Sedgwick Denies/Ignores Hundreds of Appeals
Sedgwick's persistent failure to pay providers in accordance with state workers' comp fee schedules and its refusal to respond compliantly to providers’ appeals are glaring violations of California’s laws.
Worse, the Division of Workers’ Compensation (DWC) seems entirely disinclined to do anything about it despite tens of thousands of formal Audit Complaints documenting and reporting Sedgwick’s violations.
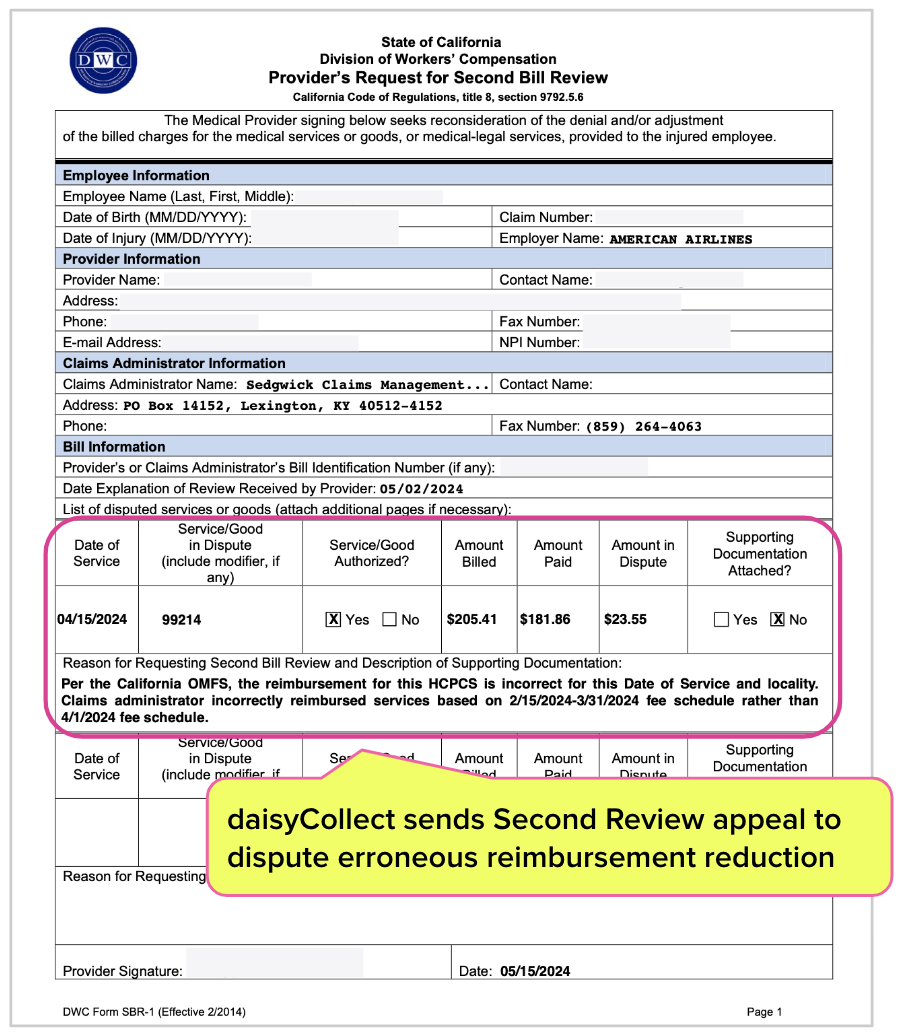
For just two practices, daisyCollect submitted 239 Second Review appeals to dispute Sedgwick’s failure to reimburse at the rates established by a Physician Fee Schedule update effective April 1, 2024. Each appeal was identical in that it indicated that Sedgwick did not reimburse the provider the correct rate due for the date of service based on the update.
Sedgwick paid just 43% of the appeals and either improperly denied or blatantly ignored 136 of the appeals.
For the denied appeals, the only recourse is to pay $180 to request Independent Bill Review (IBR). For the appeals Sedgwick ignored, daisyCollect agents must relentlessly pursue Sedgwick through phone calls, chats, and emails until the appeal is addressed (providers may not request IBR until after the claims administrator conducts Second Review).
daisyCollect clients have the advantage of outsourcing these endless battles to our agents. But how many providers are losing revenue because they lack the time, resources, or technology to fight Sedgwick's de facto pilfering?
Sedgwick Payment Torture: By the Numbers
To obtain correct payment, daisyCollect sent Sedgwick 239 Second Review appeals asserting (accurately) that the Third-Party Administrator (TPA) applied the wrong reimbursement rates for the date of service.
California law, as found in Labor Code Section 4603.2(e)(3), mandates that claims administrators respond to Second Review appeals within 14 calendar days with additional payment and a final Explanation of Review (EOR).
For 57% of the appeals, Sedgwick ignored the law as follows:
- Denied 35% of the appeals incorrectly as “duplicate” bills
- Denied 13% of the appeals citing another verifiably untrue reason
- Ignored 9% of the appeals, offering no response by the deadline
Sedgwick Second Review Appeal Responses |
Appeal Response Count |
Response % |
Appeal Paid |
103 |
43% |
Appeal Denied as “Duplicate” Bill |
83 |
35% |
Appeal Denied for Other Invalid Reason |
32 |
13% |
No Response to Appeal |
21 |
9% |
Total Second Review Appeals Sent |
239 |
100% |
DWC Enables Sedgwick Defiance
Navigating Sedgwick’s behavior is a burden placed on providers not only by Sedgwick, but also by state authorities that have shown no apparent interest in enforcing the laws that protect providers.
The DWC is fully informed of Sedgwick’s well-established practice of improperly denying Second Review appeals as “duplicate” bills; in April 2022, daisyBill sent the DWC over 4,000 Audit Complaints detailing these violations.
Fast-forward two years, and the DWC has failed to impose any consequences to deter Segwick’s impermissible business practices. Meanwhile, the DWC remains complacent, effectively enabling Sedgwick's exploitation of providers.
Remember, the table above represents only two practices. Extrapolating this payment abuse data to the entire state reveals that no provider can protect themselves from Sedgwick’s blatant disregard for fee schedules and the mandated appeals process.
All of this happens in the absence of regulatory consequences. Such permissiveness can only encourage behavior like Sedgwick’s, discourage providers, and further the erosion of the workers’ comp system.
We deal with Sedgwick so you don’t have to. daisyCollect professionals use advanced software (and years of experience) to protect your practice. Learn more below:
LEARN MORE
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.gif)
