Sedgwick Fails to Pay IBR Filing Fee for Zillionth Time
Once more for the cheap seats: when Independent Bill Review (IBR) determines that a claims administrator erroneously denied or adjusted the reimbursement owed to a provider, the claims administrator must reimburse the provider the $180 filing fee the provider paid to request IBR.
It’s a reasonable reimbursement law that California regulators don’t strictly—or remotely—enforce. Instead, providers must plead with claims administrators to return the $180 filing fee or, as recently recommended, implement a Standard Operating Procedure to obtain the $180 reimbursement.
In fact, Sedgwick Claims Management, Inc. violates this IBR filing fee reimbursement requirement so often, we’re forced to use imaginary numbers to estimate the number of times it’s happened (by our count, we’re at just over a zillion).
Sedgwick Overturned at IBR
In November 2022, daisyCollect billed Sedgwick for a Comprehensive Medical-Legal evaluation and diagnostic tests for an Inland Pipe Rehabilitation employee, on behalf of an Agreed Medical Evaluator (AME) client. Sedgwick denied payment for the entire bill.
daisyCollect submitted a compliant Second Review appeal. In response, Sedgwick paid for the evaluation, but not the diagnostic tests. With no other choice, within 30 days of the improper denial, daisyCollect compiled and submitted a 74-page IBR request along with the $180 IBR filing fee.
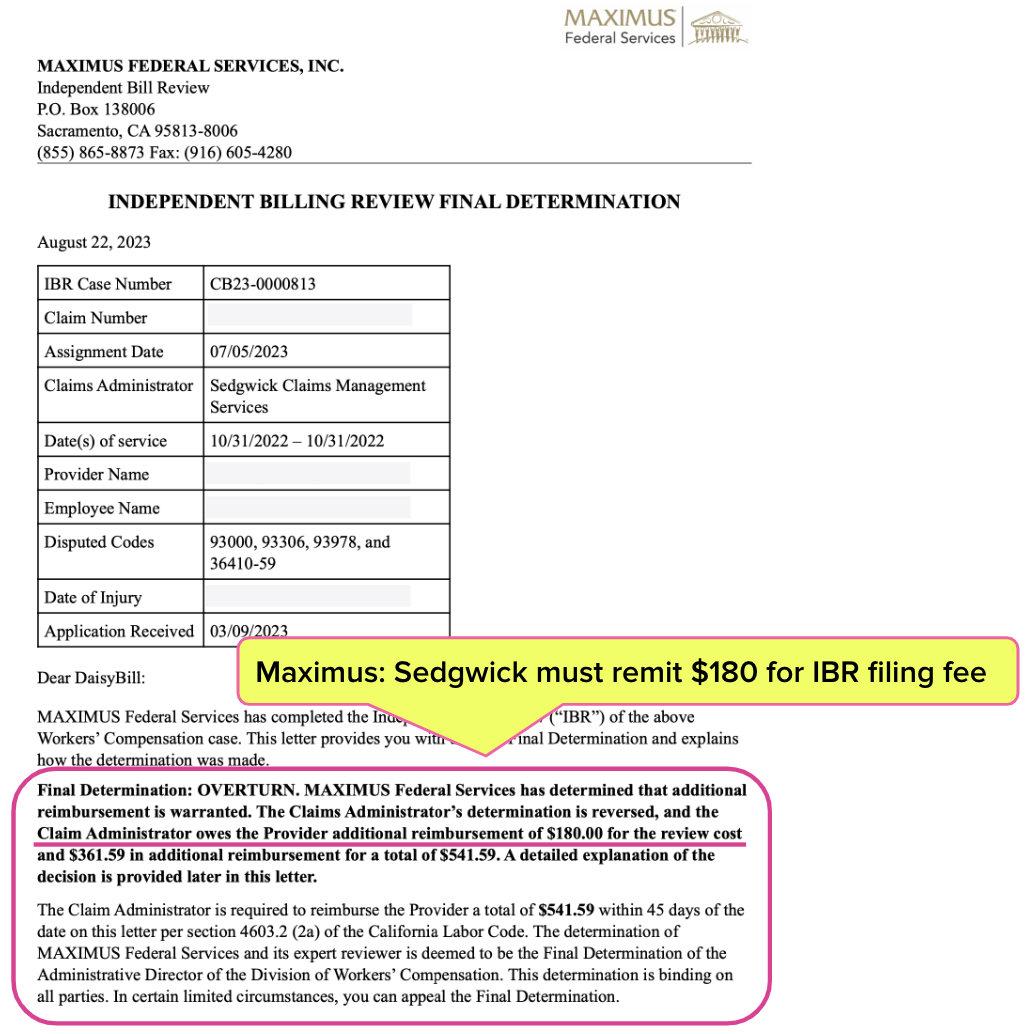
As usual, Maximus (the entity that conducts IBR in California) overturned Sedgwick’s payment denial and ordered Sedgwick to pay the provider the amount owed and the filing fee. Maximus’ August 22, 2023, Final Determination letter is shown below.
And — as usual — Sedgwick “complied” with Maximus by sending the provider the additional reimbursement owed for the diagnostic tests, but failed to reimburse the provider the $180 IBR filing fee as required by California law and ordered in Maximus’ decision.
CA Law Ignored Again
California Code of Regulations Section 9792.5.14 mandates (emphasis ours):
“If the independent bill reviewer finds any additional amount of money is owed to the provider, the determination shall also order the claims administrator to reimburse the provider the amount of the filing fee in addition to any additional payments for services found owing.”
Per California Labor Code Section 4603.2, Sedgwick had 45 days from the date of the Final Determination letter to remit all of the money owed. daisyCollect, per our IBR Filing Fee SOP, contacted the adjuster about the claim and demanded payment.
Finally, on February 1, 2024 — 163 days after Maximus’ ruling, 118 days beyond the deadline to comply with Maximus’ ruling, and 448 days after daisyCollect submitted the original bill — Sedgwick reimbursed the provider the $180 IBR fee.
There are no consequences for Sedgwick’s failure to adhere to California law. Sedgwick acts accordingly. Inland Pipe Rehabilitation and other employers should take note: when your employees and their health care providers are subject to abuse, it’s a terrible look for any company.
daisyBill makes treating injured workers easier, faster, and less costly. Request a free demonstration below.
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.
.gif)
.gif)



.gif)