Introducing: CA Med-Legal Fee Schedule Report Cards

At DaisyBill, we strive to help providers and their staff navigate the complexities of workers’ comp billing and payment, to ensure proper reimbursement. To that end, we’re debuting our California Medical-Legal Fee Schedule (MLFS) Claims Administrator “Report Cards.”
Since California’s new MLFS took effect on April 1, 2021, some claims administrators have proven better than others at properly reimbursing new billing codes and modifiers. With our Report Cards, providers can see which claims administrators get Medical-Legal payment right, which get it wrong, and how to appeal incorrect payments.
As our library of Report Cards grows, providers will be able to see exactly how charges for each new Medical-Legal billing code should be reimbursed — and which common mistakes various claims administrators make consistently. Providers, use the Report Cards as a go-to resource to make sure your bills for Medical-Legal services are paid correctly.
A Go-To Med-Legal Resource for Providers
Each time a claims administrator returns an Explanation of Review (EOR) to a DaisyBill provider, we generate a Report Card on the claims administrator’s adjudication of the bill. As displayed below, each Report Card specifies:
- The Medical-Legal billing code
- The claims administrator
- The claims administrator’s bill review
- The employer
- Our MLFS “grade” for the claims administrator
- The amount due to the physician per the MLFS
- The amount paid to the physician by the claims administrator
- The EOR
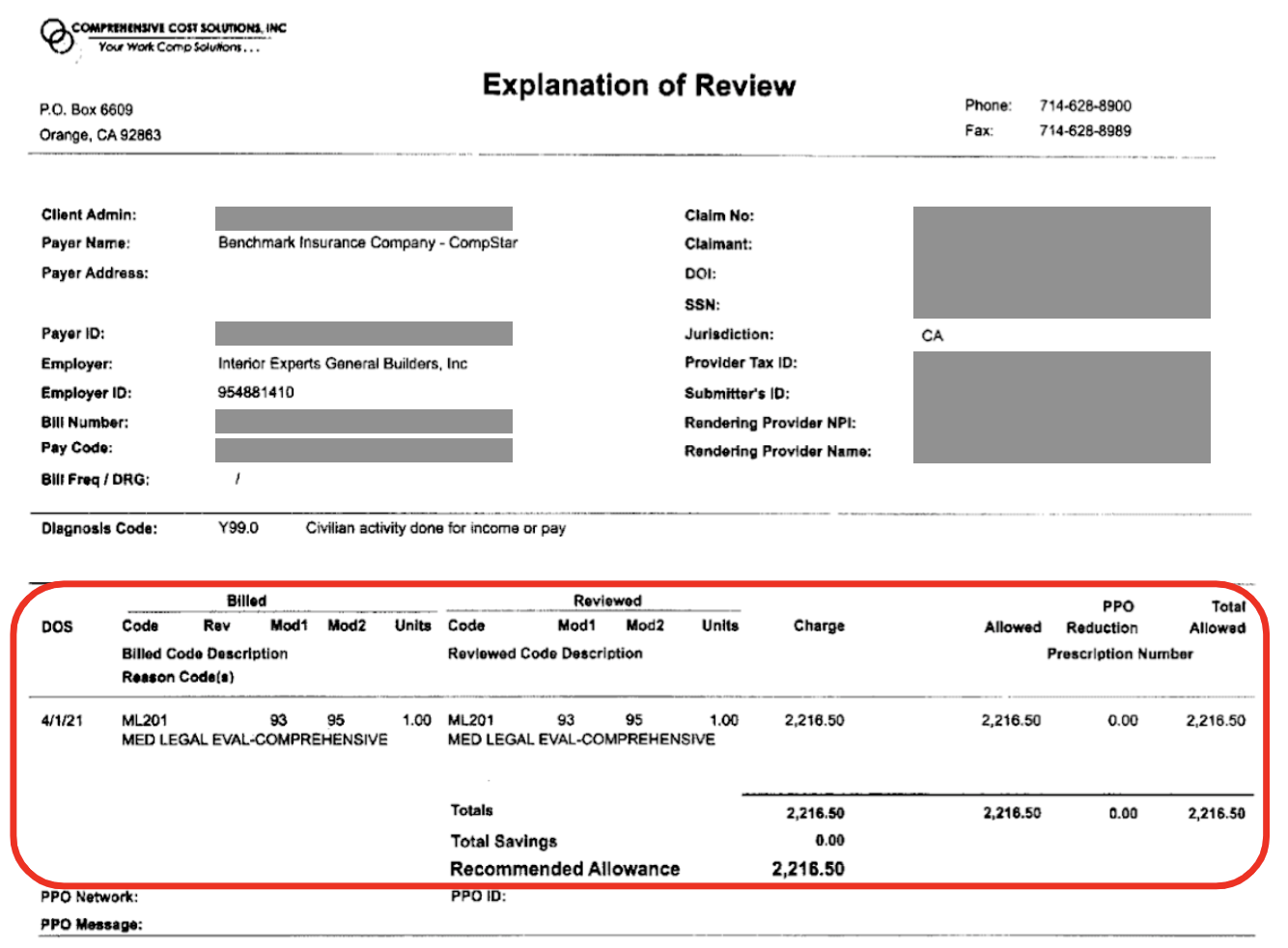
An “A” grade reflects a perfect adjudication with completely accurate payment. For example, this bang-up job from Benchmark:
Benchmark Insurance Company - MLFS Grade: A.
This claims administrator properly processed a California medical-legal bill submitted for ML201.
