CorVel Adjuster & Attorney Ignore CA Law (Part 1)
Getting paid for treating injured workers can be highly challenging for providers. And sometimes, claims administrators and their representatives can be just plain mean.
The email exchanges published below are between CorVel, a Third-Party Administrator (TPA), and a provider seeking payment for treatment that CorVel authorized. These emails exemplify one of the many reasons providers avoid treating injured workers.
After reading this series, you should wonder why any California provider agrees to endure this kind of abuse.
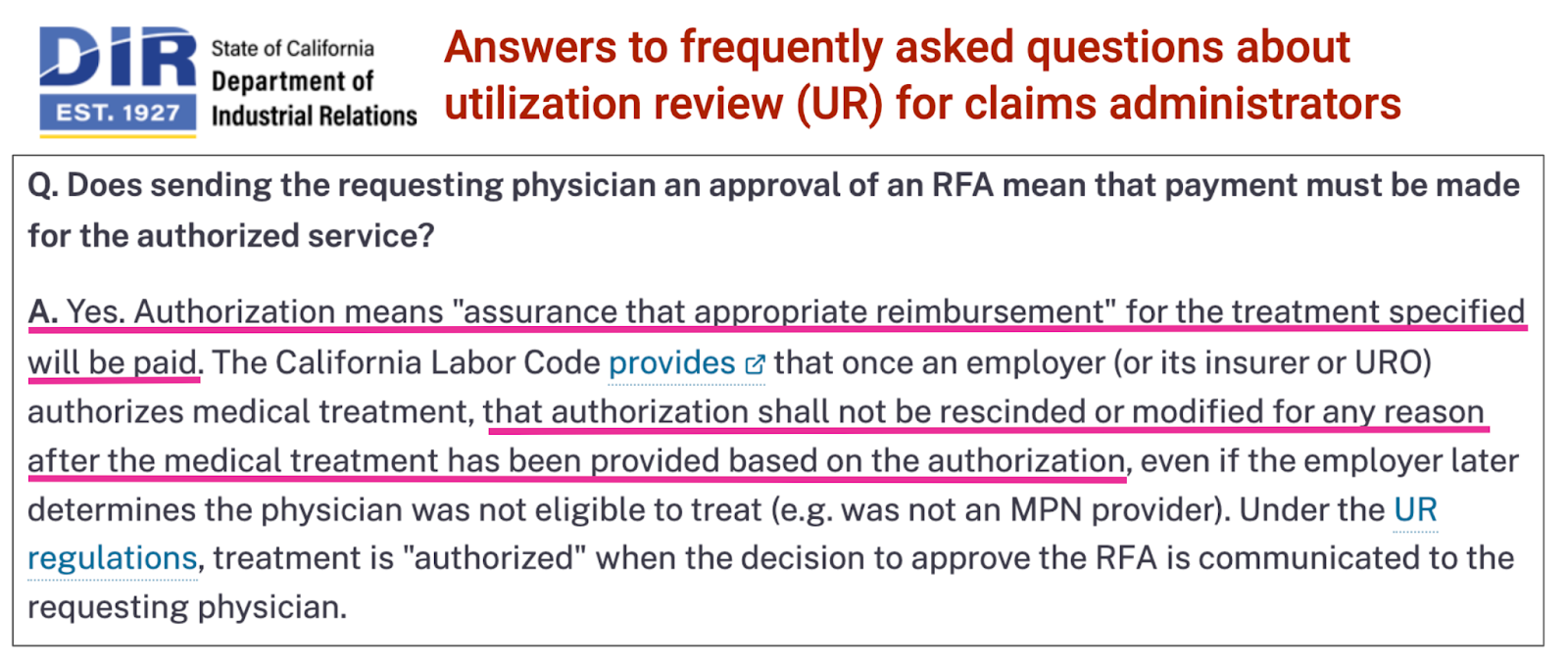
CA Law: Authorization Is Guarantee of Payment
On its FAQ web page*, the California Division of Workers’ Compensation (DWC) couldn’t be more precise: sending a requesting physician approval of an RFA means that (Yes.) payment must be made for the services rendered.
