UR & RFA: Still Important for Work Comp
I read about a recent Workers’ Compensation Appeals Board ruling about utilization review (UR) with a lot of interest. I won’t get into technical and legislative details about the case (David DePaolo does an excellent job of it) but the takeaway is this:
A disputed UR will always go to independent medical review (IMR) unless the UR was untimely. An untimely UR is the ONLY circumstances under which a UR dispute leaves the IMR process and enters the WCAB system.
Injured workers, medical providers, and applicant attorneys don’t like this decision because IMR upholds the overwhelming majority of UR decisions (and, of course, the UR is in dispute in the first place because treatment was not approved). The WCAB’s decisions on medical necessity tended to be more favorable to providers than the IMR decisions.
Now that timeliness is the only issue outside the realm of the IMR process, both providers and claims administrators need to prepare for or defend against, as the case may be, timeliness assertions.
To break it down:
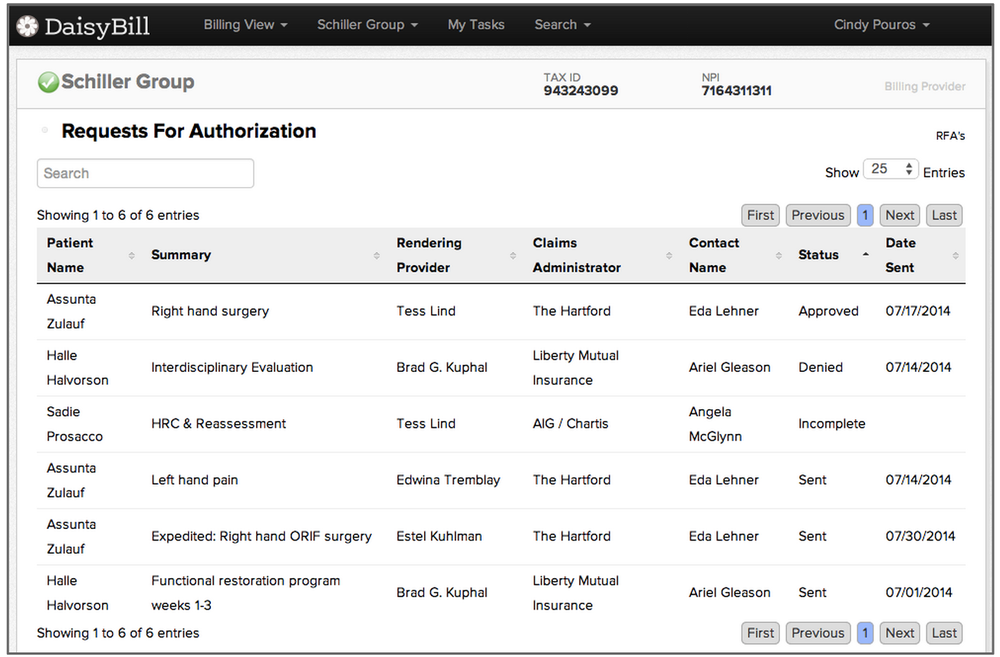
- Claims administrators must respond within the mandated timelines for RFA and UR.
- Both providers and claims administrators must keep meticulous and verifiable records of Request for Authorization (RFA) submissions and RFA responses.
I recommend that you do as we do at DaisyBill. We keep copies of all RFAs and RFA decisions, along with their transmittal date and records of receipt.
Also, if you miss our RFA webinar later today, we’ll be posting some of the slides later on our Webinar Library.
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.