Procedure Code |
ML201 - Comprehensive Medical-Legal Evaluation |
Claims Administrator |
Benchmark Insurance Company |
Bill Review Vendor |
Comprehensive Cost Solutions, Inc |
Employer |
Interior Experts General Builders, Inc |
MLFS Grade |
A |
Amount Due |
$2,216.50 |
Amount Paid |
$2,216.50 |
In cases where the claims administrator failed to properly reimburse for a Medical-Legal service, our Report Card will also include:
- The Claims Adjustment Reason Code
- Second Review appeal language, with which providers can dispute similar incorrect adjustments
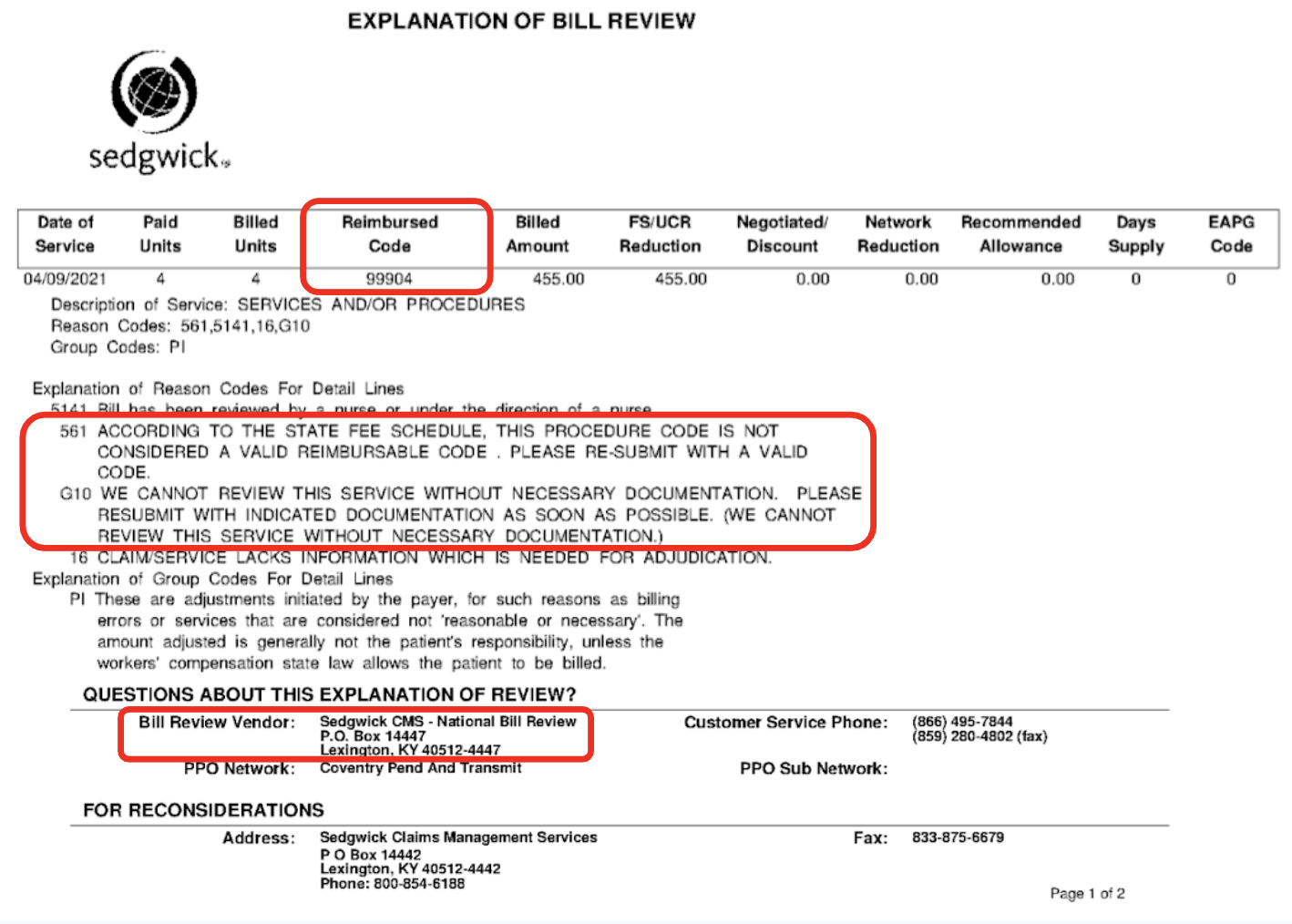
For example, see the below “F” grade from Sedgwick:
Sedgwick Claims Management Services - MLFS Grade: F.
This claims administrator failed to properly process a California medical-legal bill submitted for ML204. To receive correct payment, the provider must submit a timely and compliant Second Bill Review to dispute the incorrect reimbursement for the services.
Procedure Code |
ML204 - Fees for Medical-Legal Testimony |
Claims Administrator |
Sedgwick Claims Management Services |
Bill Review Vendor |
Sedgwick CMS National Bill Review |
Employer |
Orange County Zone |
MLFS Grade |
F |
Amount Due |
$455.00 |
Amount Paid |
$0.00 |
Adjustment Reason Code |
561 - According to the state fee schedule, this procedure code is not considered a valid reimbursable code. Please re-submit with a valid code. |
Second Review Reason to dispute incorrect reimbursement |
Claims administrator incorrectly denied reimbursement. Per CCR §9795, if a deposition is cancelled fewer than 8 calendar days before the scheduled deposition date, the physician shall be paid a minimum of one hour for the scheduled deposition. ML204 payment due: $455.00. In addition to payment, penalties and interest are now due. |
Make RFAs, billing, and appeals easier than ever — and get paid faster. DaisyBill empowers providers to collect what’s owed in record time. Contact us to learn how we can help your practice.
LET’S CHAT!
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.