CA State Fund: Superior Virtual Technology

Annually, daisyBill sends over 150,000 e-bills to the California State Compensation Insurance Fund (CA State Fund), a non-profit insurer that is practically perfect at e-billing.
State Fund’s near perfection in paying its bills is clearly a consequence of its leadership.
In addition to being a star at e-billing compliance (and responding decisively to resolve the inevitable occasional glitches), the insurer also excels in another particular area of technology that makes treating injured workers infinitely easier for providers (other claims administrators should take note).
CA State Fund’s advanced, fully automated Virtual Assistant technology is glorious. This technology makes it incredibly fast and easy for providers to investigate claims and bill statuses with minimal friction, any time of day or night, without even picking up the phone.
Quantifying the time and administrative resources that State Fund’s Virtual Assistant saves California providers is almost impossible.
Providers’ administrative staff do not need to spend inordinate amounts of time on hold with the CA State Fund to chase down adjusters, RFA fax numbers, claims information, billing details, or missing payments.
See how CA State Fund’s brilliant technology works below—and why it compels us to tip our hats to a fellow innovator who makes treating injured workers easier for providers.
CA State Fund: A Chatbot Worth Talking to
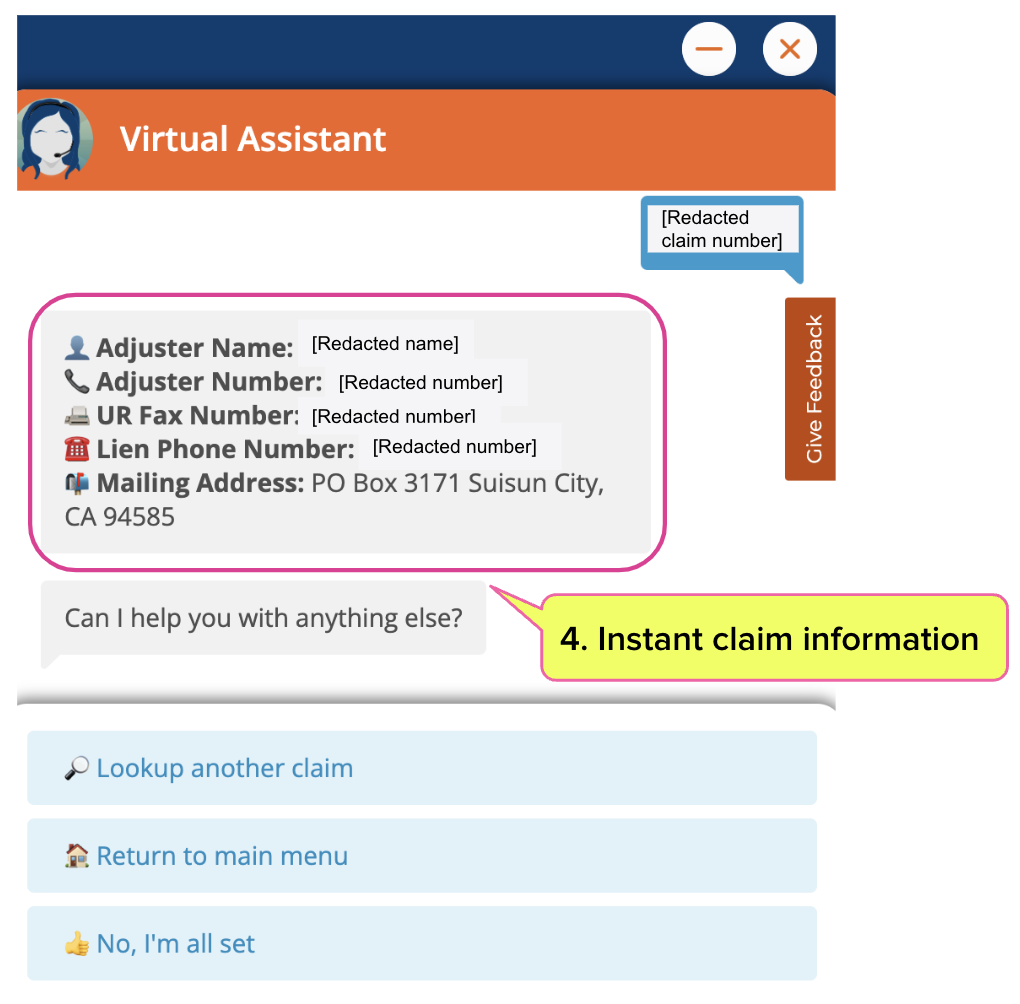
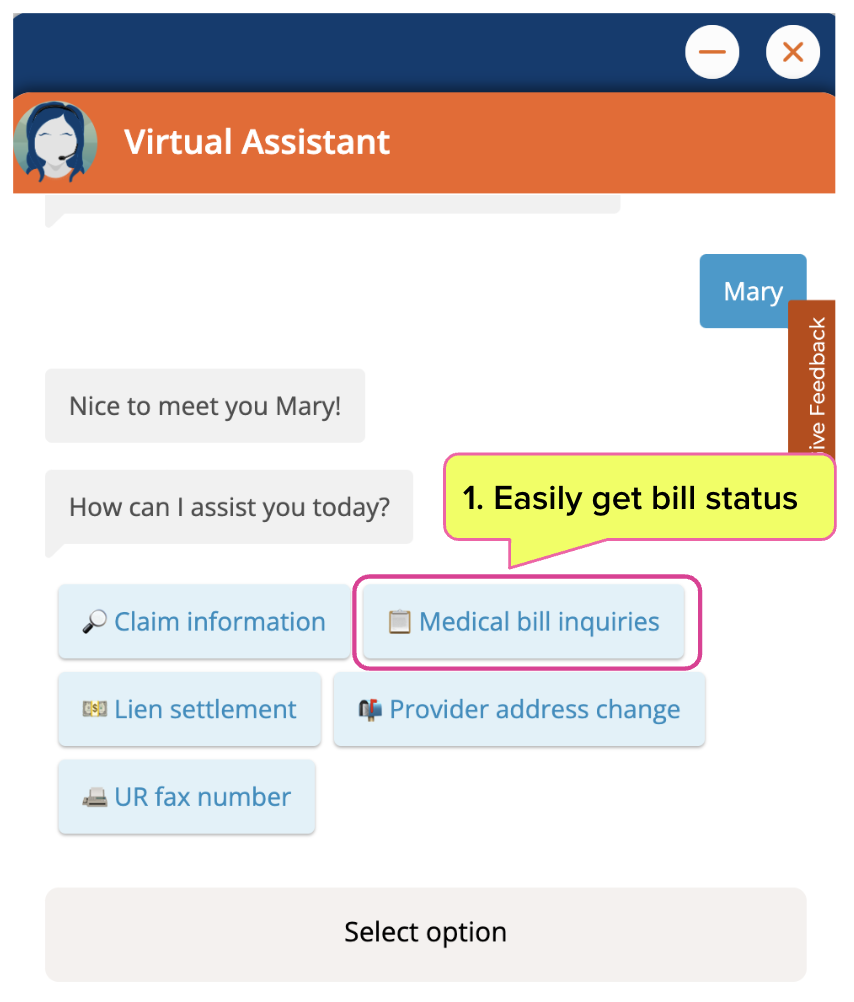
With CA State Fund’s Virtual Assistant, provider staff can get claims information, make bill inquiries, get information about Utilization Review (UR), and more—all in a