How It Works: Independent Bill Review (IBR)

Think about what workers' comp providers go through to obtain correct payment for treating injured workers. Compliant authorization and billing are taxing enough. Appealing incorrect reimbursements or denials with a request for Second Review means even more work. Then, when the Second Review appeal fails to produce proper compensation, the only recourse is to navigate yet another onerous process: Independent Bill Review (IBR).
Fortunately, the IBR process — though extremely burdensome — is navigable, and usually the provider prevails.
We’ve discussed the unholy hassle that is the Second Review process, with all its requirements. But when the insurer responds to a Second Review appeal without additional payment, it’s time to appeal to a higher authority. In this case, that higher authority is Maximus Federal Services, a private firm tasked by the Division of Workers' Compensation (DWC) with resolving payment disputes.
We here at daisyBill haven’t been shy in pointing out Maximus’ missteps. But the good news is that in about 75% of cases, Maximus rules in favor of the provider. Think about that: according to the state-sanctioned arbiter of all disputes, the provider is right the vast majority of the time.
The bad news? Requesting IBR requires extraordinary administrative time and resources, including a payment of $180.00 from the provider. As in the rest of workers' comp, the provider must fight and pay to obtain their due reimbursement.
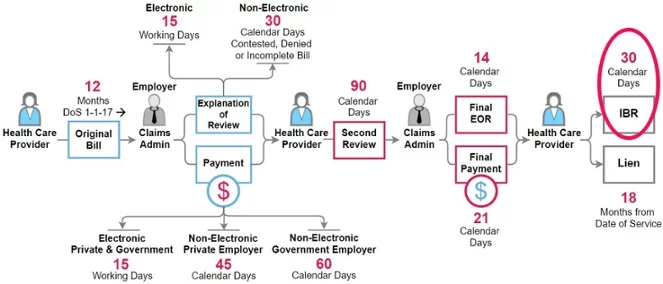
The IBR Process
The IBR process was one of the sweeping reforms brought on by the passage of Senate Bill 863. Before that, filing a lien was the only way to address a dispute. Because so many disputes are strictly about the amount owed (rather than more complex questions regarding compensability), SB 863 established the Second Review and IBR processes to resolve those differences more expediently.
The first step for providers is to make sure that the bill in question is eligible for IBR. Before requesting IBR, confirm the bill meets the following three requirements:
- The only issue in dispute is the amount of payment for services, not the compensability of the treatment.
- Reimbursement for the treatment in dispute is established in the Official Medical Fee Schedule (OMFS) or a separate reimbursement contract per Labor Code § 5307.11.
- A compliant request for Second Review was submitted. A bill is eligible for IBR only after Second Review.
Providers must submit the request for IBR according to (you guessed it) strict regulations. Failure to comply with any of the rules will result in (you guessed it again!) dismissal of the provider’s appeal. For Maximus to consider the bill in question, the provider must:
- Request IBR within 30 days from receipt of the final explanation of review (EOR) for the Second Review.
- Submit the request for IBR using the official form, DWC Form IBR-1.
- Include the final EOR from Second Review appeal, plus all other relevant documentation indexed and arranged as specified in the instructions that accompany DWC Form IBR-1.
- Submit a $180 processing fee, refundable only if Maximus rules in the provider’s favor (DWC Form IBR-1 incorrectly states the fee is $335; the DWC did not update the form to reflect recent changes).
- Concurrently send a copy of the IBR request and all supporting documents to the insurer’s claims administrator.
Providers can request IBR either electronically by registering with Maximus, or by mailing the request and its attendant documents to the address provided on the DWC IBR web page. For reference purposes, daisybill maintains a searchable database of all of the IBR decisions issued by Maximus,
The IBR process is a harrowing one, but the more providers insist on their right to just compensation — whatever it takes — the better off California workers' compensation will be. The lengths to which providers must go to obtain the reimbursement they’ve earned reflects a systemic bias against those who treat injured workers. That said, providers can (and should) fight back.
daisyBill’s Billing Software quickly completes the official DWC Form IBR-1, making request for IBR much easier. Our IBR tool automatically generates the required documentation, complete with instructions for assembling and submitting a complete IBR package to Maximus. Schedule a free demonstration, and see how daisyBill can help your office.
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.gif)