Orange County/Sedgwick Inflict MPN Mayhem
How much of California workers’ comp dysfunction directly results from the effectively ungoverned Medical Provider Network (MPN) system?
California does not furnish any reliable mechanism for a provider to determine when an MPN applies to an injured worker. Instead, providers must consult (and trust) the claims administrator to identify the applicable MPN.
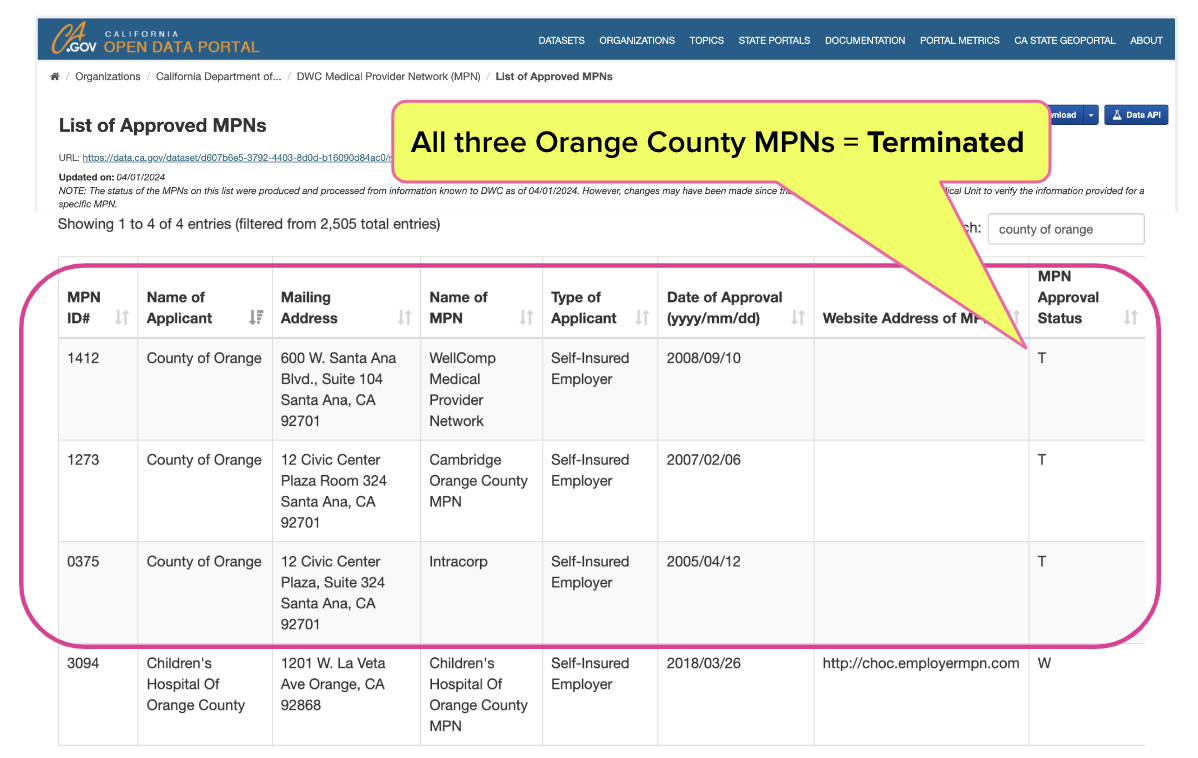
As recently reported, the County of Orange’s Third-Party Administrator, Sedgwick, told a provider that the county’s MPN prohibits telehealth for its employees. The provider checked the Division of Workers’ Compensation (DWC) list of 2,505 approved MPNs, which features three different MPNs listing the County of Orange as the applicant — all three of which are terminated.
When the provider pointed out that Orange County has no active MPNs, Sedgwick claimed that “Wellcomp” was the applicable MPN. Again, the provider consulted the DWC list of approved MPNs, which revealed:
- 130 WellComp MPNs that are currently terminated or withdrawn
- 1 active WellComp MPN with a stated policy of allowing telehealth
This incident exemplifies how California claims administrators use MPNs as justification for treatment restrictions and subsequent threats of payment denial, without providing any evidence that the MPNs cited are valid or applicable.