fraction of the time it usually takes staff to climb around phone trees with other claims administrators.
CA State Fund’s competent and friendly bot furnishes essential details with just a few completely automated steps, as shown below.
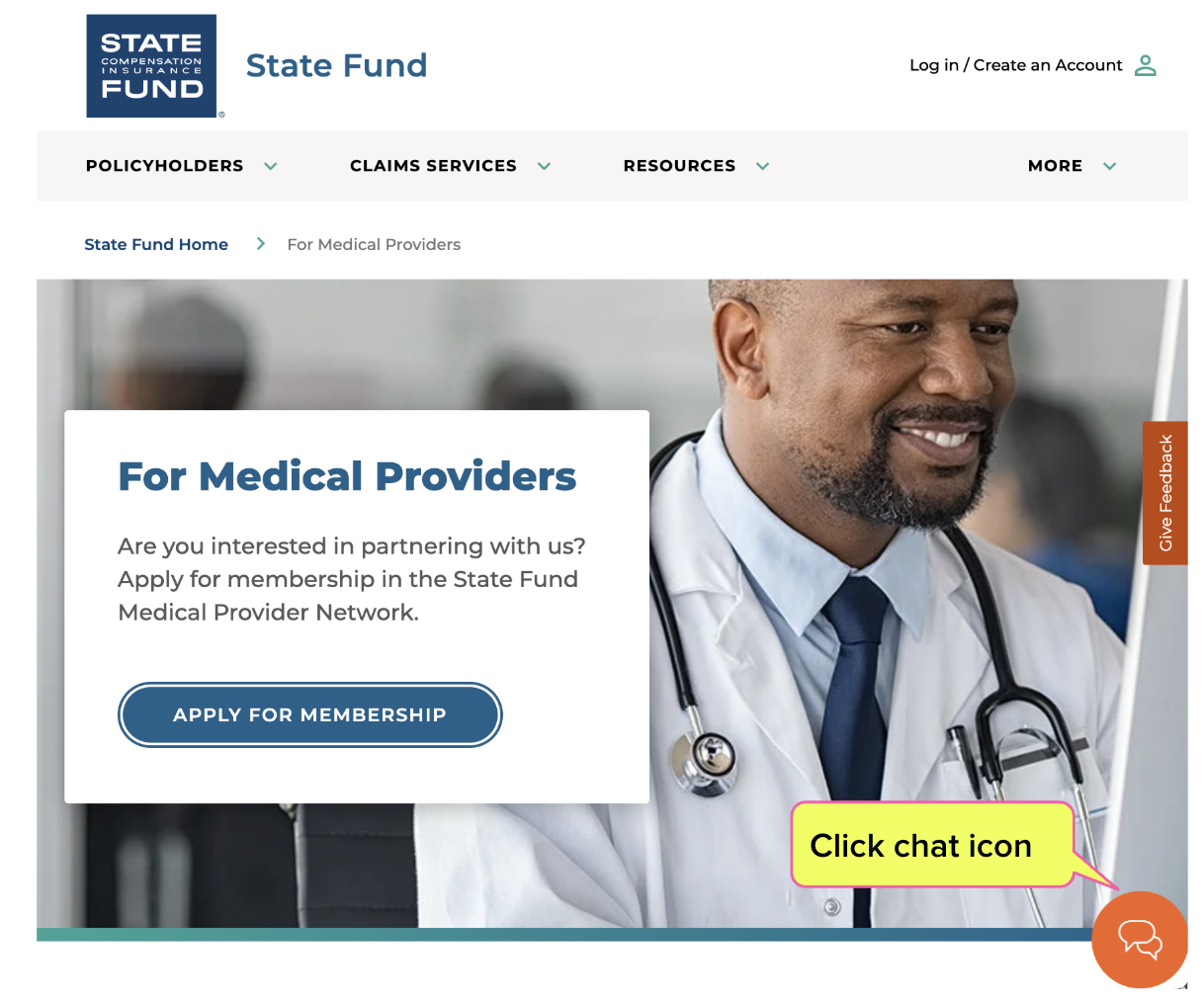
Providers begin by clicking the chat icon on State Fund’s “For Medical Providers” page.
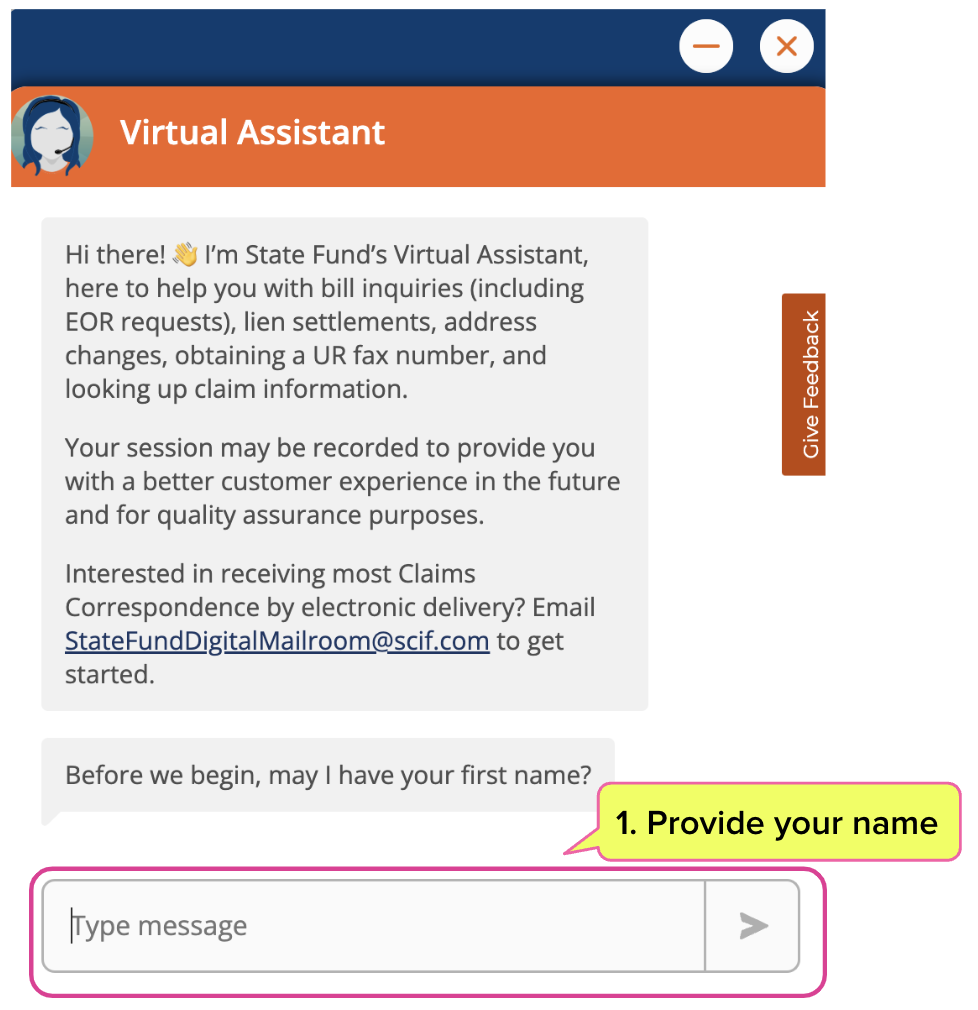
From there, a cheery but very informed Virtual Assistant introduces themselves and outlines the information they have—which is quite a lot. To get started, the provider or staff submits their first name.
