Helmsman's Ridiculous Refund Request (Part 1)
Why do so many doctors avoid treating injured workers? We have a perfect illustration from Helmsman Management Services LLC. This Third-Party Administrator (TPA) recently:
- Underpaid a doctor for treating an NBC Universal injured employee
- Subsequently, incorrectly determined that the doctor's bill was “not related” to any claim Helmsman manages
- Demanded a full refund from the doctor
To be clear, there’s no question whether the doctor’s bill was legitimate. Helmsman paid the doctor multiple times for treatment on this exact injury claim—both before and after the bill date of service that Helmsman questions.
Daily, doctors fight battle after (uphill) battle simply to receive reimbursement for treating injured workers. Even after the check has cleared, Helmsman proves there’s no guarantee a doctor’s payment torture is over.
This example of Helman’s run-a-muck payment abuse is yet another reason that doctors refuse to treat California’s injured workers.
(Tip to NBC: Helmsman’s inability to keep track of injury payment details should hardly be comforting.)
Helmsman Demands a Refund
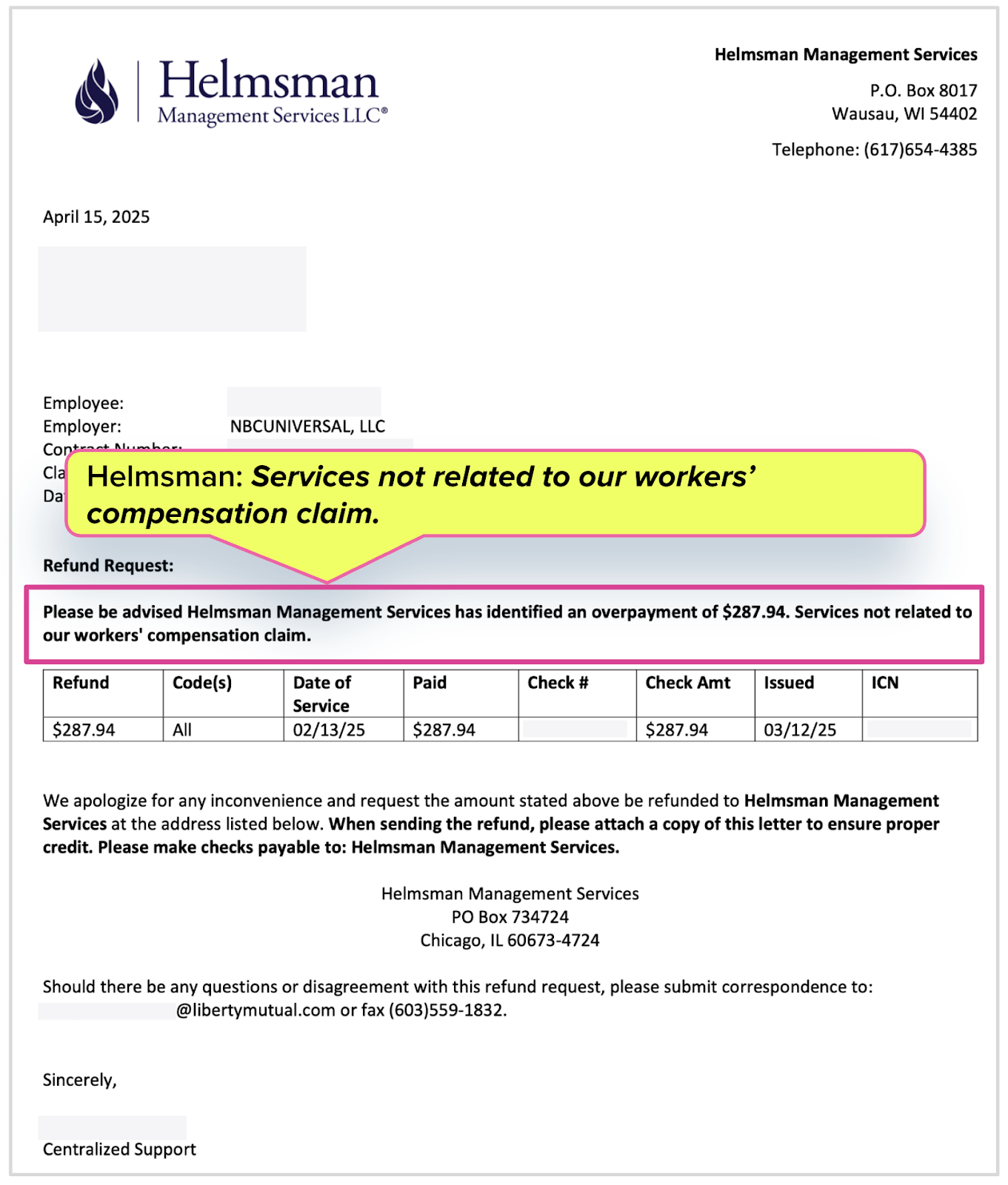
After receiving payment for rendering (authorized) services to the NBC Universal employee, the doctor got the letter below from Helmsman, which claimed that Helmsman “identified an overpayment” to the doctor and demanded a refund of $287.94
Helmsman offered a vague and dubious explanation: “Services not related to our workers’ compensation claim.”
