Submit Me Baby One More Time: Second Review Payment Data

Have you heard? We’re coming up on a major milestone. In a matter of days, daisyBill clients will reach $15,000,000 in additional revenue generated from Second Reviews (SBRs) alone. As more and more daisyBillers submit their bills for Second Review, we’re collectively clearing $1,000,000 every month in additional revenue.
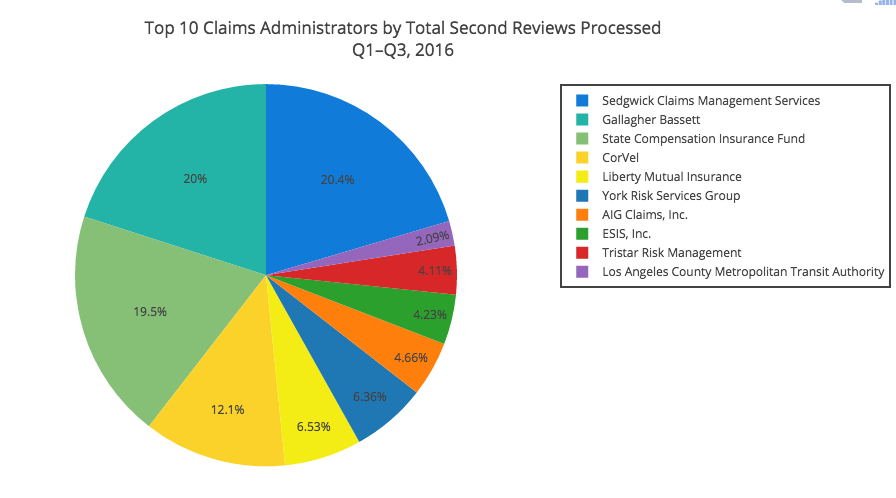
To celebrate reaching that nice, round number, we took a look at the top claims administrators by volume of electronic Second Reviews for medical treatment bills submitted in the first three quarters of 2016.
To no one’s surprise, there’s a lot of overlap with our top 20 claims administrators by volume.
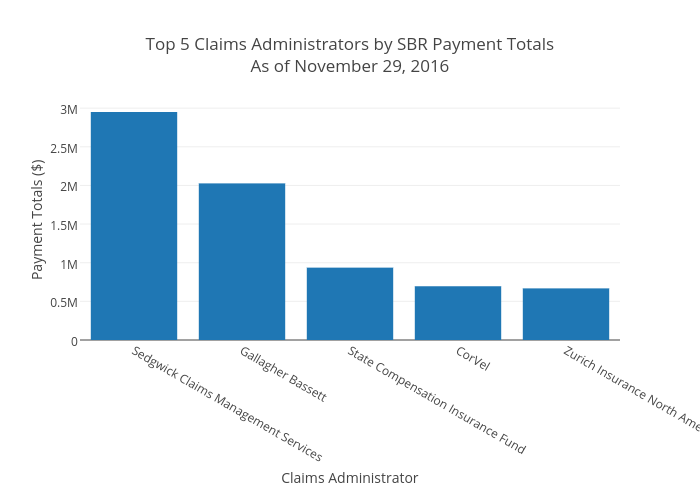
Sedgwick, Gallagher Bassett, and State Compensation Insurance Fund top the list. That’s to be expected – those three also lead the way in total original medical treatment bills submitted by daisyBillers. So it’s really no surprise that they lead the way in SBR payouts, too, with Corvel and Zurich Insurance North America rounding out the top five.
Bar Graph Payment Totals:
Combined, these five claims administrators paid $7.2 Million in Second Review payments – almost half of the $15,000,000 total for all claims administrators.
Remember, you can monitor all of this data on your daisyBill dashboard. Every time you log into your account, we display updated Second Review payment totals specific to your account, as well as a snapshot of payment totals across all daisyBill accounts.
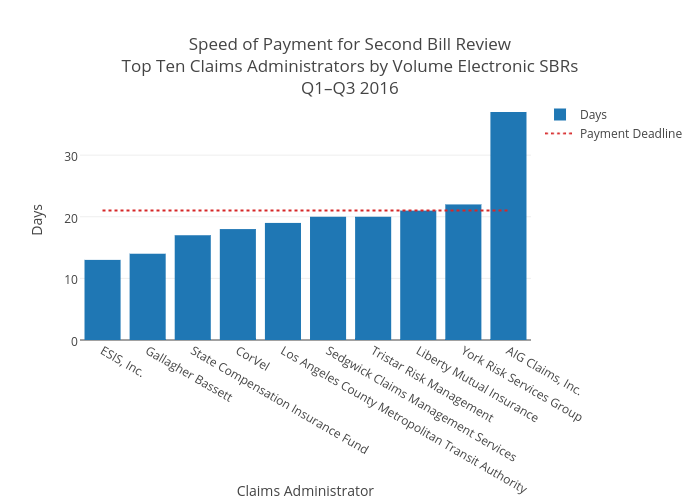
There’s one thing that your dashboard doesn’t show you, though – speed. We tracked average days to payment for electronic Second Reviews for the top ten claims administrators above. This is where things get interesting.
Remember, per Labor Code 4603.2. (e)(3), an EOR is due “within 14 days of a request for second review,” while payment “shall be made within 21 days of receipt of the request for second review.”[1]
Usually, payment is sent with the EOR, rather than separately. We’ll give our claims administrators the benefit of the doubt, though, and assume that they’re using that seven-day cushion before remitting payment. By this measure, ESIS, Inc. and Gallagher Bassett are pretty speedy. On the other end of the spectrum, we have York Risk Services Group and AIG Claims, Inc. While York misses compliance by just one day, AIG Claims, Inc. languishes far behind with an average of 37 days to payment – that’s slower than ESIS and Gallagher Bassett combined.
Check back soon for a fascinating examination of the number of Second Reviews upheld and overturned for each claims administrator above. The numbers paint a very clear picture of who plays fair and who doesn’t care.
In the meantime, keep submitting your bills for Second Review – we’ve got our sights set on $20 million.
To learn more about how daisyBill can supercharge your work comp second reviews, schedule a live demo with one of our billing experts.
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.