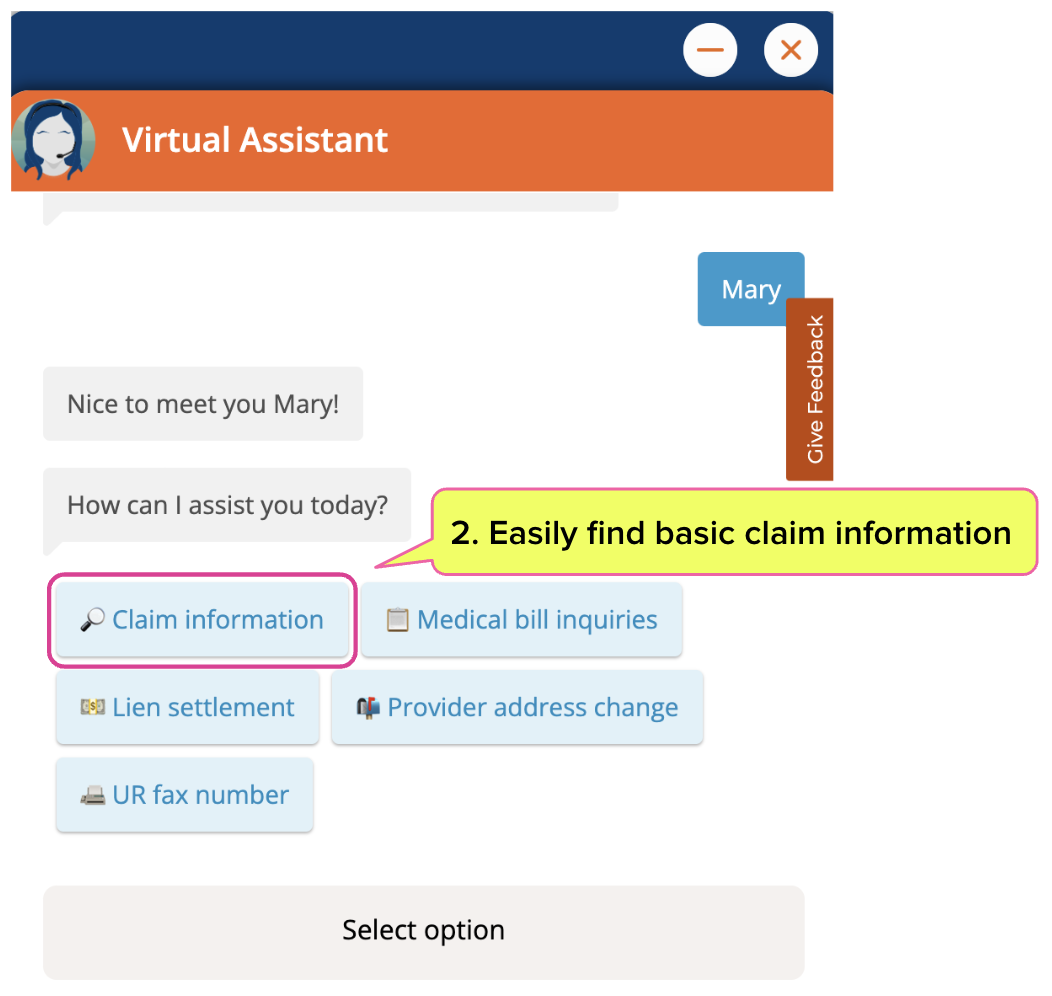
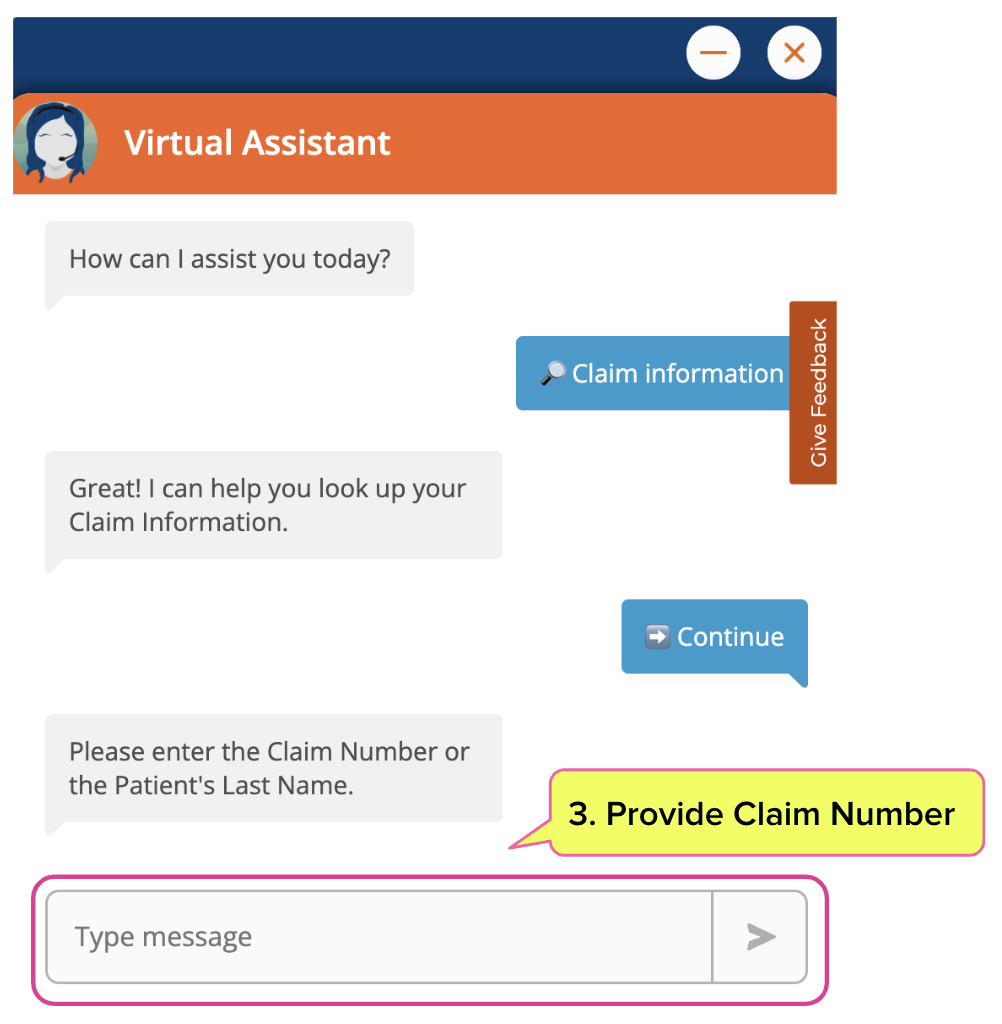
With the introductions complete, the Assistant offers five broad inquiry categories, including general claim information. Clicking “Claim information” prompts the Assistant to request the claim number.
As in the example below, entering a claim number prompts the Assistant to deliver every relevant piece of high-level information the provider needs to investigate further, from the claims adjuster’s name and contact information to UR fax numbers.