As the DWC states, “authorization shall not be rescinded or modified for any reason after the medical treatment has been provided based on the authorization.”
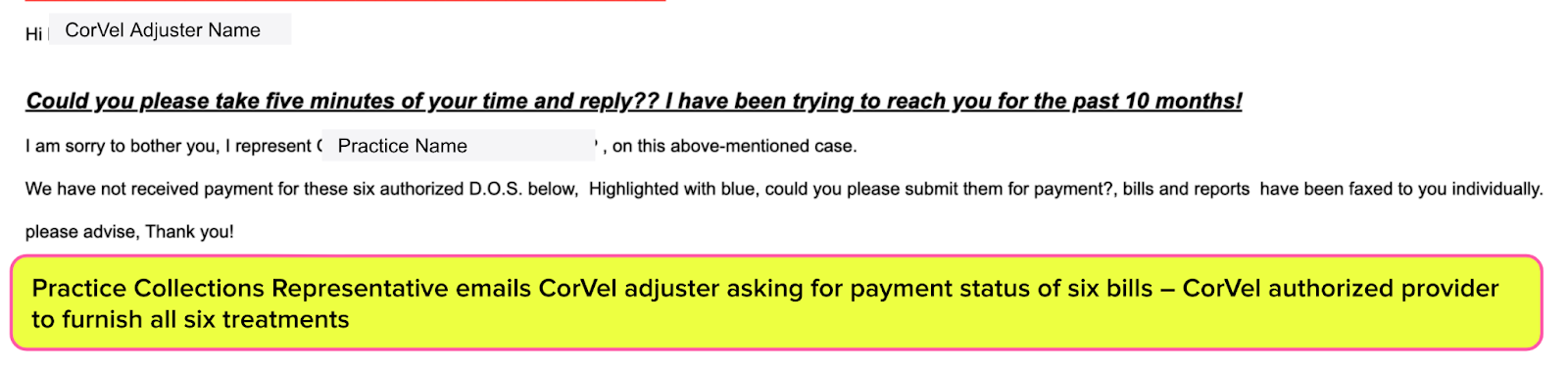
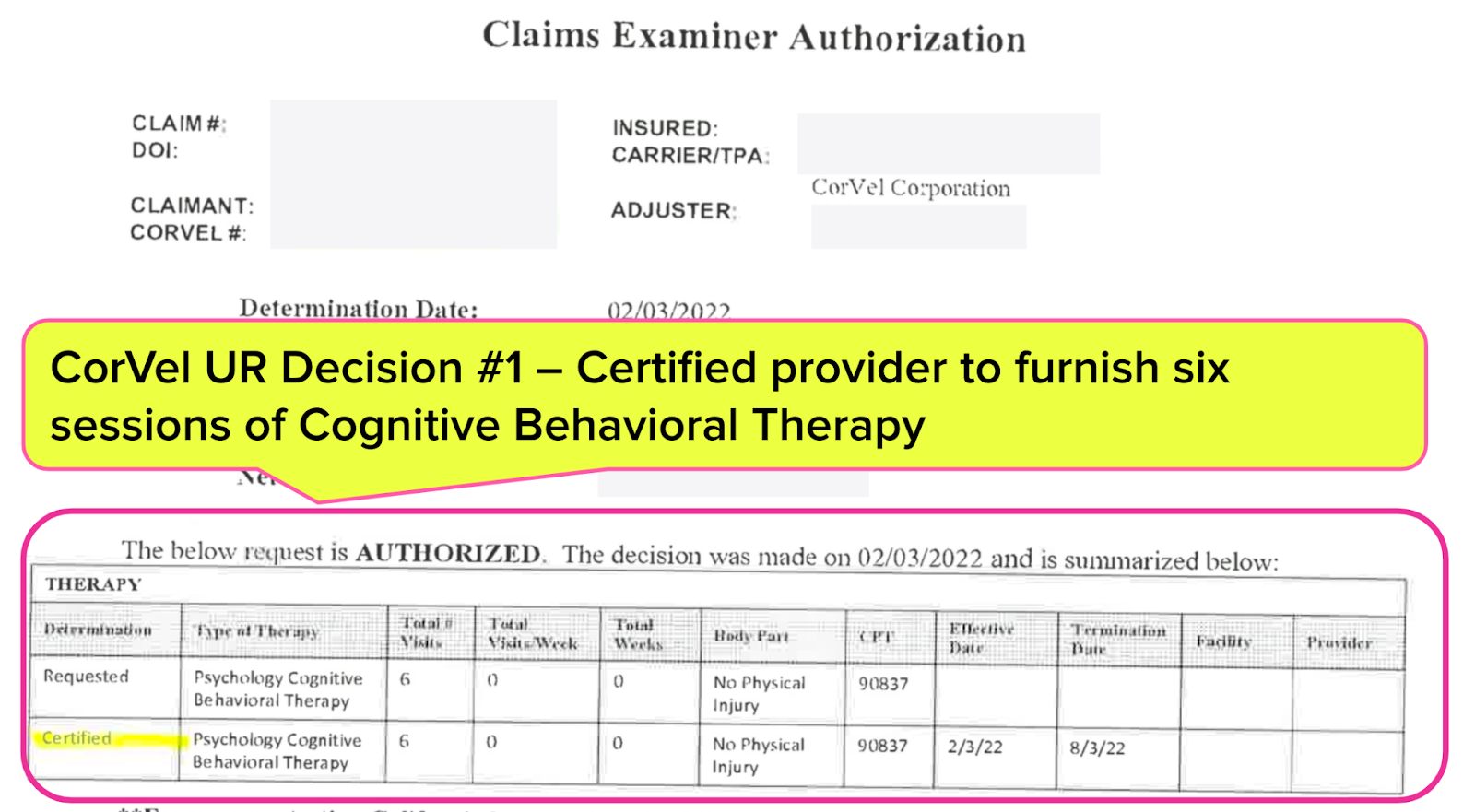
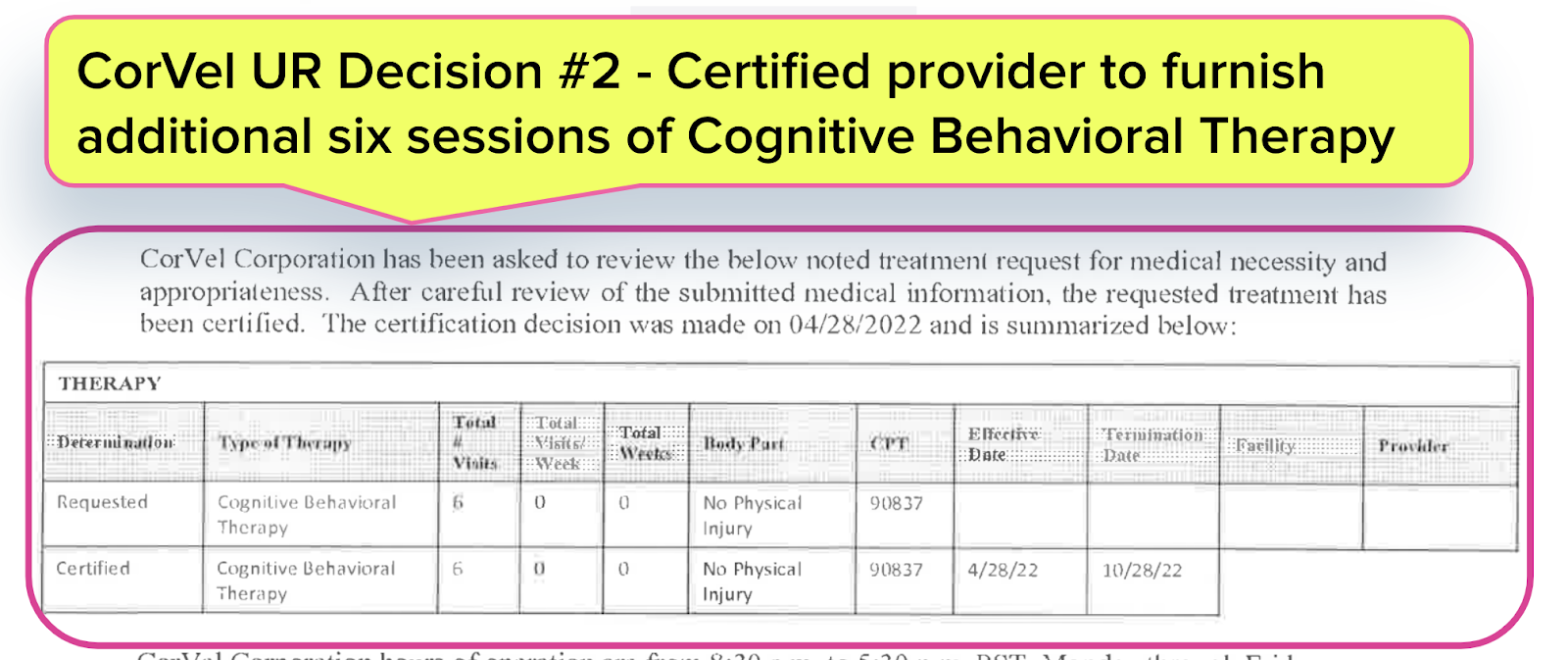
Armed with the legal fact that authorization is a guarantee of payment (and after several previous attempts