Anthem's THM Network Closes, Stiffs Providers
Workers’ comp providers—in particular ancillary providers like physical therapists (PTs)—take note: if you have treated injured workers through Anthem’s Transparent Health Market (THM), you may need to take action to receive payment.
Anthem’s THM recently closed its doors. However, physical therapy providers report this network did not forward payment owed to providers despite receiving payment from claims administrators before shuttering.
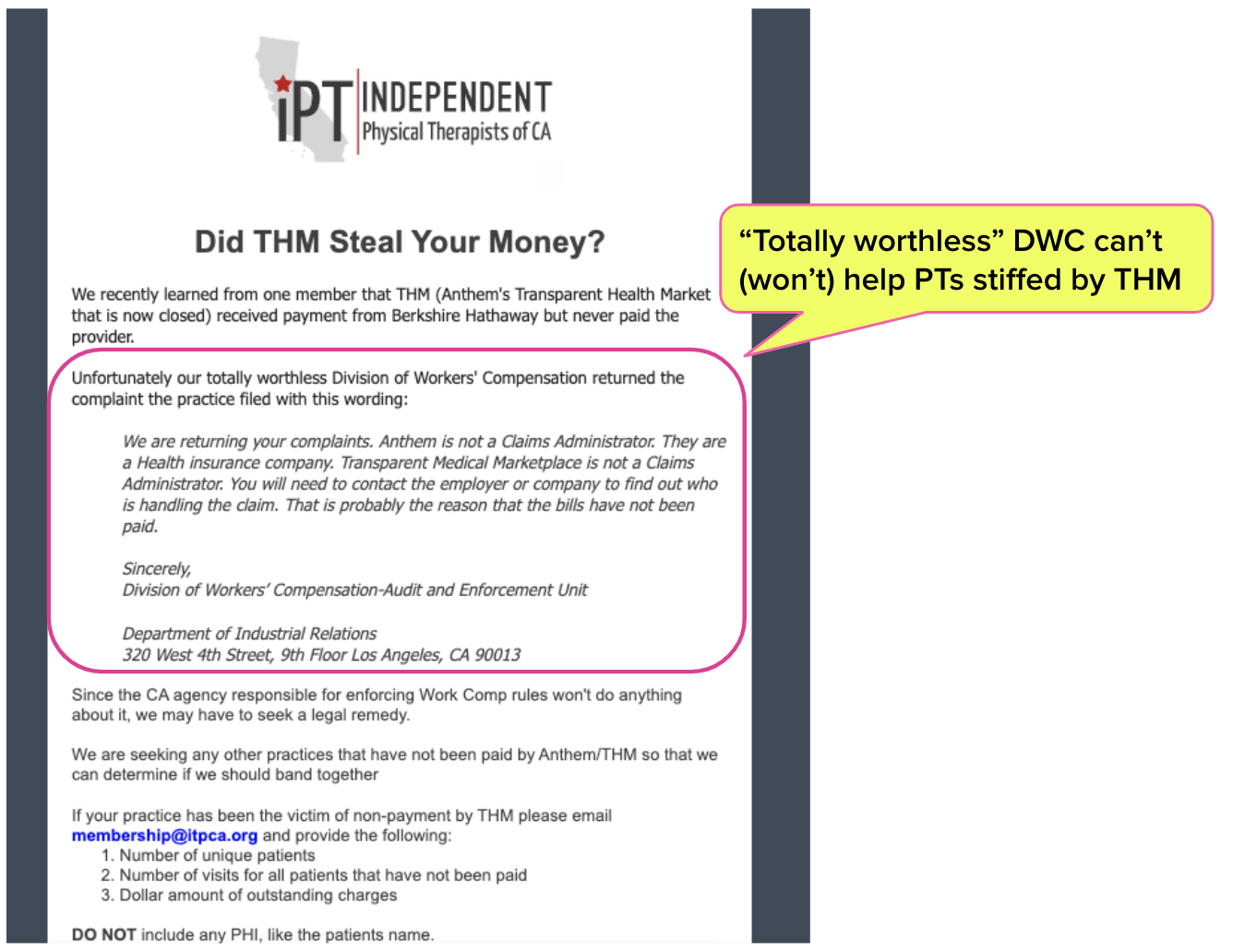
Also, according to the Independent Physical Therapists of California, in an infuriatingly on-brand move, California’s Division of Workers’ Compensation (DWC) declined to provide help or guidance to physical therapist providers who did not receive payments owed from THM.
daisyBill did some daisyDigging and discovered an avenue these providers can use to seek payment. See how to proceed below.
THM Stiffs PTs, DWC Shrugs
Independent Physical Therapists of California (iPTCA) recently shared with its members that Anthem’s THM:
- Went out of business
- Received payment from from at least one claims administrator, Berkshire Hathaway, for physical therapist bills THM submitted
- Failed to pay the physical therapists despite having received the funds
Moreover, when an iPTCA member filed a complaint with the DWC, the DWC returned the complaint with an explanation that since neither Anthem nor THM are workers’ comp claims administrators, the DWC is powerless to intervene (or, in iPTCA’s words, “totally worthless”).
The message from iPTCA is below.
To daisyBill’s knowledge, before its closing, THM submitted providers’ bills to at least the following three claims administrators:
- Berkshire Hathaway Homestate Companies
- Cannon Cochran Management Services, Inc.
- Employers Compensation Insurance Company
How to Seek Payment for THM Bills
While iPTCA contemplates some kind of collective legal action, daisyDigging discovered that there is one avenue to pursue payment for unpaid THM bills. Providers are advised to resubmit their unpaid bills to ‘THM dba Opyn Health’ at the address below:
Lou DiGiovine, CPA
SVP, Finance and CFO
Opyn Health, Inc.
1950 Butler Pike, #267, Conshohocken, PA 19428-1202
o: (484) 423-4421 f: (484) 727-9404
While daisyBill is trying to help providers receive payment for treating injured workers, we cannot guarantee that THM/Opyn will pay the physical therapists’ outstanding bills. However, we will continue to cover this story to alert the workers’ comp community to the outcome of Anthem’s Transparent (ha!) Health Marketplace's actions.
Networks: Look Before You Leap
When providers submit bills to networks rather than directly to claims administrators, depending on the state, there can be two distinct—and potentially costly—disadvantages:
- The network takes a cut of the reimbursement issued by the claims administrator in exchange for scheduling appointments and any other services offered before forwarding the provider the remaining scraps.
- The provider loses all rights to timely and correct payment at fee schedule rates. Additionally, in states like California, the provider also loses the right to appeal through the state-mandated fee schedule review processes. When it comes to reimbursement, you are at the mercy of the network.
For ancillary providers, PTs in particular, networks have driven reimbursement into the gutter by leveraging the Medical Provider Network (MPN) system. Under current law, MPNs may list networks like THM rather than individual providers, giving the networks near-total control over which providers can treat injured workers.
Take note: in some states the regulatory agencies have no regulatory authority over networks, leaving network-bound providers defenseless against abuse.
Think twice about the network game, especially if you provide ancillary services like physical therapy.
Edited July 10, 2024 for clarity.
daisyBill makes treating injured workers easier, faster, and less costly. Request a free demonstration below.
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.

.gif)