Finding Bill Information
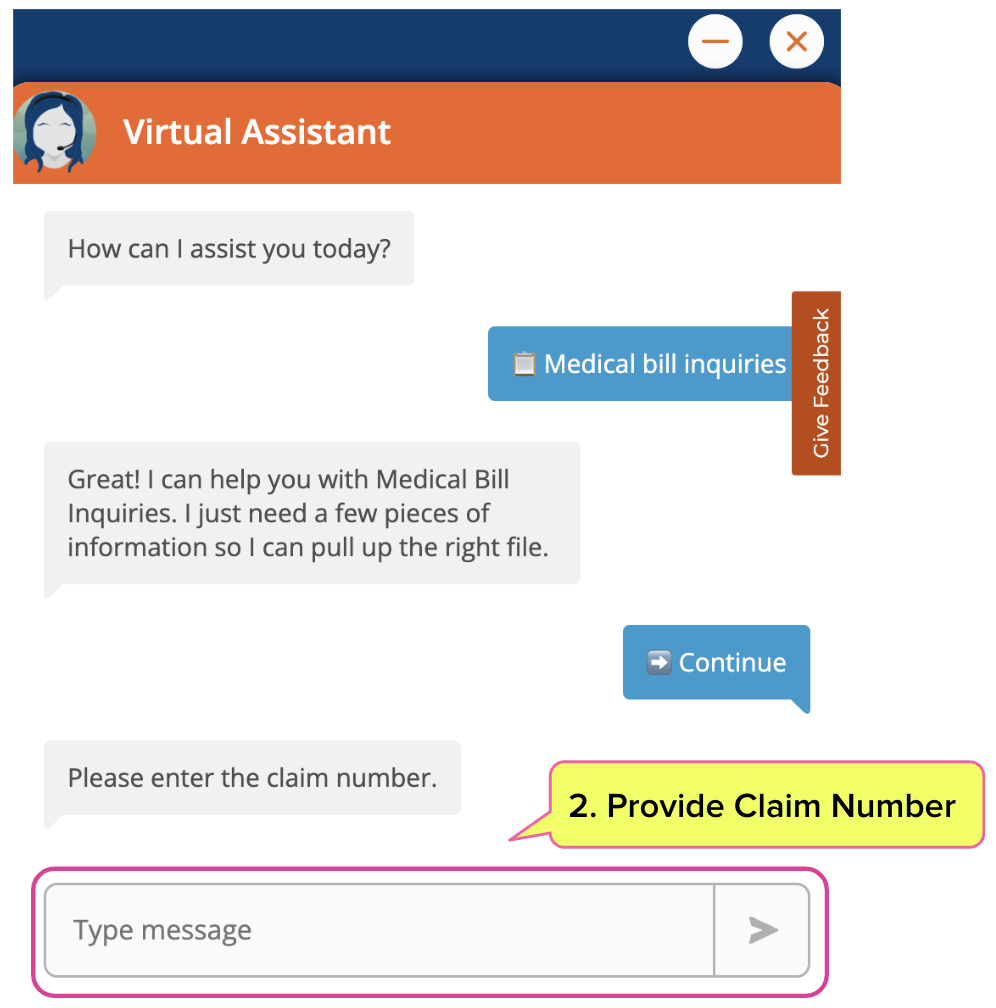
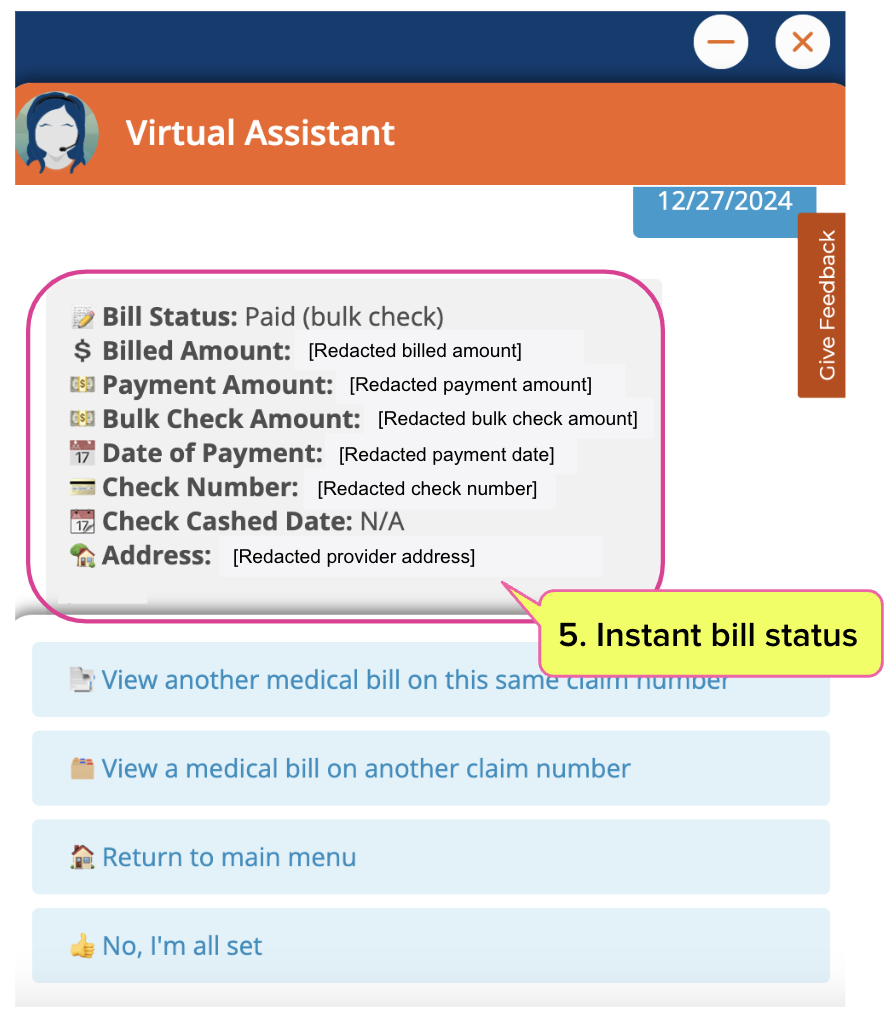
For complete information on a medical bill—the kind that can and does take hours to obtain from some claims administrators—the Assistant needs only a few more pieces of information, and the bill details are available immediately.
