Coding Clinic: How to Bill for Evaluation & Management Services

As the Centers for Medicare and Medicaid Services (CMS) like to say, “If it is not documented, it has not been done.” Of course, documenting can be just as painstaking as the doing, especially in workers’ comp. Sometimes — as in the case of Evaluation and Management (E/M) services — the documentation is frightfully complicated, making billing even more of a hassle than usual.
E/M services billing requires providers to select the correct billing codes for the level of services rendered. Determining which level can be tricky. Fortunately, there’s a guide for that.
To determine which level of E/M services the provider rendered (and thereby determine the appropriate coding), providers must refer to the CMS’ Documentation Guidelines for Evaluation and Management Services. There are two relevant editions of this guide, from 1995 and 1997. Providers may use either, but not a combination of the two.
Each level of E/M service is defined by its descriptors. The descriptors are comprised of seven E/M components:
- History
- Examination
- Medical Decision Making
- Counseling
- Coordination of Care
- Nature of Presenting Problem
- Time
Of those seven, the first 3 are the “key” components that primarily determine the appropriate level of E&M service, and therefore the appropriate coding (with one exception, described below). Once the provider determines the correct types of these 3 components, they can pinpoint the overall level of E/M service rendered.
Understand that the rules determine the E/M service level based on 2 of the 3 key components. This means that providers cannot necessarily bill based on the highest level reached by any one component, but rather on the conjunction of two. The CMS offers guidelines for determining which type of History, Examination, and Medical Decision Making the provider rendered:
Key Component #1: History
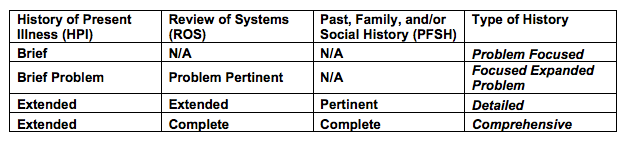
The types of history-establishing services include Problem Focused, Focused Expanded Problem, Detailed, and Comprehensive. To qualify as any one of these 4 types, the service must meet all 3 of the respective criteria for each type as listed in the table below, from the CMS
Key Component #2: Examination
Like History, the four types of examination include Problem Focused, Focused Expanded Problem, Detailed, and Comprehensive. To determine which type of examination occurred, refer to the following CMS definitions:
- Problem Focused - a limited examination of the affected body area or organ system.
- Expanded Problem Focused - a limited examination of the affected body part or organ system and any other symptomatic or related body area(s) or organ system(s).
- Detailed - an extended examination of the affected body area(s) or organ system(s) and any other symptomatic or related body area(s) or organ system(s).
- Comprehensive - a general multi-system examination or complete examination or a single organ system and other symptomatic or related body area(s) or organ system(s).
Key Component #3: Medical Decision Making
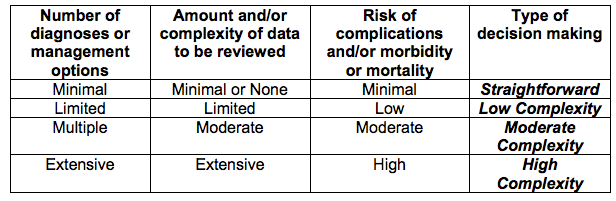
Determining the type of Medical Decision Making essentially comes down to the decision’s complexity. The types include Straightforward, Low Complexity, Moderate Complexity, and High Complexity. To qualify as any given type, the decision must meet 2 of the 3 respective criteria listed in the table below:
Time-Based E&M
As mentioned above, there is an exception to the usual 3 “key” components being the primary determining factors in which level of E/M to code for. For E/M services that consist primarily of components 4 (Counseling) and 5 (Coordination of Care), component 7 (Time) is the “key” factor in determining the level of E&M service rendered. |
For visits in which counseling or coordination of care comprise 50% or more of the total encounter, time is the key controlling factor to qualify for a given level of E/M service. Providers must document the total face-to-face time spent, and keep records that describe the counseling or coordination activities.
For more detailed explanations of the criteria for each component, see the CMS Guide. For further resources, including relevant Independent Bill Review (IBR) decisions regarding E/M billing, see our FAQ.
daisyBill’s Billing Software includes everything providers need to bill correctly, compliantly, and effectively. To see how much easier workers’ compensation billing can be, schedule a free demonstration for your office!
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.