to resolve the issue), a practice’s Collections Representative sent CorVel an email requesting payment for six bills for Cognitive Behavioral Therapy — treatments that CorVel authorized the practice to furnish to the injured worker.
CorVel Email #1: Senior WC Specialist to Practice - Buzz Off
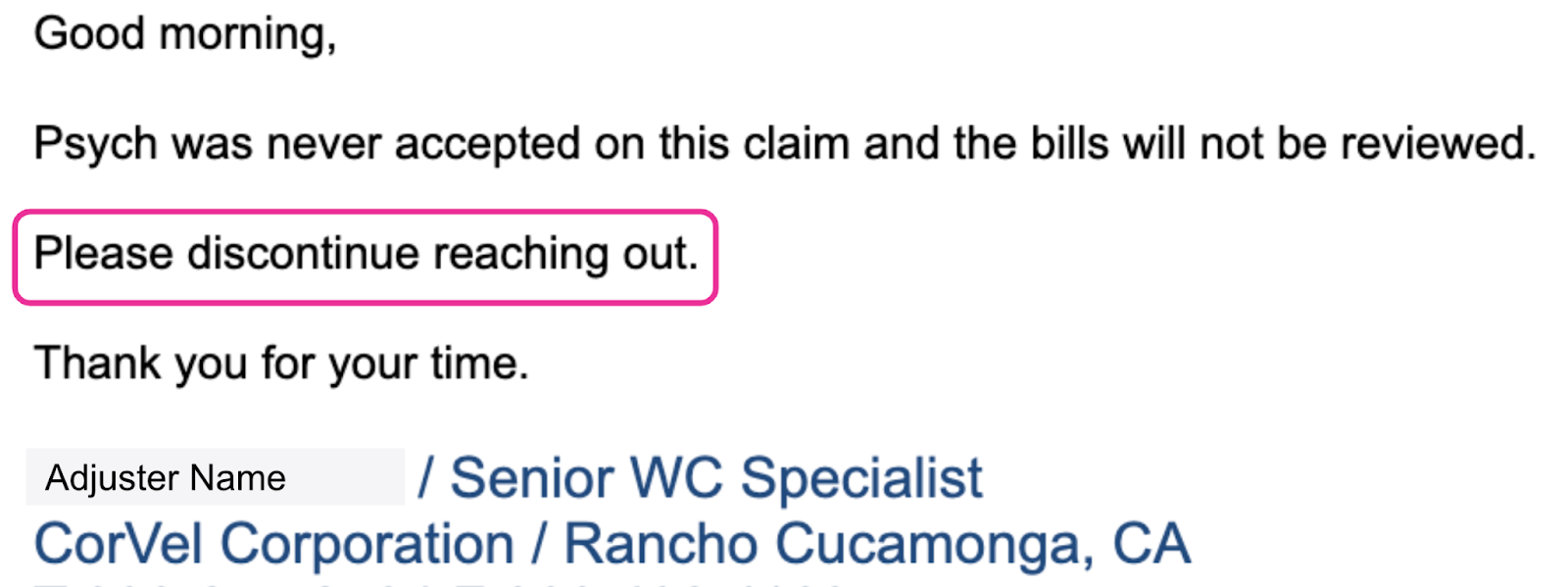