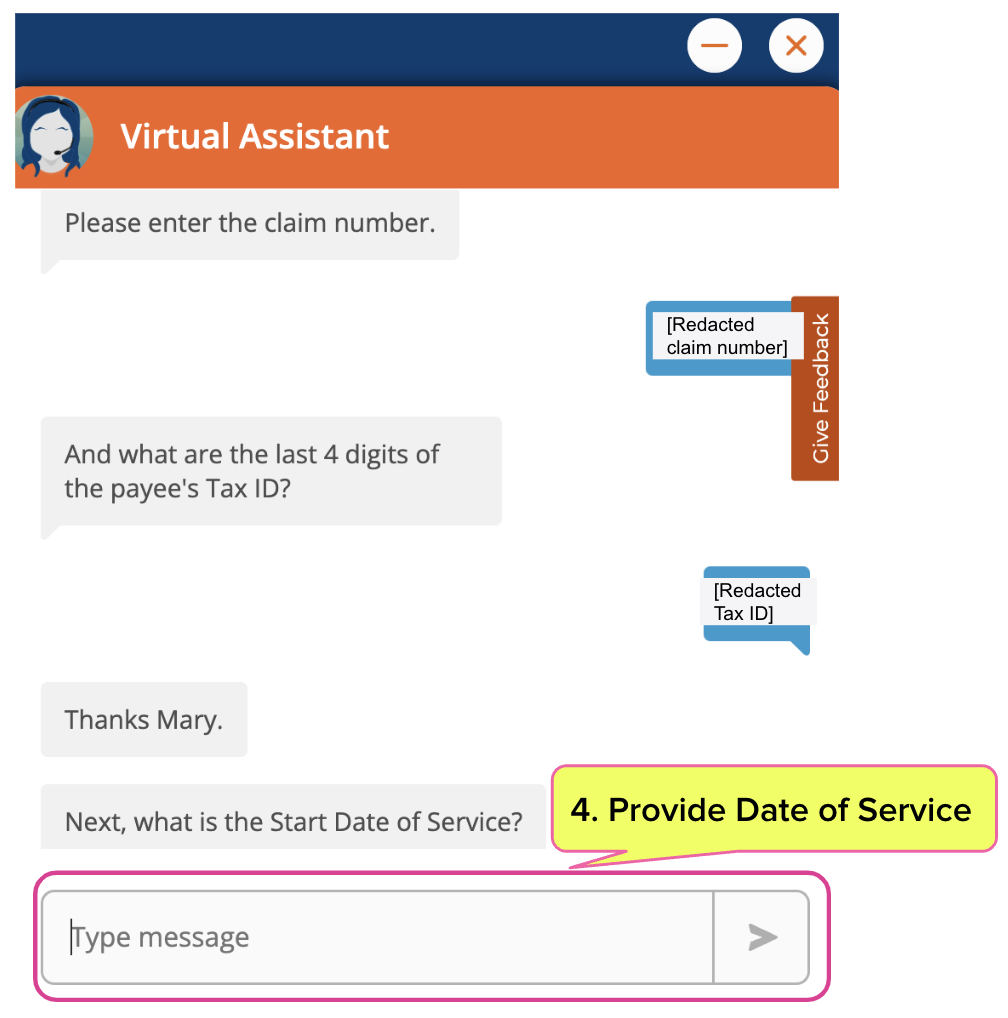
Once the provider selects “Medical bill inquires,” the Assistant asks for the claim number.
