For CA Interpreters, Appeals Pay More Than Bills
California interpreters, pay close attention!
A new interpreter service began using daisyBill in February. Since then, the service has collected more revenue from Second Review appeals than from the original bills initially submitted.
Providers, including interpreters, must submit Second Review appeals to dispute incorrect denials or adjustments in payment. For this interpreter service, collections from Second Review appeals increased revenue by 149% in just four months.
These dramatic numbers demonstrate California’s de facto incentivization for claims administrators to underpay providers (of both health care and health care-related services like language interpreting). For any improperly denied or reduced payment, if a provider fails to timely appeal, the claims administrator keeps the balance owed.
In this case, the interpreter service was so consistently, dramatically underpaid that revenue more than doubled from the simple act of clicking ‘Second Review’ in the daisyBill application.
The sad fact is that claims administrators consistently underpay providers throughout California. If you have any doubts that consistent Second Review appeals are a necessity, these numbers are proof.
Second Review Appeals Are Not Optional
daisyBill provides each client with eleven Payment Analytics reports featuring detailed collection analyses, updated daily. Given the importance of submitting Second Review appeals, multiple reports include Second Review appeal data.
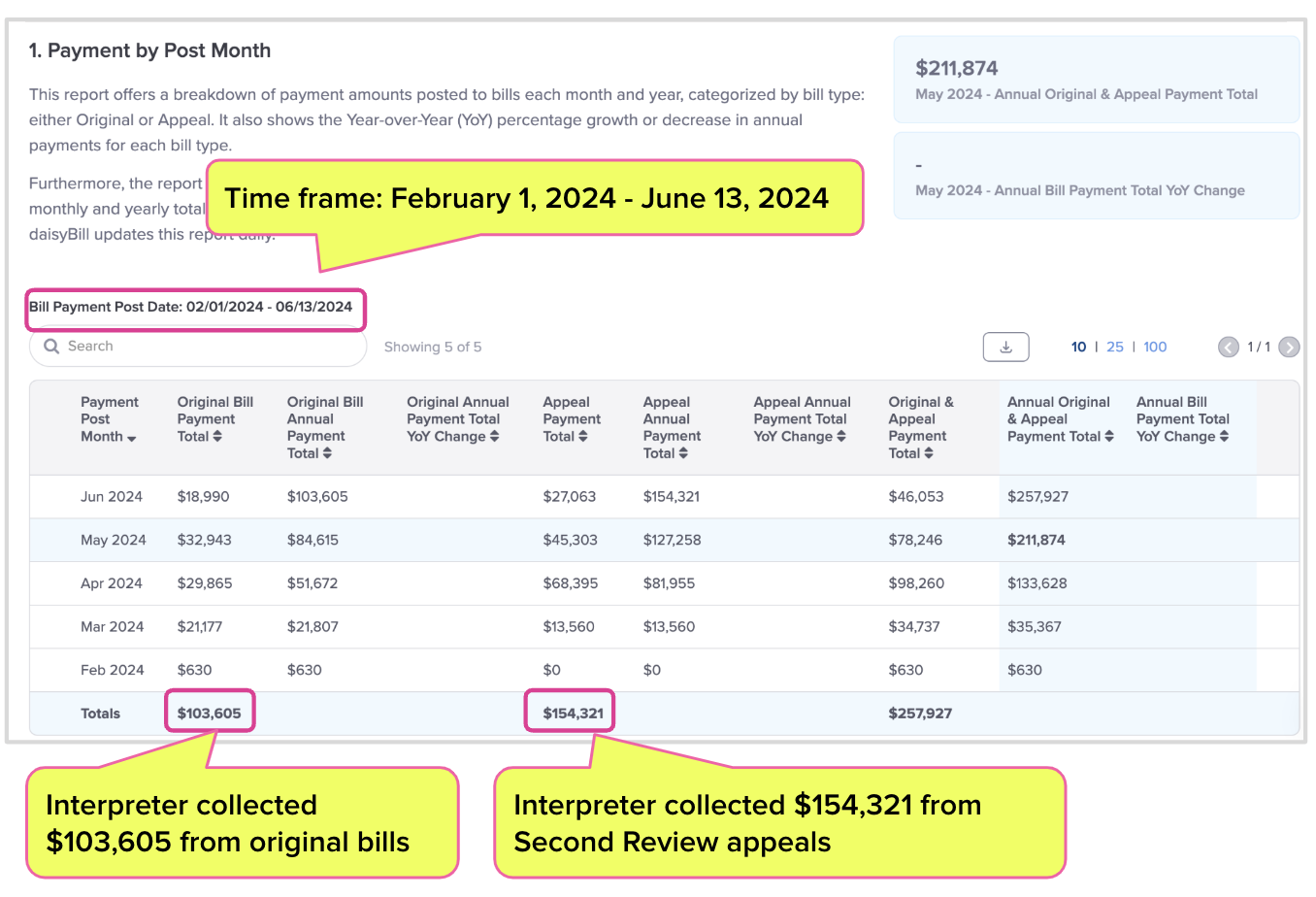
The screenshot from the interpreter’s Payment by Post Month report (below) shows that for payments posted since February 1:
- Claims administrators collectively paid the interpreter $103,605 for all original bills.
- The same claims administrators subsequently paid the interpreter an additional $154,321 in response to Second Review appeals the interpreter sent to dispute incorrect payments.
These data demonstrate how claims administrators routinely fail to correctly reimburse interpreters for service rendered to injured workers. But without this report, the interpreter may not realize just how essential Second Review appeals really are.
