CA Alert: ESIS e-Bill Rejections (and What to Do)
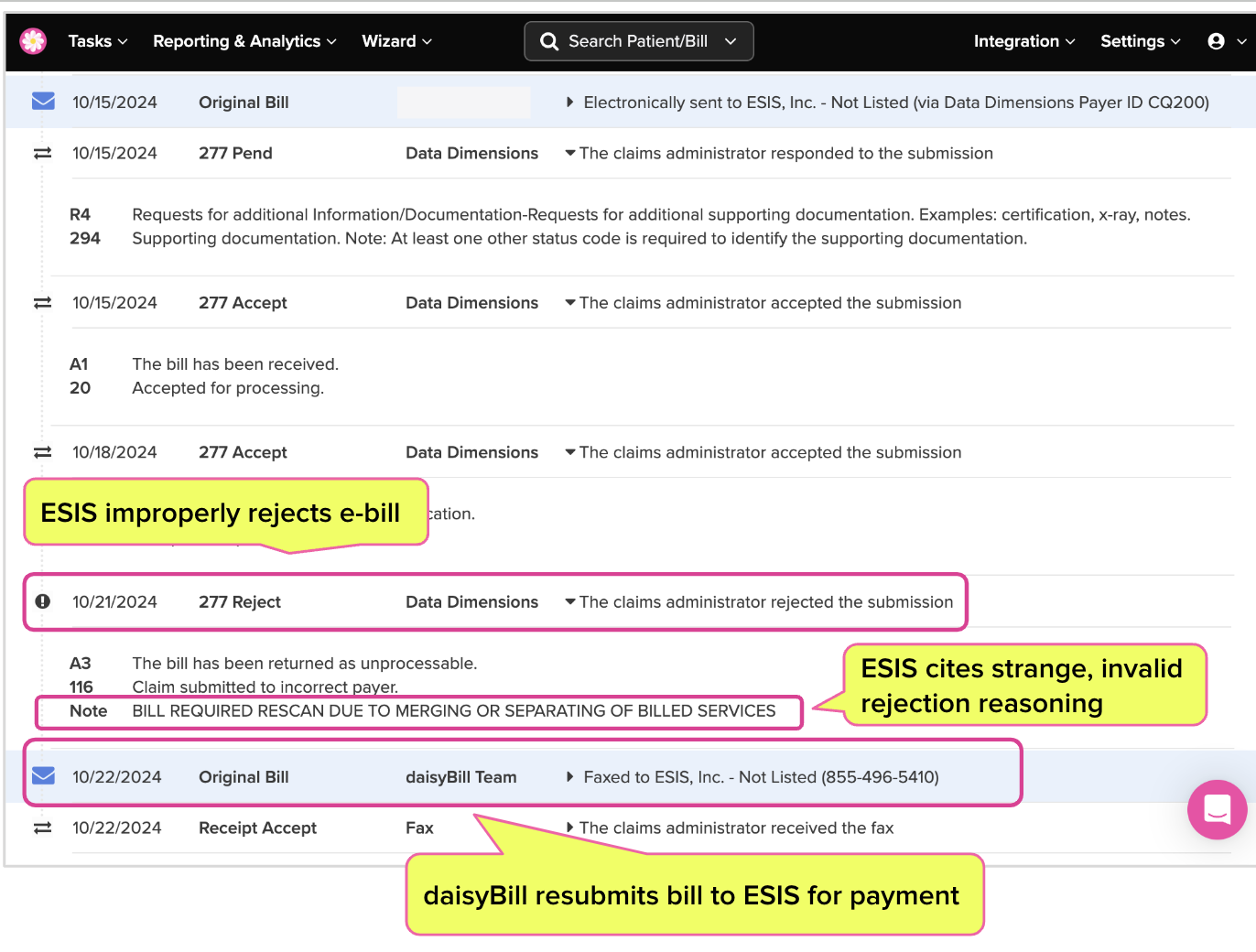
Third-party administrator (TPA) ESIS is improperly rejecting valid e-bills from California providers, citing an inexplicable, seemingly random (and definitely non-compliant) reason.