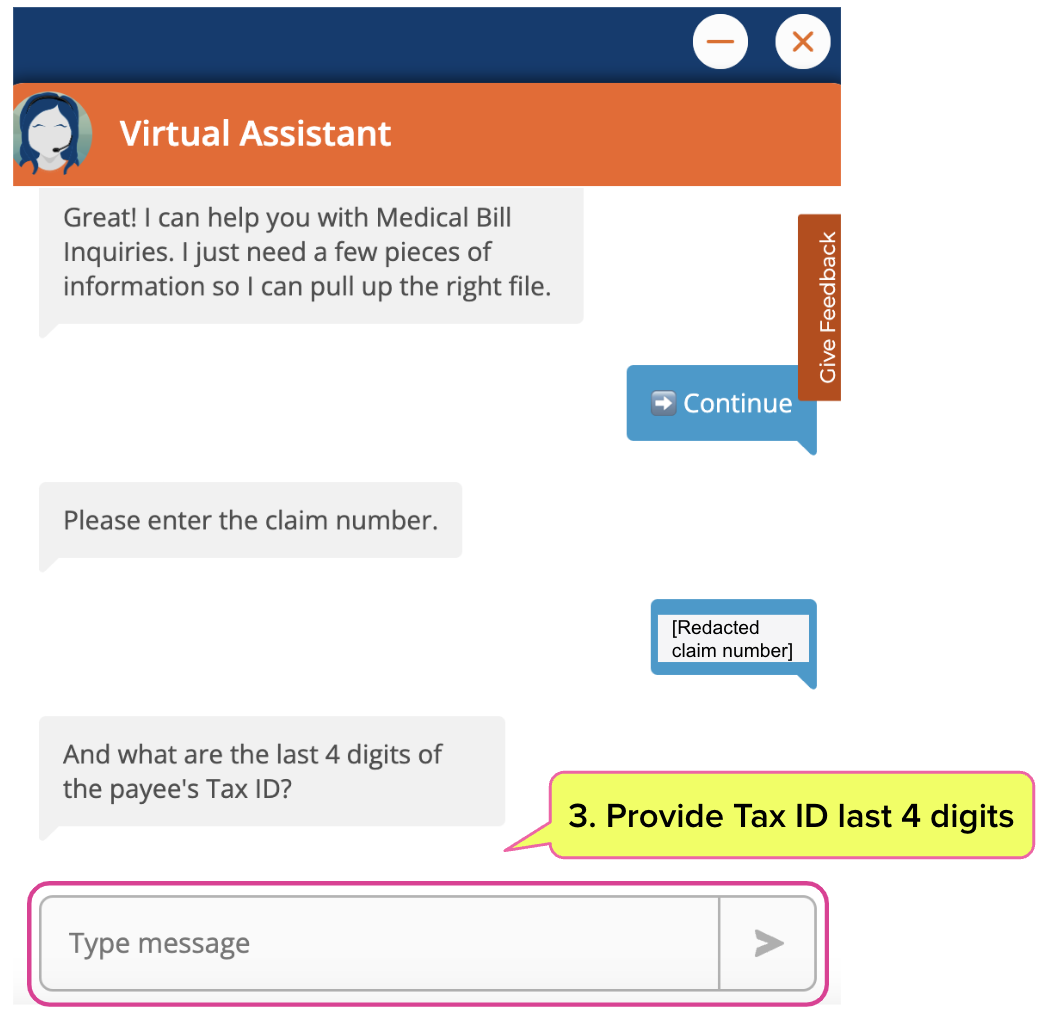
To access bill details, the Assistant requires only the last four digits of the provider’s Tax ID number and the Date of Service.
And just like that, the provider has all the relevant information on the bill status and payment details—from a process staff can complete in under a minute.
An efficient chatbot that helps providers find injury claim and bill information might seem like an extremely niche thing to gush about—even for workers’ comp tech nerds like us.
However, the critical fact is that every bit of technology that removes friction from the administrative side of workers’ comp helps injured workers.
Administrative friction is one of the primary factors driving providers away from treating injured workers. When a claims administrator tries to save doctors time and resources, the ultimate result is improved access to better care for people injured on the job.
Stay tuned for the next virtual assistant technology review. It’s not pretty.
Workers’ comp billing is different. Talk to daisyBill about making treating injured workers easier and less costly.
CONTACT US
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.