Claims Administrator Days to Payment Q1 – Q3
So you’ve filled out all the required fields in daisyBill and clicked ‘submit’ on your bill. End of story? Not a chance.
For us, that’s just the beginning.
From the moment you click ‘submit,’ our software works overtime to collect payment amounts, payer activity, submission types, code counts, denial reasons, and more.
The result? A really, really big spreadsheet. And in that spreadsheet? Some truly spectacular Claims Administrator days-to-payment data.
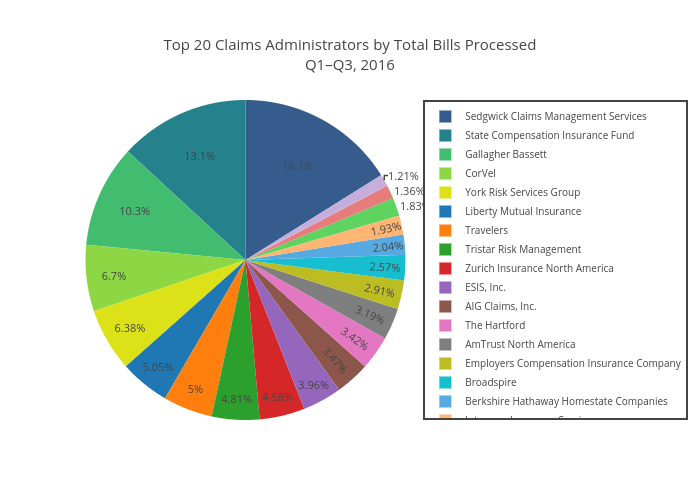
Over the first three quarters of 2016, daisyBill processed more than 640,000 bills. We isolated the top 20 claims administrators by volume, then went to town with the graph-maker.
Unsurprisingly, big names dominate this list. Sedgwick Claims Management Services, State Compensation Insurance Fund, and Gallagher Bassett topped the list, accounting for nearly 40% of all bills within the top twenty.
Pie Chart:
Volume is great, but what about speed? Remember, Labor Code 4603.4 requires that “Payment for medical treatment provided or prescribed by the treating physician… shall be made with an explanation of review by the employer within 15 working days after electronic receipt” of an electronic bill.[1]
Keeping that in mind, we isolated original bill submissions for medical treatment handled by our top twenty claims administrators and compared average business days to payment.
Last time we checked, Liberty Mutual led the way, with an average payment time of six days. Two additional quarters of data cement their position at the top of the pack.
Bar Graph:
In total, seven of the top twenty claims administrators delivered payment on original submissions of medical treatment bills in ten business days or fewer: Liberty Mutual, State Compensation Insurance Fund, Gallagher Bassett, Berkshire Hathaway Homestate Companies, Broadspire, Travelers, and The Hartford.
On the opposite end of the spectrum, AIG Claims, Inc., Athens Administrators, Tristar Risk Management, and AmTrust North America all ran afoul of the 15-day mandate in Labor Code 4603.4. Meanwhile, Intercare Insurance Services barely squeaks in with an average of 15 business days. The good news? Those five claims administrators combined for less than 15% of bill submissions within the top twenty.
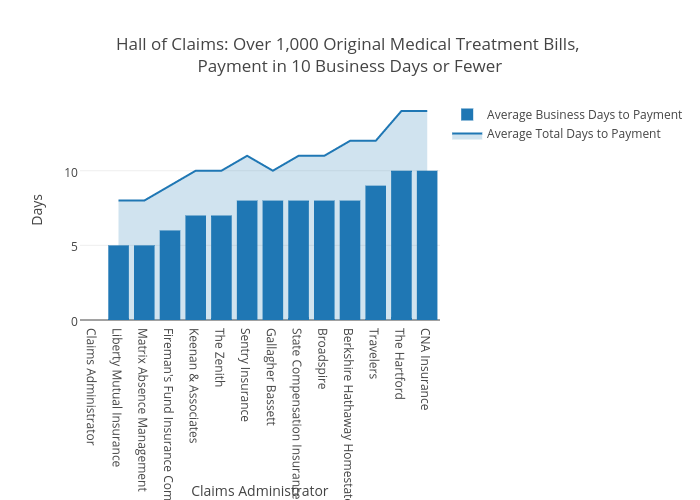
One last thing before we go – we’d like to shout out an elite group of thirteen claims administrators who processed over 1,000 original medical treatment bills while delivering payment in ten business days or fewer. They may not all have cracked the top twenty by volume, but the display of power and speed is impressive nonetheless.
Bar graph:
Now that’s what we call a claim to fame.
Tired of submitting your work comp via mail and waiting weeks – if not months – for payment to come through? We can show you a better way. Click below to schedule a demo and experience the power of electronic billing.
REQUEST DEMO
[1] Full text of Labor Code 4603.4 here.
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.png)
.gif)