Second Bill Reviews in 500 Words or Less

Consider this the SparkNotes or Cliff Notes for Requests for Second Review (also known as Second Bill Reviews (SBRs)). You should really read the book but this shortcut will help you out in a pinch. Workers’ comp medical billing has never been shorter.
For more detail and fuller explanations of the SBR process, watch a free recording of our SBR webinar here -- it includes downloadable slides.
Request for Second Review (SBR) Summary
When a provider is underpaid or not paid at all for a workers’ compensation bill, the appeal process starts with the Request for Second Review (SBR), but only if the disagreement arises due to the amount of reimbursement. SBRs are only for payment disputes.
Where are the SBR Rules?
- CCR § 9792.5.5 Second Review of Medical Treatment Bill or Med-Legal Bill, Subdivisions (a)-(i)
- Labor Code §4603.2, Subdivisions (e) and (f)
The Regulations and the Labor Code spell out everything you need to know about work comp SBRs. Always come back to these sources, but be warned that it’s pretty dense reading.
When Should an SBR Be Filed?
A provider can file an SBR within 90 days of :
- Receiving an explanation of review, or
- A decision of the Workers’ Compensation Appeals Board regarding a threshold issue related to the bill
This is a serious deadline because if providers don’t file within 90 days, then no further money is due.
What Is the Form or Method for Filing an SBR?
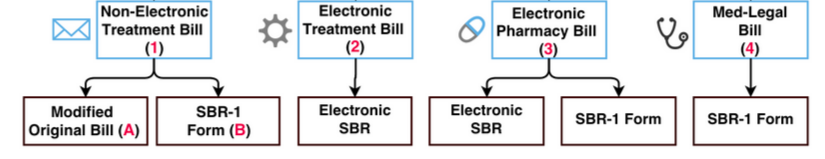
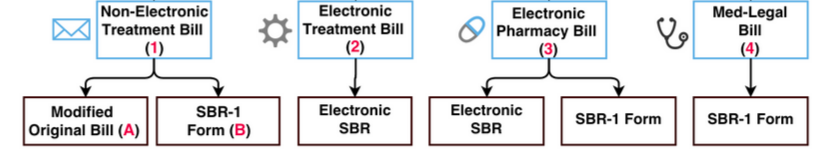
The method for filing an SBR depends on the method used to file the original bill. Here’s a handy diagram:
So, for instance, if the original bill was a non-electronic treatment bill on paper (CMS 1500), then the SBR must be submitted on paper, using either a modified original bill or the SBR-1 form.
Is the SBR-1 Form Mandatory?
Although, in some circumstances, the DWC allows providers to submit an SBR on a modified original bill, we highly recommend submitting on the SBR-1 form, found here.
What Are the Most Useful Tips for Filling out an SBR?
- SBRs can’t have any new dates of service or additional billing codes that were not on the original bill.
- Only one SBR per single original bill--no combining multiple bills in a single SBR.
When Does a Claims Administrator Have to Respond to an SBR?
Claims administrators must respond with an SBR Explanation of Review (EOR) within 14 calendar days.
What’s Next If the SBR Is Not Successful?
If the SBR isn’t resolved satisfactorily, a provider has three potential courses of action:
- File an Independent Bill Review--but only after receiving the EOR for the SBR.
- File a lien if the claims administrator breached its duty to the provider. Examples of breach of duty include failure to respond to the SBR and failure to send an EOR.
- File an audit complaint* if the claims administrator demonstrates a pattern of bad behavior. Although the particular bill will not be investigated, this process alerts the Department of Workers’ Compensation that a claims administrator may not be following the rules.
Watch daisyBill's free webinar for more info on SBRs!
*NOTE: The Audit Complaint form was updated in 2019. Access the updated form here: https://www.dir.ca.gov/dwc/Auditref.pdf
VIDEO AND SLIDES
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.