Confusion and Running in Circles: AIG / MedRisk Incorrect Denials

Recently DaisyBIll providers reported receiving incorrect and very confusing denials from MedRisk, a managed care provider network, for bills that were actually submitted directly to AIG. The MedRisk denials state: “Not currently a participating MedRisk provider. Please submit bill directly to insurance carrier.”
But in every reported incident, the providers had submitted the denied bills directly to AIG, the correct carrier for the particular patient and injury.
So the providers are, understandably, confused by the denial from MedRisk. Welcome to the heinous, dark world of nightmarish workers’ comp networks. Without careful review of the network contract terms, here at DaisyBill we strongly advise providers against signing workers’ comp network contracts.
Need convincing that these network contracts are potentially awful and lousy for your bottom line (not to mention sanity)? Read the following real-life Denial Nightmare described in five painful steps.
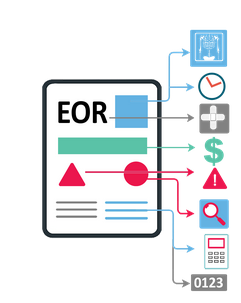
Upon receiving the incorrect MedRisk denial (“Not currently a participating MedRisk provider. Please submit bill directly to insurance carrier”) :
- The provider calls AIG about the incorrect denial from MedRisk, and the AIG representative insists that the provider sent the bill to MedRisk, when the provider KNOWS they did not send the bill to MedRisk.
- Fortunately, for an electronically submitted bill, the provider has documented proof the bill was correctly sent to AIG’s payer ID. Despite this irrefutable proof, the AIG representative relentlessly insists that the misdirected bill is due to provider’s error.
- Unfortunately, for a bill sent via mail, the provider usually has no proof substantiating the address on the bill’s envelope.
- Next the provider calls MedRisk, and after an extended amount of time on hold, the MedRisk representative confirms either:
- AIG did, in fact, send the bill to MedRisk, or
- AIG sent the bill to a related / affiliate MedRisk network (Stratose Network - now Zelis, Multiplan, etc.), with which the provider contracted, and the related / affiliate network sent the bill to MedRisk.
- BTW: MedRisk does not keep a record of the specific company that forwarded the bill to them.
- Once MedRisk receives a bill forwarded either directly or indirectly by AIG, MedRisk can either:
- Send the bill BACK to AIG for payment (believe-it-or not, no kidding!!!), or
- Deny the bill if the provider is not contracted with MedRisk with a denial reason: “Not currently a participating MedRisk provider. Please submit bill directly to insurance carrier.”
- Now, the circle of Denial Nightmare is complete. For an incorrectly denied bill, there is no way to get this bill processed. If the provider resubmits the bill, AIG will, once again, send the bill to either:
- MedRisk or
- The related / affiliate network (Stratose Network, Multiplan, etc.) with which the provider contracted.
- MedRisk will:
- Deny the bill if the provider is not contracted with MedRisk with the denial reason: “Not currently a participating MedRisk provider. Please submit bill directly to insurance carrier.”
DaisyBill clients often contact DaisyBill for assistance with the recurring Denial Nightmare described above, stating that they are not contracted with MedRisk. Inevitably, upon further investigation, it is determined the provider either signed a contract in the past with MedRisk or signed a contract with a MedRisk related or affiliate network.
Here is the worst part of the Denial Nightmare: by signing a managed care network contract, providers abdicate their rights to combat this surreal situation, because these networks are not regulated by California’s Division of Workers’ Compensation (DWC). Once a provider signs a network contract, the claims administrators that use the networks are no longer obligated to abide by the DWC regulations put in place to protect providers.
Again, we strongly advise providers not to sign network contracts. If a provider opts to sign a network contract, carefully review the terms of the contract. Often the terms allow the network to sell / share signed contracts with other networks and multiple claims administrators. Accordingly, a single signed contract may obligate a provider to many claims administrators and other undisclosed networks.
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.