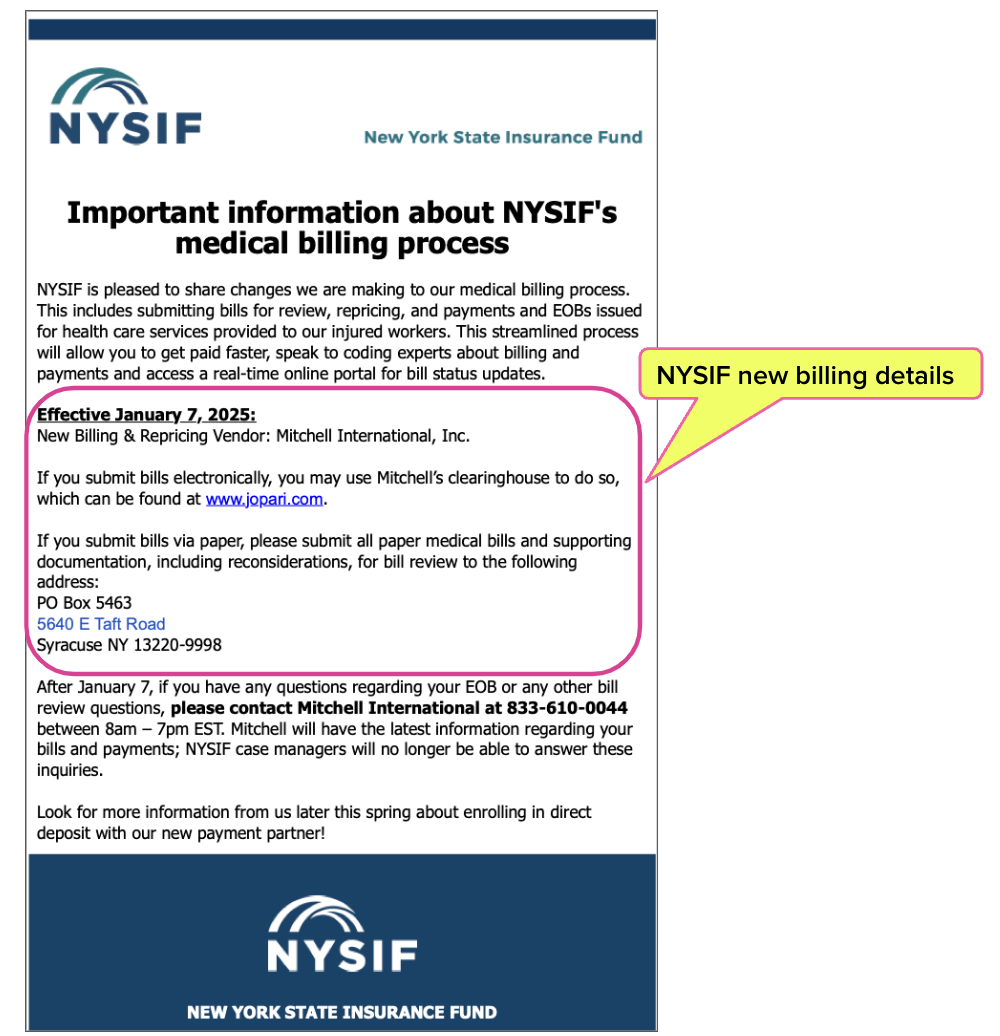
The New York State Insurance Fund (NYSIF) is changing its bill review and electronic billing clearinghouse vendors. Effective January 7, 2025, NYSIF will use:
- Mitchell International, Inc. for its bill review vendor, and
- Jopari for its clearinghouse vendor to accept bills that providers send electronically (e-bills).
daisyBill providers do not need to take any action. daisyBill will automatically route all NYSIF e-bills to Jopari beginning on January 7th.
The mailing address for paper bills will also change. As a reminder, beginning August 1, 2025, New York mandates that providers send all workers' comp bills electronically.
The new billing details for NYSIF are below.
Sending Bills to NYSIF Effective January 7, 2025
According to a recent announcement (below), effective January 7th, NYSIF instructs providers to send their e-bills to Jopari, the clearinghouse vendor used by Mitchell.
The NYSIF announcement does not include the new Payer ID Jopari assigned to NYSIF. However, according to a recent Jopari Payer ID list, when sending e-bills to NYSIF, providers should use Jopari Payer ID 45052.
The new mailing address for paper bills is as follows:
PO Box 5463
5640 E Taft Road
Syracuse, NY 13220-9998
Important note: the message above instructs providers to contact Mitchell with “questions regarding your EOB or any other bill review questions” after January 7.
However, in the case of improper payment denials or reductions, the New York Workers’ Compensation Board (WCB) instructs providers to use the established procedure for billing and payment disputes. Per the WCB website:
“Payers are required to pay a health care provider's bill in full or submit a Notice of Objection to Payment of a Bill for Treatment Provided (Form C-8.1B) within 45 days of submission. If a payer has failed to do this, the health care provider may be able to request the Board's assistance by filing Form HP-1.0 through OnBoard.”
daisyBill is a New York State WCB-approved e-billing vendor. For questions about New York e-billing requirements, contact our experts using the pink chat icon in the bottom right of this screen, or email us at info@daisybill.com.
We make the switch to e-billing easy. daisyBill is a WCB-approved XML submission partner. Please request a free demonstration of our software below.
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.



Ever since Mitchell has taken over NYSIF claims processing, it has been a disaster!!! They are denying EVRYTHING for No Auth! They also are issuing C8.1's on EVERYTHING, even on claims that they say are going to be paid! I've never seen anything like it! It started with them denying/issuing C8.1's for x-rays taken in office at our orthopedic office. There is a rule that states that claimants must use an "In Network Diagnostic Provided", but there are certain circumstances in which the claimant can have x-rays taken in office, this mainly pertains to Orthopedics' Offices, where this rule states, "x-rays can be taken during an office visit, if used for diagnosis and treatment of fractures/possible fractures, joint dislocations, tumors, infections, loosening of surgical implants, dislocation of prosthetic joints, spinal instability or follow-up to surgery." This information can be found on NYS WCB's website under/search: Board Bulletins and Subject Number 046-480. https://www.wcb.ny.gov/content/main/hcpp/hcpp.jsp The carrier NYSIF (Mitchell), does not even pay any claims anymore, everything is denied for No Auth and then C8.1'd, leaving the NYS WCB Judges completely overwhelmed and also denying claims, agreeing with C8.1's that deny orthopedic office's x-rays, which are a necessity for the proper care of our patients/claimants. It is hard enough to get paid in NYS for seeing Worker's Comp patients, then along some new carrier (that does not know what they are doing) taking over NYSIF (a huge carrier for NYS Compensation). I wish I could send you some of the CRAZY denials we have received, but I do not see anywhere I could upload them. If there is anything you are able to do, (spread the message) it would be greatly appreciated. (I'm sure other orthopedic offices would agree). Unfortunately, we as providers are not able to object to Notices of Decisions, so we do not even have a fighting chance. I have attempted to connect with claimants' attorneys to have them file "objections" to the NOD, I have even emailed the NYS Medical Director's Office, in hopes that someone can do something. If there is a way to upload documents here, please notify me, these denials/C8.1's are outrageous!!