The adjuster, a CorVel “Senior WC Specialist,” responded to the practice’s inquiry by explaining that “the bills will not be reviewed” (despite CorVel authorizing the treatment) because “psych was never accepted on this claim.”
The Senior Specialist also instructed the practice’s representative to “discontinue reaching out” to CorVel.
Below is CorVel’s email response to the Collections Representative, followed by two Utilization Review (UR) decisions that CorVel had sent to the practice certifying (aka authorizing) the treatments in question.
CorVel Email #2: Orthopedic Gibberish
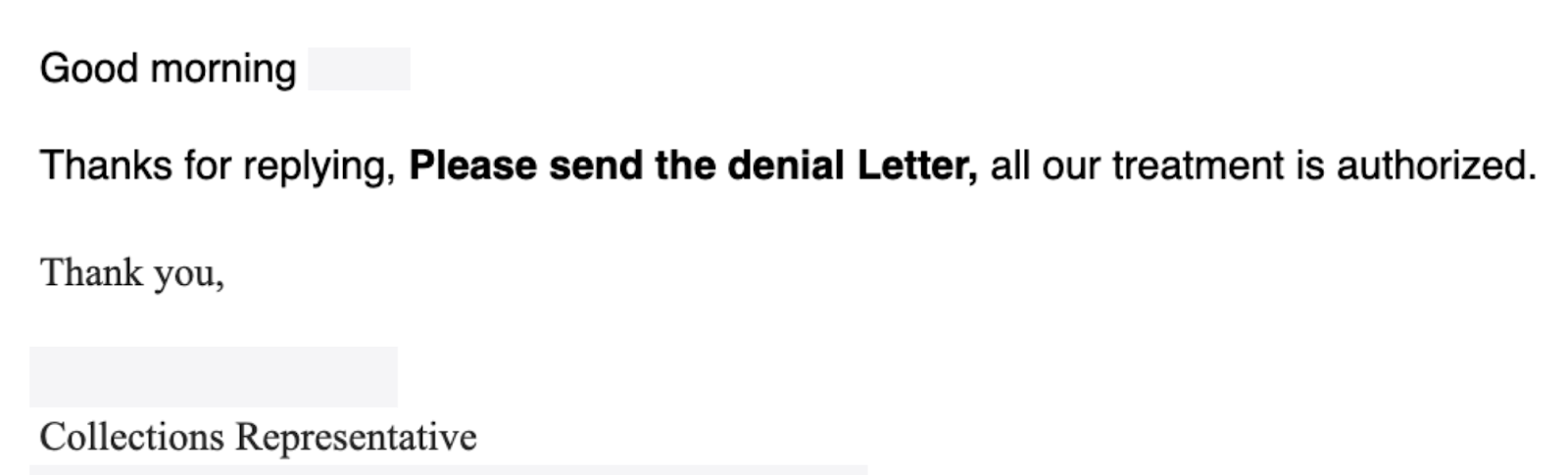
Ignoring the instructions to “discontinue reaching out,” the practice’s Collections Representative sent a follow-up email thanking the Corvel Senior Specialist and asking them to “Please send the denial letter.”