Helmsman’s Story Doesn’t Check Out
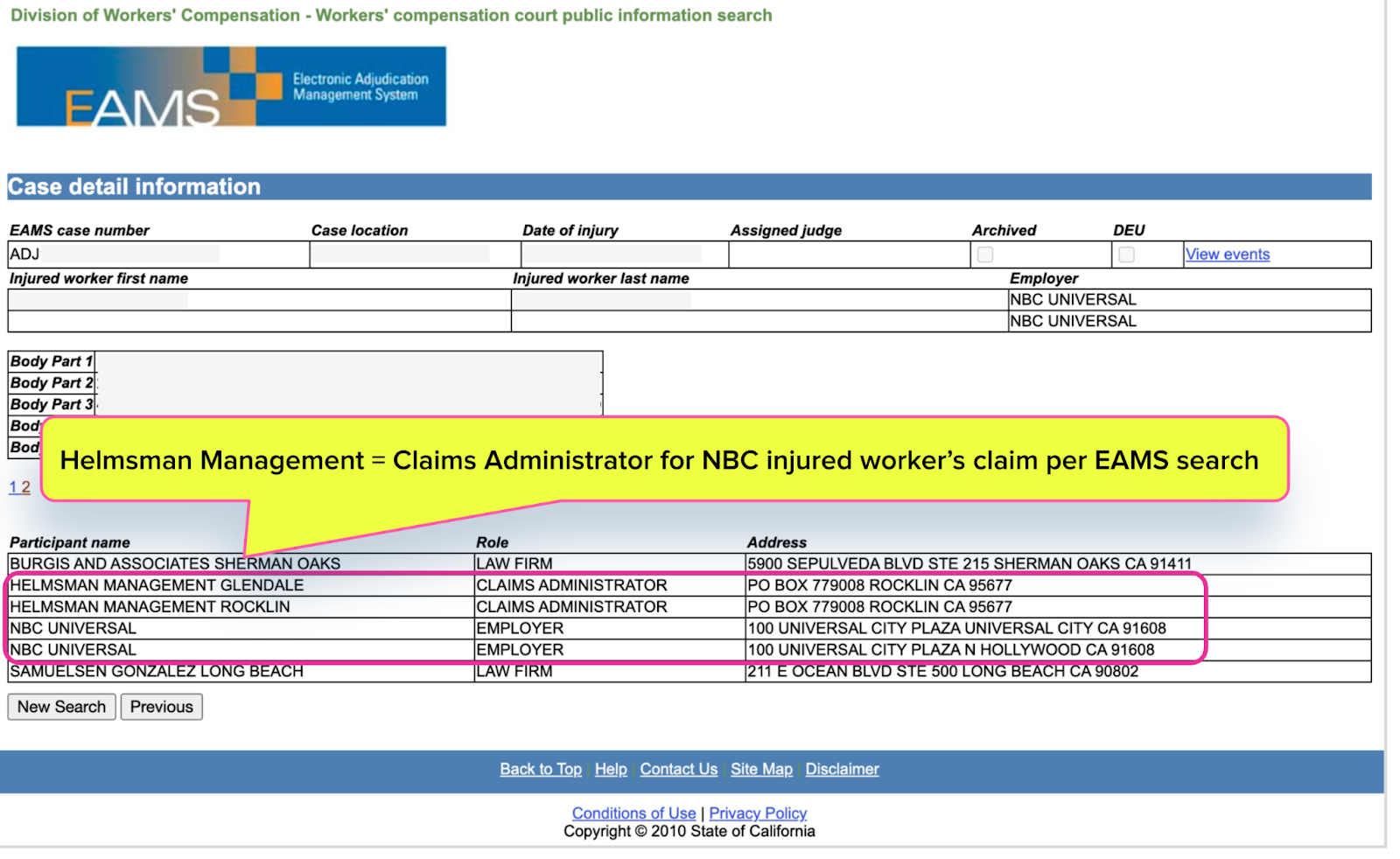
To verify the NBC claim as Helmsman’s, we searched California’s Electronic Adjudication Management System (EAMS), where attorneys electronically file forms and documents on workers’ comp claims with the Workers’ Compensation Appeals Board.
As the screenshot below shows, EAMS confirmed the NBC claim as Helmsman’s…not that there was any doubt.