As this blog has demonstrated on countless occasions, the resulting MPN chaos all but guarantees statewide payment abuse.
Sedgwick Cites MPN to Justify “No Telehealth” Policy
After Sedgwick told the provider that all members of Orange County’s MPN were made aware of the telehealth prohibition, the provider consulted the DWC MPN list. As shown below, all three Orange County MPNs are listed as terminated.
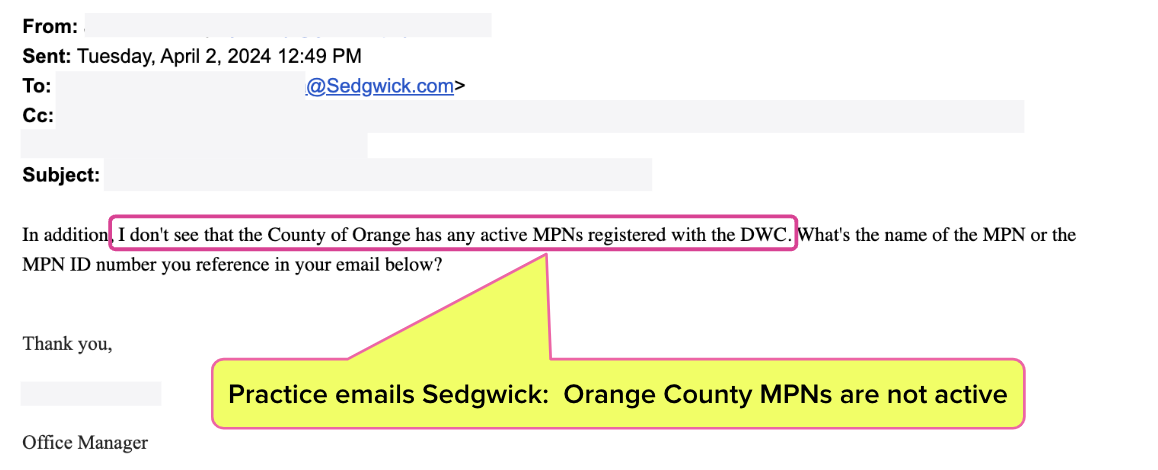
The provider pointed this out to Sedgwick, and requested the specific MPN name and ID number that allegedly applies.
After some back-and-forth, Sedgwick told the provider that “the Wellcomp MPN” applied to Orange County employees, but did not provide an MPN ID number. As we pointed out yesterday, the only active WellComp MPN (MPN ID 2387) has a publicly stated policy of allowing telehealth treatment.
In other words, neither Sedgwick nor Orange County can justify banning telehealth for its injured workers since:
- All Orange County MPNs are terminated
- The only active WellComp MPN allows telehealth
In theory, Sedgwick could deny payment of any bill from any California provider, and cite any of the 2,505 MPN listed by the DWC. Other than a Sedgwick pinky promise, it is impossible for providers (or the public) to confirm whether the WellComp MPN — or any MPN — actually applies to Orange County’s injured workers.
MPN Mayhem
We’d be shocked if this story wasn’t so on-brand for an MPN system gone entirely off the rails.
California is virtually drowning in examples of suspended, terminated, withdrawn, and otherwise defunct MPNs used by claims administrators to justify everything from improper payment denials to delayed treatment to contractual discounts — and now, to justify arbitrary and self-declared treatment restrictions.
Chaos breeds abuse, and the California MPN system is a fertile breeding ground for such abuse. California legislators’ and regulators’ inaction have left business interests better protected than injured workers and the providers who treat them.
daisyBill makes treating injured workers easier, faster, and less costly. Schedule a free demonstration below.
SCHEDULE DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.
.gif)
.gif)


.png)