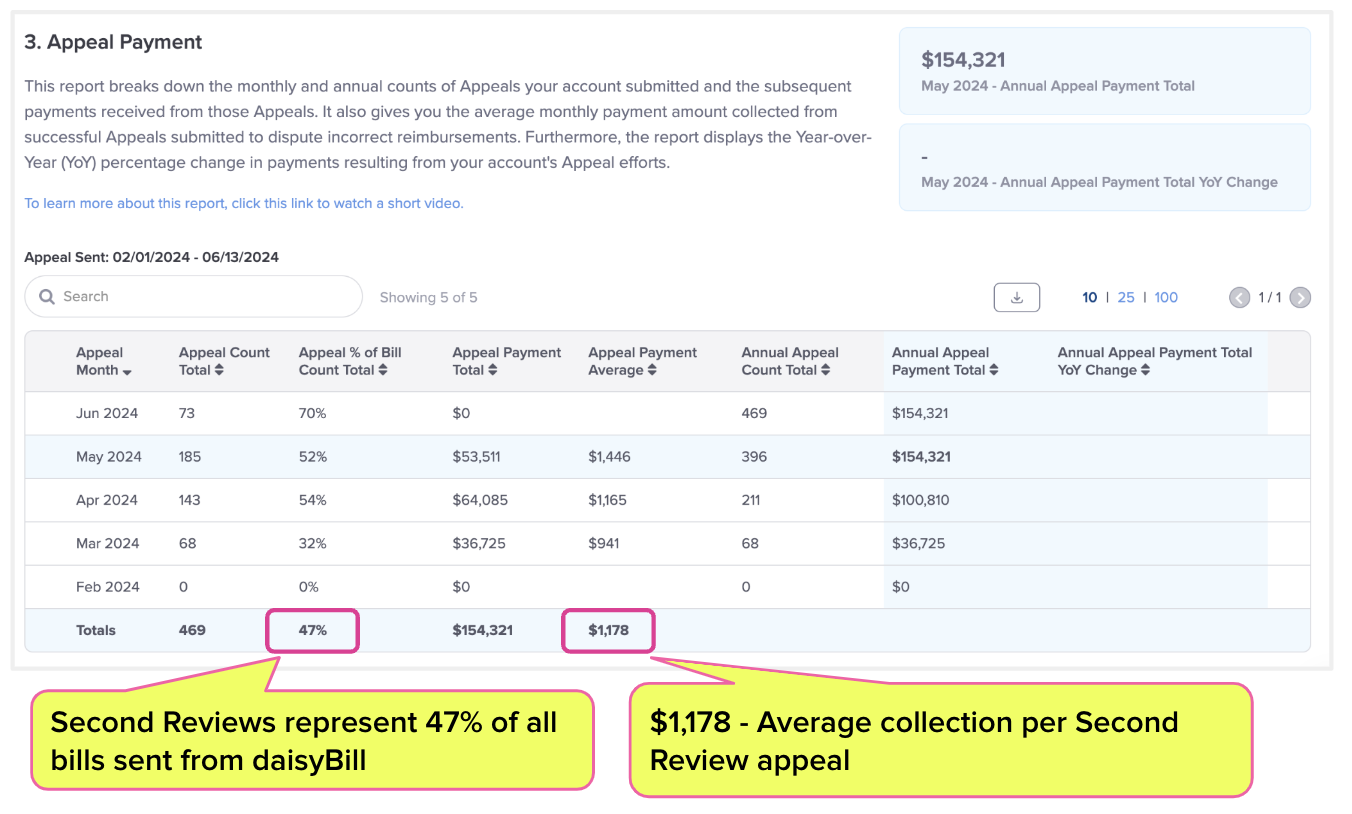
The screenshot below from the interpreter service’s Appeal Payment report provides even more detailed insight into payments received for appeals. Since starting with daisyBill:
- The interpreter service submitted 469 Second Review appeals in total.
- 47% of the service’s bill submissions have been Second Review appeals to dispute incorrect reimbursements.
- On average, each appeal paid the interpreter $1,178.
Claims administrators consistently shorted this interpreter, an unfortunate but common practice. Our recent article on bill denial data revealed that depending on the claims administrator, anywhere from 1% to 42% of all bills are denied in their entirety—and that’s without factoring in improper reductions in reimbursement amounts or individual line item denials.
To top it all off, denial rates are only getting worse. Providers—including interpreters—have no choice but to establish procedures for consistently appealing denials and underpayments.
Second Review Applies to Interpreter Services
Thanks to misinformation, too many interpreters mistakenly believe that Second Review appeals are not an option for them.
California Code of Regulations (CCR) Section 9792.5.4 states that workers’ comp bills are subject to Second Review only when there is a state fee schedule for the services. Since California’s Official Medical Fee Schedule (OMFS) does not contain an interpreter fee schedule per se, many interpreters believe Second Review is off the table.
However, a 2019 court case, Meadowbrook Ins. v WCAB, established that CCR Section 9795.3 (which establishes “reasonable” fees for interpreter services) legally serves as the interpreter's “fee schedule” for billing and appeal purposes.
Bottom line, interpreters: you can submit Second Review appeals—and you should. If you don’t, you’re leaving potentially large amounts of money on the table, which claims administrators and their private equity owners are only too happy to grab. Don’t allow claims administrator “errors,” effectively encouraged by California’s payer-friendly system, to drain your bank account.
The video below shows that the right technology makes it easy to submit timely, compliant Second Review appeals and get the reimbursements you’re owed.
With tools for quicker, easier appeals, daisyBill gets you full reimbursement with just a few clicks. Learn more below:
LEARN MORE
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.

.gif)
.png)