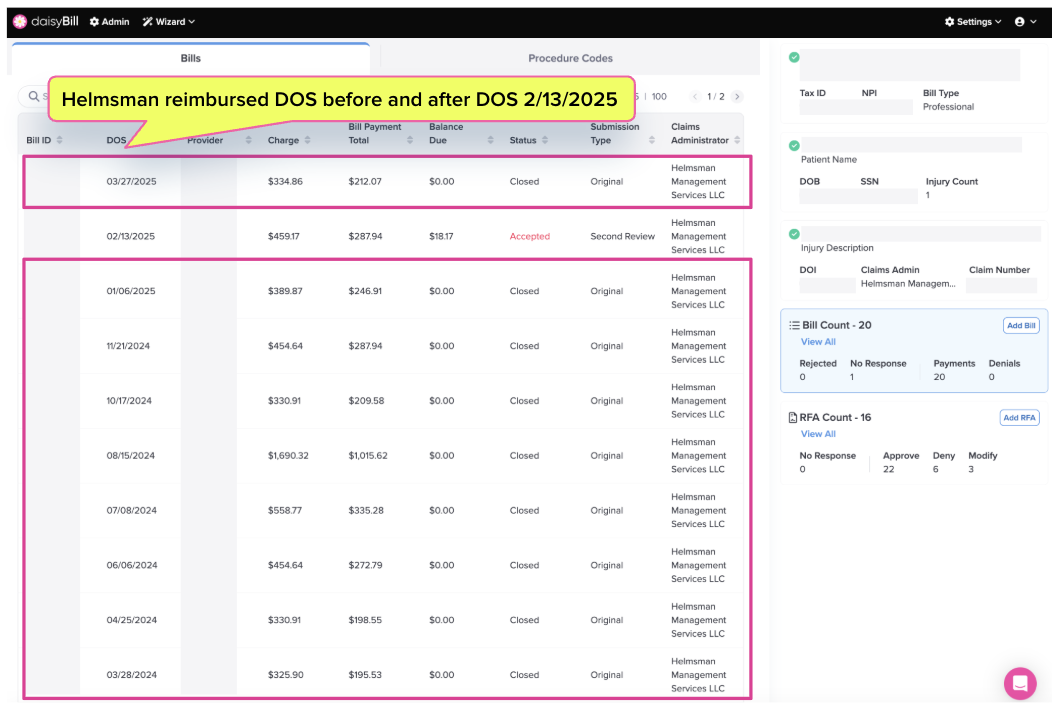
Helmsman Paid 19 Other Bills for Injury Claim
It is even more ridiculous for Helmsman to dispute their management of the NBC claim, considering the injury claim’s bill payment history.
The date of the treatment in dispute was February 13, 2025. The screenshot below from daisyBill confirms that Helmsman paid this doctor for treatment under this exact NBC claim 18 times before that date. And it gets even more absurd—Helsman also paid the doctor for the treatment of this NBC injured worker after paying the bill in dispute.
daisyBill technology offers providers a way to confirm billing history easily. We can’t help but ask: Doesn’t Helmsman have the technology to confirm injury claim payment history?
(Tip to Helmsman: Billing technology might serve NBC better than erroneous letters to doctors demanding refunds.)
(PS - NBC, are you alarmed yet?)
CA: No Refunds for Workers’ Comp Treatment
Helmsman insisted that the provider’s bill was “not related” to any Helmsman claim. We disproved that assertion with state records and the simple fact that Helmsman had paid multiple bills for the disputed injury claim.
But hypothetically, even if Helmsman were correct, it wouldn’t matter.
California law is very clear on the issue of refunds, even for payments the claims administrator made in error (which is not the case here). Providers only have to return funds if:
- The provider and claims administrator have a separate reimbursement contract that specifically requires refunds, or
- If the Workers’ Compensation Appeals Board or a judge issues an order for restitution
In American Psychometric Consultants, Inc. v. Workers' Comp. Appeals Bd. (1995), a California court left no doubt that letting claims administrators take refunds would lead to financial chaos for providers, stating:
“Approving restitution [aka refunds]...would set a precedent which would have unfortunate consequences for the workers' compensation system...No one can operate a business on receipts only conditionally possessed, and medical providers are no exception.”
We advise providers who receive letters requesting refunds to file them immediately under ‘Recycle.’
This doctor shouldn’t have to navigate Helmsman’s bungling, which will ultimately consume practice time and resources. It’s a textbook example of the administrative slog that convinces so many doctors to give up on treating injured workers, shrinking the provider pool for everyone hurt at work.
NBC Universal’s injured employees deserve better claim management than this. California’s injured workers deserve a system that incentivizes provider participation—instead of allowing provider torment.
Keep perfect track of every bill—and make revenue management for workers’ comp a breeze. Click below to see how we make it happen:
CHECK OUT DAISYBILL
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.
.gif)