Sedgwick – IBR Hall of Shame

All too often, insurance companies and claims administrators find unfair ways to deny, delay, and otherwise wiggle out of paying the workers’ compensation reimbursements that they owe doctors.
Like much other payer misconduct, the frequent failure of claims administrators to comply with the mandated California Independent Bill Review (IBR) regulations is a result of a complete lack of consequences for noncompliance. Our latest examples of payment foot-dragging and creative payer excuses feature Sedgwick (again) and Broadspire (next blog post).
For those familiar with workers’ comp, this is an all-too-common and increasingly disturbing story that often goes untold.
Sedgwick Fails as Agent for Falls Lake Fire and Casualty Company
Sedgwick is apparently not overly concerned about paying a provider the $195 fee that was due when the provider prevailed in a recent IBR case. The timeline below demonstrates yet again how the provider must shoulder all responsibility for collecting payment, making multiple phone calls to induce a claims administrator to meet its mandated obligations.
Date |
Action |
Note |
11/14/2019 |
$195 IBR Fee Due |
45-Days after Maximus Final Determination Letter |
11/14/2019 |
Voicemail #1 |
Left VM for adjuster BXXX, saying we received the disputed amount but not the IBR filing fee. Requested a return call. |
12/4/2019 |
Voicemail #2 |
Left VM for adjuster BXXX, saying we received the disputed amount but not the IBR filing fee. Requested a return call. |
12/10/2019 |
Voicemail #3 |
Left VM for adjuster BXXX, saying we received the disputed amount but not the IBR filing fee. Requested a return call. |
12/10/2019 |
Contacted Sedgwick for supervisor info |
Spoke with Sedgwick to obtain supervisor info. Informed that the adjuster is no longer BXXX, but instead is now RXXXXXX. |
12/10/2019 |
Voicemail #1 |
Left VM for adjuster RXXXXXX, saying we received the disputed amount but not the IBR filing fee. Requested a return call. |
1/8/2020 |
Voicemail #2 |
Left VM for adjuster RXXXXXX, saying we received the disputed amount but not the IBR filing fee. Requested a return call. |
1/15/2020 |
Telephone conversation |
Called adjuster RXXXXXX, who said that the check for the IBR Filing Fee went out in early October, but was returned as undeliverable. Sedgwick sent the check to an address in an incorrect city, instead of sending the check to the address listed on the disputed bill. Adjustor reported the check would be reissued tomorrow (1/16/2020) and arrive by next week. |
The Sedgwick claim that it sent the check to the wrong address raises additional questions, as none of the hundreds of pages of documents submitted in an attempt to receive correct reimbursement ever listed an address in that particular (incorrect) city.
It should not take even a single phone call or anything at all apart from Maximus’ letter. But Sedgwick is not the only claims administrator behaving badly.
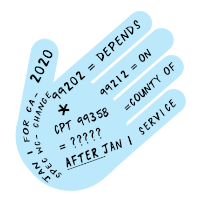
Sedgwick Treats DWC Regulations as Optional
The selective enforcement of the rules of the Department of Workers’ Compensation (DWC) has created a double standard in California. One for claims administrators and insurance companies and another for everybody else. Workers jump through hoops to get basic treatment, while their doctors do the same to get reimbursed. Yet, it is all but optional for claims administrators to correctly reimburse a provider for services rendered to an injured worker.
When a payer incorrectly reimburses a provider, the current California appeals process places the entire burden of correct reimbursement on the provider, imposing strict timeframes and high fees, while the payer suffers no consequences for failing to correctly reimburse the provider.
As an example of the punitive provider consequences, a provider is disallowed correct payment if the provider fails to compliantly complete a single one of the following required steps:
- Submit a Second Review appeal within 90 days of receipt of the Explanation of Review (EOR)
- Submit an IBR within 30 days of receipt of the EOR
- Pay $195 fee to submit the IBR for review by Maximus
- Send the payer a copy of the IBR sent to Maximus
Providers are given no leeway for even the slightest and most innocent error, and none of the myriad excuses used by claims administrators—incorrect address, broken technology, canine hunger—can be used by providers to exempt them from adhering to DWC regulations to the letter.
The example below shows Sedgwick suffering no consequences for failing to reimburse the provider correctly or timely. In fact, the burden fell on the provider to expend even more time and resources to secure reimbursement for the $195 IBR fee.
California’s DWC needs to make changes to address the problem of claims administrators that clearly act as though adhering to the DWC regulations is optional.
Because IBR noncompliance is so common, DaisyBill regularly publishes blog posts highlighting this type of violation (see this post about Liberty Mutual and this post on Tristar). In future, we will be alerting the community to other instances in which claims administrators, bill review companies, and employers engage in this gross non-compliance, in effect cheating providers who have treated injured workers.
Weekly, DaisyBill will encourage change, we will not sit on the sidelines.
DaisyBill offers all the tools a provider needs to bill compliantly--and to appeal effectively, when needed. Our Billing Software includes everything you need for RFAs, bills, and appeals for second review, plus tools for effective IBR requests, including our IBR Decision Library. Schedule a free demonstration today:
SCHEDULE DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.gif)