96136 / 96137 - Sedgwick Claims Management Services: Grade F
%20rounded.png)
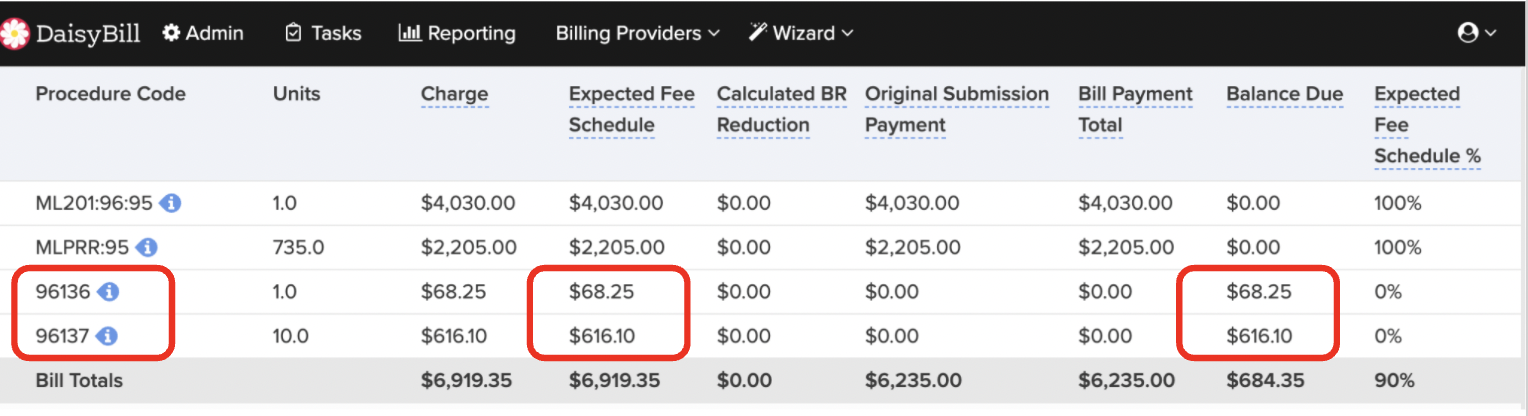
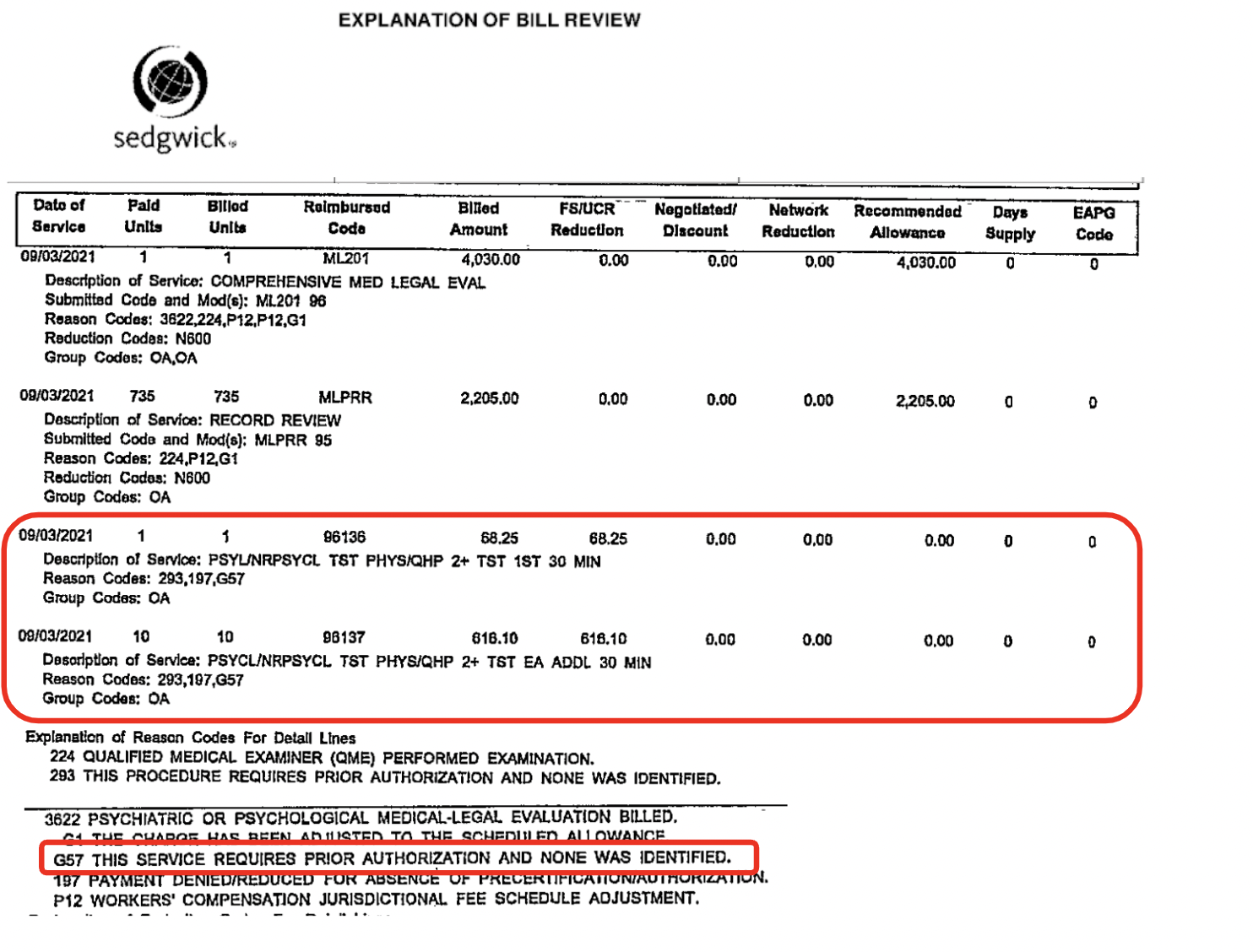
Claims administrator failed to properly reimburse 96136 and 96137 as part of a Medical-Legal evaluation. Sedgwick incorrectly denied reimbursement citing prior authorization required.
Date of Service: 09/03/2021
MLFS Code(s) |
ML201 - Comprehensive Medical-Legal Evaluation MLPRR - Record Review |
MLFS Modifier(s) |
96 - Evaluation performed by a Psychiatrist or Psychologist 95 - Evaluation performed by a panel selected Qualified Medical Evaluator |
Diagnostic Code(s) |
96136 - Psychological or neuropsychological test administration and scoring by physician - first 30 minutes 96137 - Psychological or neuropsychological test administration and scoring by physician - each additional 30 minutes |
MLFS Grade |
F |
Claims Administrator |
Sedgwick Claims Management Services |
Bill Review Vendor |
Sedgwick CMS National Bill Review |
Employer |
Transdev |
|
EOR Adjustment Reason |
G57 - This service requires prior authorization and none was identified. |
Second Review Reason to dispute incorrect reimbursement |
Claims administrator incorrectly denied reimbursement. For the medical-legal evaluation, adequate diagnostic tests were not included in the medical information (i.e. current and relevant test results) sent by the parties. To complete the medical-legal evaluation, the evaluator performed diagnostic tests. Per the DWC reimbursement is due for said testing: “A claims administrator must pay for a diagnostic test ordered by an AME or QME as long as the subjective complaints and physical findings that warrant the necessity for the test are included in the medical/legal evaluation report.” 96136 payment due: $68.25. 96137 payment due: S616.10. In addition to payment, penalties and interest are now due. An IBR will be filed upon failure to properly reimburse the diagnostic codes. |
View All MLFS Report Cards
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.