The Collections Representative reiterated that CorVel authorized the practice to provide the treatment.
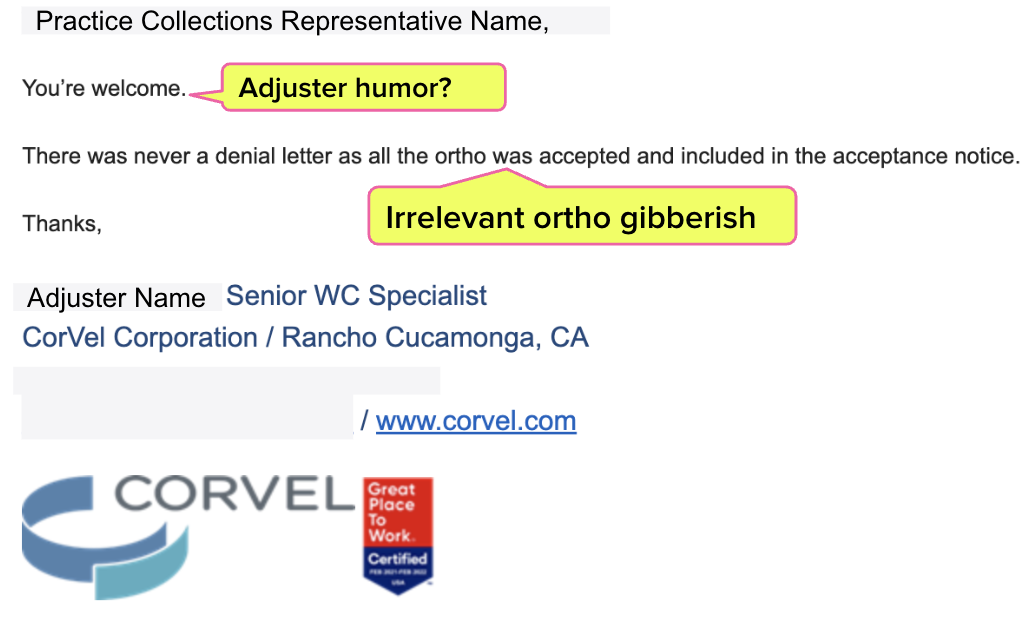
The CorVel Senior Specialist replied to the Collections Representative with some irrelevant gibberish about orthopedic treatment being the reason CorVel refused to discuss payment for the authorized psych treatment.
