“Automatic” Authorization, but Denied Bill? How to Appeal the Denial
The new “automatic” authorization process for workers’ comp is in effect, as of January 1. We’ve discussed this new system extensively on our blog and in our recent webinar, covering everything from eligibility to timeliness to new utilization review requirements. But what happens if the employer or insurer’s claims administrator denies payment for automatically authorized services rendered? Does the usual second review appeal process apply?
In short, authorized is authorized, automatically or otherwise — but in this case, there is a twist.
As we’ve said before, second review appeals are the provider’s burden. When the claims administrator incorrectly denies payment, it’s on the provider to demand redress and provide relevant documentation. Providers must make their case, or the default outcome is a loss of revenue.
Automatic authorization adds a new dimension to the second review process. That’s because the claims administrator essentially has no ability to deny the recommended treatment. On top of that, billing timelines are very different — as are the rules regarding timely bill submission and the penalties for untimeliness.
Billing Rules Under Automatic Authorization
When a service is automatically authorized, there is no utilization review (UR). The treatment (as long as it meets the 6 DWC-required conditions) is authorized without input from the claims administrator. And while the revised Labor Code § 4610 requires the provider to submit a retrospective RFA within 5 days, the claims administrator cannot modify or deny the recommended treatment.
Significantly, 4610 also requires the provider to submit the original bill for services rendered much sooner than usual. For services authorized in the standard way, the deadline to submit the original bill is 12 months. But for automatically authorized services, providers must submit the original bill within 30 days of service for non-emergency treatment, and within 180 days for emergency treatment.
Here’s the twist.
When a provider untimely submits a bill for non-automatically authorized services, the claims administrator is under no obligation to pay. After 12 months, the provider is simply out of luck. But for automatically authorized services, the new § 4610 makes no provision for non-payment of untimely submitted bills.
That’s right: as it stands, the claims administrator must pay for automatically authorized services, even when the bill is late.
Consequences for Non-compliance
Automatic authorization creates unique wrinkles in the billing and appeals process. Not only is the claims administrator powerless to deny authorization for automatically authorized services, even provider untimeliness cannot remove the obligation to reimburse. The rules are different, but so are the consequences.
The employer or insurer can enact some penalties if a provider abuses automatic authorization. While UR for automatically authorized services is not required, the employer can conduct retrospective UR to determine if the provider acted within the bounds of the Medical Treatment Utilization Schedule (MTUS).
The employer still cannot deny or modify the requested treatment, nor can they rescind authorization, even the automatic sort. But if the employer can demonstrate a pattern of treatment not in accordance with the MTUS, they can remove the provider’s permission to provide automatically authorized treatments. They can also remove the provider from the MPN or HRO in question.
None of which releases the claims administrator from their legal obligation to pay for authorized services rendered.
Of course, we always recommend full compliance on both sides of the workers’ comp billing and payment equation. Providers should, if only to reduce friction, adhere to § 4610’s 30 and 180 day billing deadlines for non-emergency and emergency treatment, respectively. That said, failure to do so is not grounds for denial of payment.
Second Review Procedure
While the requirements (and consequences for non-compliance) regarding authorization and billing are different under the “automatic” system, the rules for second review are not. When the claims administrator returns an incorrect denial, the provider must still adhere to the usual second review rules:
- Timeliness: Submit Second Review appeal within 90 calendar days from receipt of the Explanation of Review (EOR).
- Format: Use either a modified original bill or DWC Form SBR-1. (We strongly recommend using the DWC Form SBR-1 ).
- Delivery: Use the same delivery method (i.e., paper or electronic) as the original bill.
- Reason: Articulate the rationale for disputing the incorrect payment.
- Documentation: Provide all relevant supporting documentation.
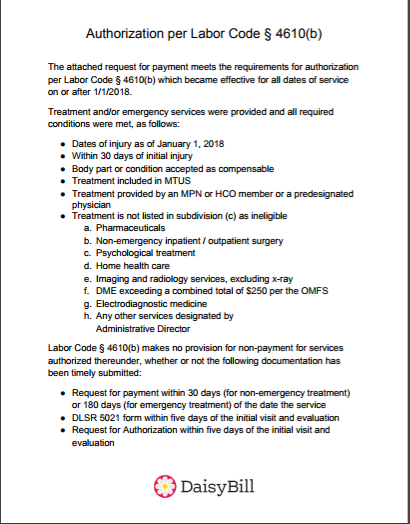
For automatically authorized services, we strongly recommend attaching supporting documentation that substantiates the treatment’s eligibility for automatic authorization. Below is a sample letter to the claims administrator with sufficient language:
To download this sample letter as a printable pdf, just click here. Use this letter whenever a claims administrator incorrectly denies a bill for compliantly, automatically authorized services rendered. As always, we’ve got your back!
daisyBill makes compliant authorization, billing, and appeals easier than ever. Schedule a free demonstration of our Billing Software for your office, and see just how easy workers’ comp can be.
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.