So far, ESIS has rejected 171 daisyBill clients’ e-bills, offering only the nonsensical “explanation” that the e-bills “REQUIRED RESCAN DUE TO MERGING OR SEPARATING OF BILLED SERVICES.”
If that sounds like meaningless technobabble, that’s because it is. Representatives of ESIS’s clearinghouse vendor Data Dimensions, which accepts and responds to provider’s e-bills on the TPA’s behalf, confirmed that ESIS’s rejection reason is invalid and “odd.”
The bad news is that despite repeated attempts by Data Dimensions to work with ESIS to resolve the issue (kudos to DD, by the way), the TPA has apparently remained uncooperative. Multiple communications, follow-ups, and escalation attempts by Data Dimensions have proved unfruitful.
The good news is that this strange glitch has a relatively easy fix. According to Data Dimensions, providers must simply resubmit affected bills, and ESIS will process them properly.
The really bad news is that California workers’ comp’s consequence-free environment for non-compliant claims administrators gives ESIS little incentive to uphold its obligations to providers who treat injured workers.
ESIS Rejects e-Bills for Random “Reason”
ESIS began rejecting compliant e-bills in late July, using the wholly inapplicable (and frankly bizarre) rejection “reason” noted above.
When a provider sends an electronic bill (aka an e-bill) to a claims administrator, the claims administrator’s clearinghouse vendor must initially respond with a ‘277’ electronic receipt indicating whether the e-bill was accepted or rejected for processing.
Occasionally, a clearinghouse rejects an e-bill due to technical errors or missing information. But in this case, Data Dimensions accepted the affected e-bills and forwarded them to ESIS—but ESIS rejected and refused to process the e-bills, citing:
“BILL REQUIRED RESCAN DUE TO MERGING OR SEPARATING OF BILLED SERVICES.”
Between July 29, 2024 and October 24, 2024, ESIS rejected 171 e-bills in this manner.
daisyBill’s Compliance Team reviews our clients’ e-bill rejections and contacts the claims administrator’s designated clearinghouse when an e-bill is rejected improperly. In this case, with ESIS refusing to cooperate with efforts to resolve its apparent e-billing glitch (details below), daisyBill resubmitted the affected bills via fax.
ESIS Gives Data Dimensions the Runaround
In July 2024, daisyBill contacted ESIS’ designated clearinghouse, Data Dimensions, to report the improper e-bill rejections. Over several months, Data Dimensions shared its continuous attempts to resolve the problem, but it apparently received no clear feedback or substantive action from ESIS.
We thank and applaud Data Dimensions for its exceptional responsiveness and proactivity in addressing the problem. ESIS, however, proved to be a stone wall.
Despite Data Dimensions' efforts to bring ESIS into compliance, to our knowledge the TPA has yet to explain or address the nonsensical denial reasoning. As a result, the core issue remains unresolved. However, as of October 2024, Data Dimensions advises that providers can simply resubmit affected bills for processing.
Not for the first time, ESIS is wasting providers’ time and resources, this time by forcing practices to submit the same bill twice to receive payment. While glitches and errors are inevitable, ESIS’s apparent refusal to sufficiently communicate even with its own clearinghouse is a significant, if passive, insult to providers who expect their bills to be processed and paid in a timely manner.
Once again, we appreciate Data Dimensions’ efforts. As a clearinghouse, Data Dimensions has only so much power to prod its clients toward compliance, but it clearly went above and beyond in its attempts to untangle this problem.
Once again, in the absence of willing or effective regulators, California providers must depend on vendors like daisyBill and Data Dimensions to help enforce the billing laws and regulations designed to protect providers from abuse.
daisyBill makes treating injured workers easier, faster, and less costly. Request a free demonstration below.
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.