CorVel Email #3: A Grim Exchange
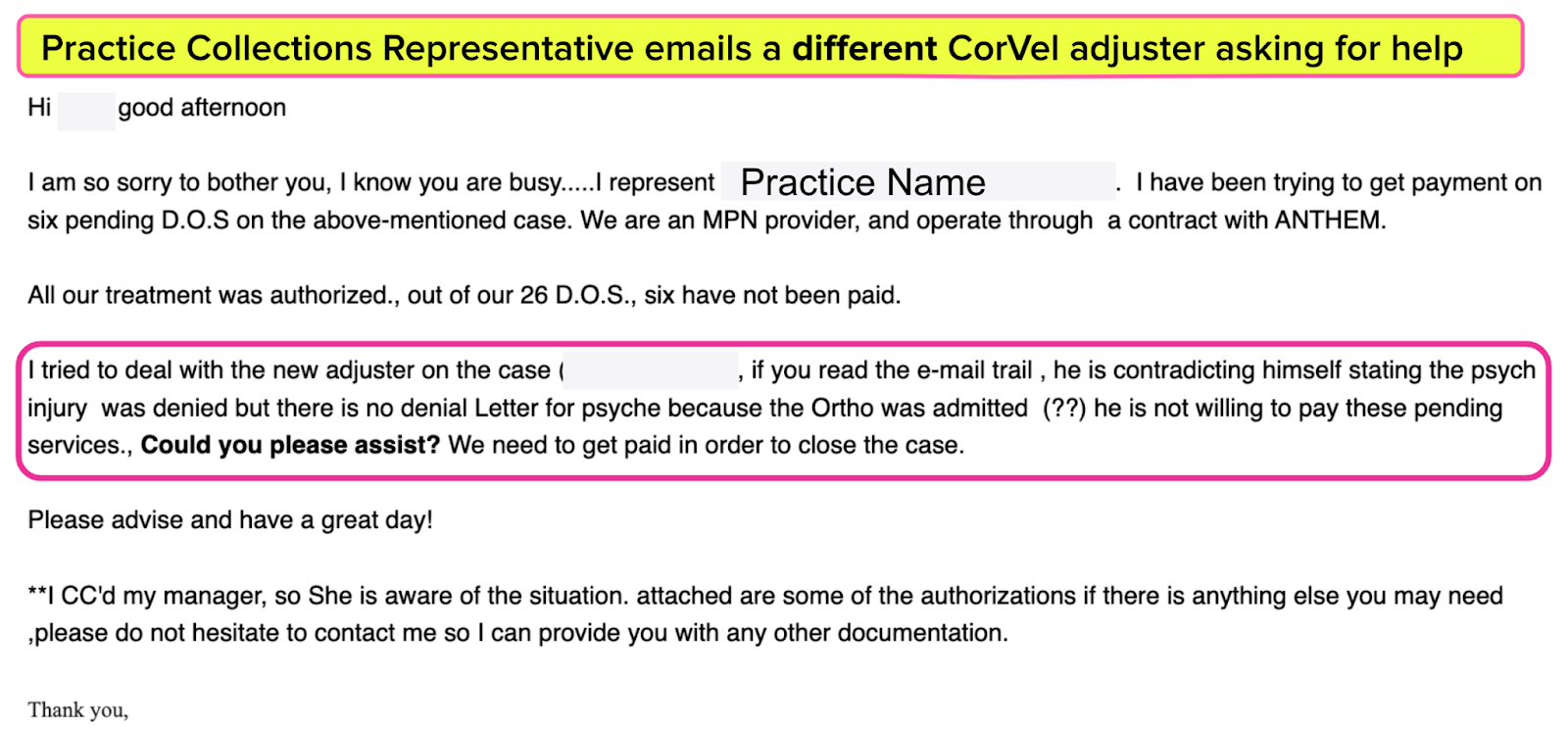
Having failed to make progress with the Senior Specialist, the Collections Representative emailed a different CorVel adjuster, asking for this second adjuster’s assistance in obtaining payment for the six bills.
Then, things got…weird (but not as weird as they would get).
