Providers, File Those Independent Bill Reviews (IBRs)!
Recently I heard Dr. Rupali Das speak at the CWC & Risk Conference--she’s the DWC Executive Medical Director. Her very interesting presentation started me thinking about workers’ compensation IBRs, along with Richard Boggan’s posts about the process.
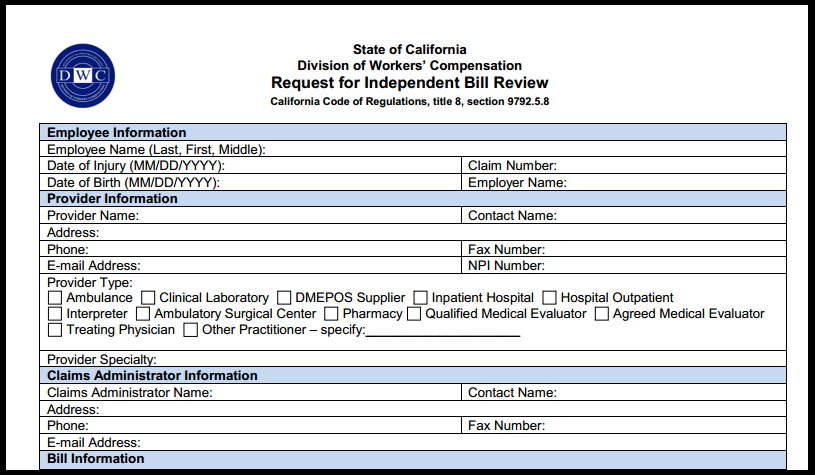
My understanding from Dr. Das’ presentation is that the DWC is encouraging providers to take advantage of the IBR process to resolve payment disputes. daisyBill agrees that the IBR process is under-utilized and we would like to see providers better use the IBR venue when their bills are incorrectly processed.
The IBR process is working better since its rocky start and cases have been making their way through Maximus at a steady clip.
Providers should realize what an incredibly powerful process IBRs can be, not only for getting paid for a particular bill but also for setting up a precedent for future bills. Again, I’ll point you to Richard Boggan’s informative writings.
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.