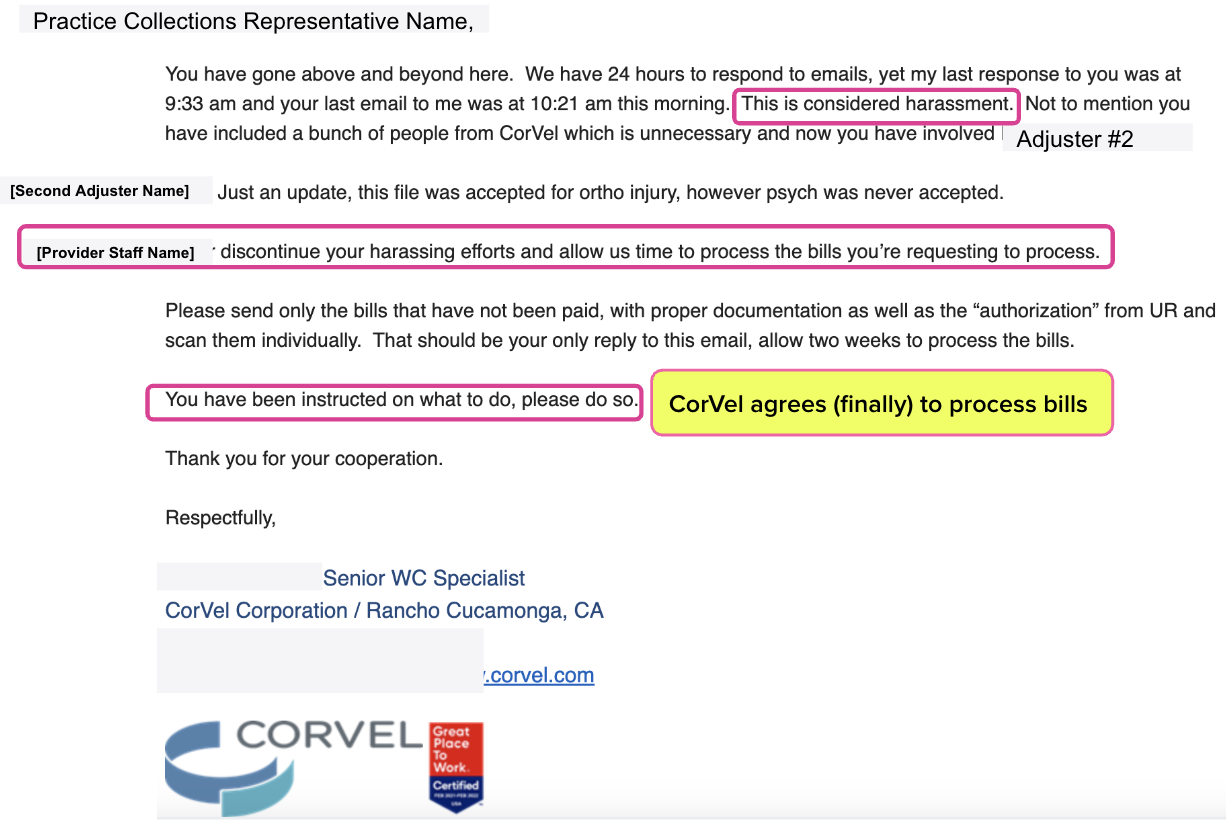
The first CorVel adjuster responded to the Collections Representative’s message to the second CorVel adjuster with an emotional rant, repeatedly accusing the provider’s representative of “harassment.”
However, the Senior Specialist finally agreed to “process the bills” and instructed the practice to resubmit the bills and the UR decisions authorizing the treatment.
CorVel’s responses to the practice’s reasonable inquiries were rude and unprofessional. But somehow, subsequent emails to the practice from CorVel’s defense attorney are even more unhinged and nonsensical.
Continue to Part 2 of this story to see how this TPA escalated the abuse.
*The DWC FAQ, a screenshot of which from December 2023 was included in this article, has been removed from the DWC website as of its most recent update in January. The answer to the question, however, remains the same.
We make treating injured workers easier, faster, and less costly. Request a free demonstration below.
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.




It's becoming more and more frequent. This is again why we are selective with the carriers we treat.
It's terrible that they're allowed to get away with this. I've had my share of grief with "Cor-Hell".
Wonder what the outcome might have been if CareMC Edge had provided he same services? What a wonderful dynamic for a CONFLICT OF INTERESTS when you can: refer to your own subsidiary, create invoices to bill your parent company, review the invoices in your own Medical Bill Review software, and then pay yourself all with the clients' money.
https://www.corvel.com/services/