Sedgwick's UR Obstacle Course Delays Care
.gif)
Welcome to California workers’ comp, where the law requires two doctors to do the job of one:
- A treating physician to heal the injured worker
- A Utilization Review (UR) physician to ration and restrict the care recommended by the treating physician
For all treatment, drugs, diagnostics, and services (essentially everything that costs money), California law requires the treating physician to submit a Request for Authorization (RFA) to the claims administrator for Utilization Review (UR) and approval. This requirement has no exceptions.
Claims administrators enforce this law by denying payment for unapproved treatment. However, there is no adequate enforcement when it comes to issuing compliant UR decisions. Case in point: the extended rigamarole that Sedgwick UR put a doctor through in response to a straightforward RFA.
This UR nightmare included:
- An incomplete UR decision in response to an RFA and 9-page PR-2 report
- A vague request for a peer-to-peer call with an unknown UR entity to discuss…who knows?
The ugly UR details are below.
9-Page PR-2: Not Enough for Sedgwick
The treating physician first submitted a complete, compliant RFA form (shown below) and a 9-page Primary Treating Physician’s Progress Report, or PR-2 report (also shown below).
For an accepted injury, the PR-2 exhaustively detailed the justifications for the requested treatments, which included five specific items: H-Wave treatment (which helped the injured worker sleep through pain), an MRI (to determine the appropriate treatment for the pain), and three medications.
Significant time and practice resources went into the medical evaluation and preparation of the PR-2 report and RFA, aiming to give Segwick more than enough information to make a complete UR decision.
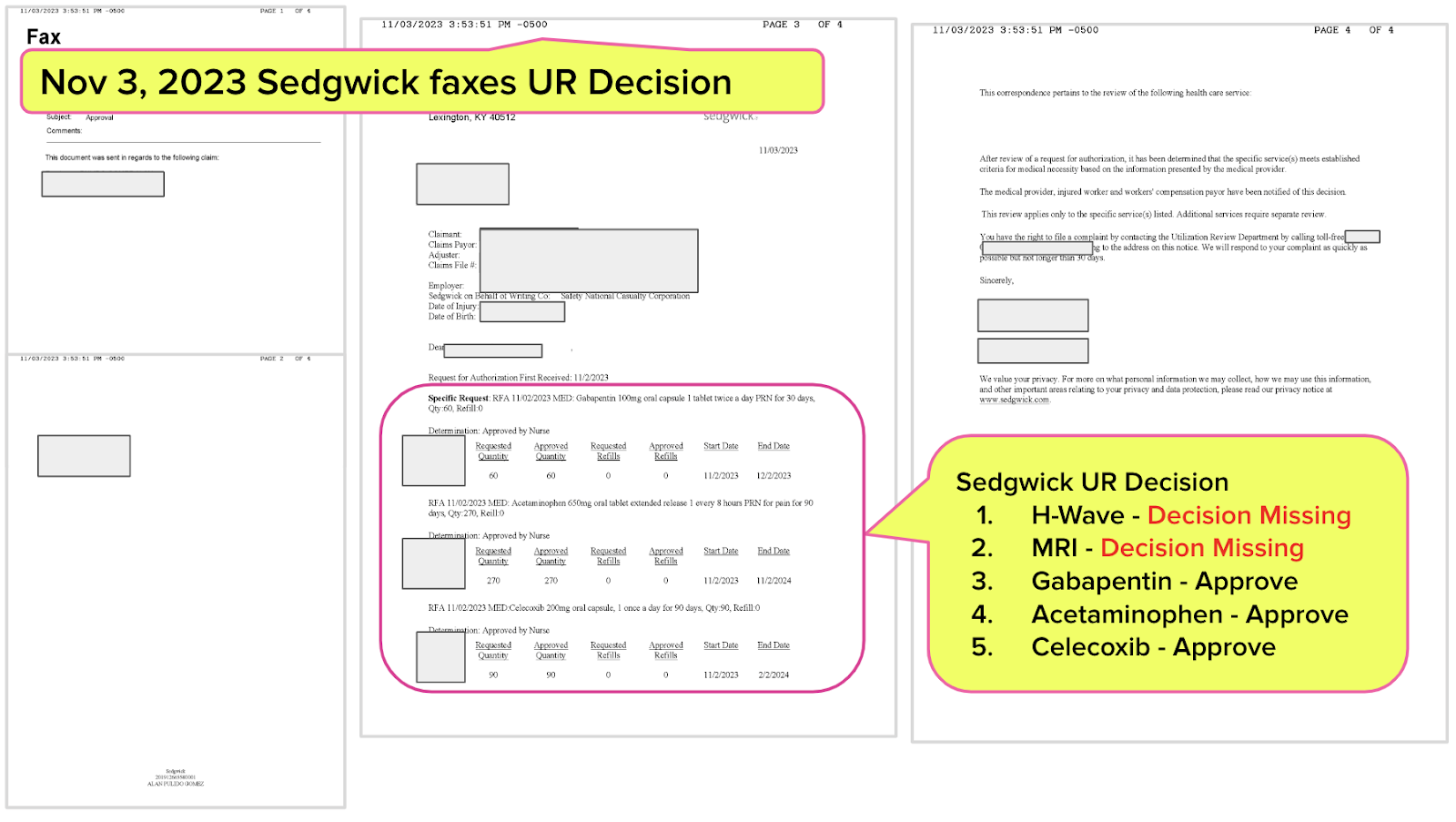
Sedgwick’s Vague, Incomplete UR Decision
Sedgwick’s UR decision (below) approved the three drugs, but did not address the H-Wave and MRI; Sedgwick failed to mention either of these treatments in any way.
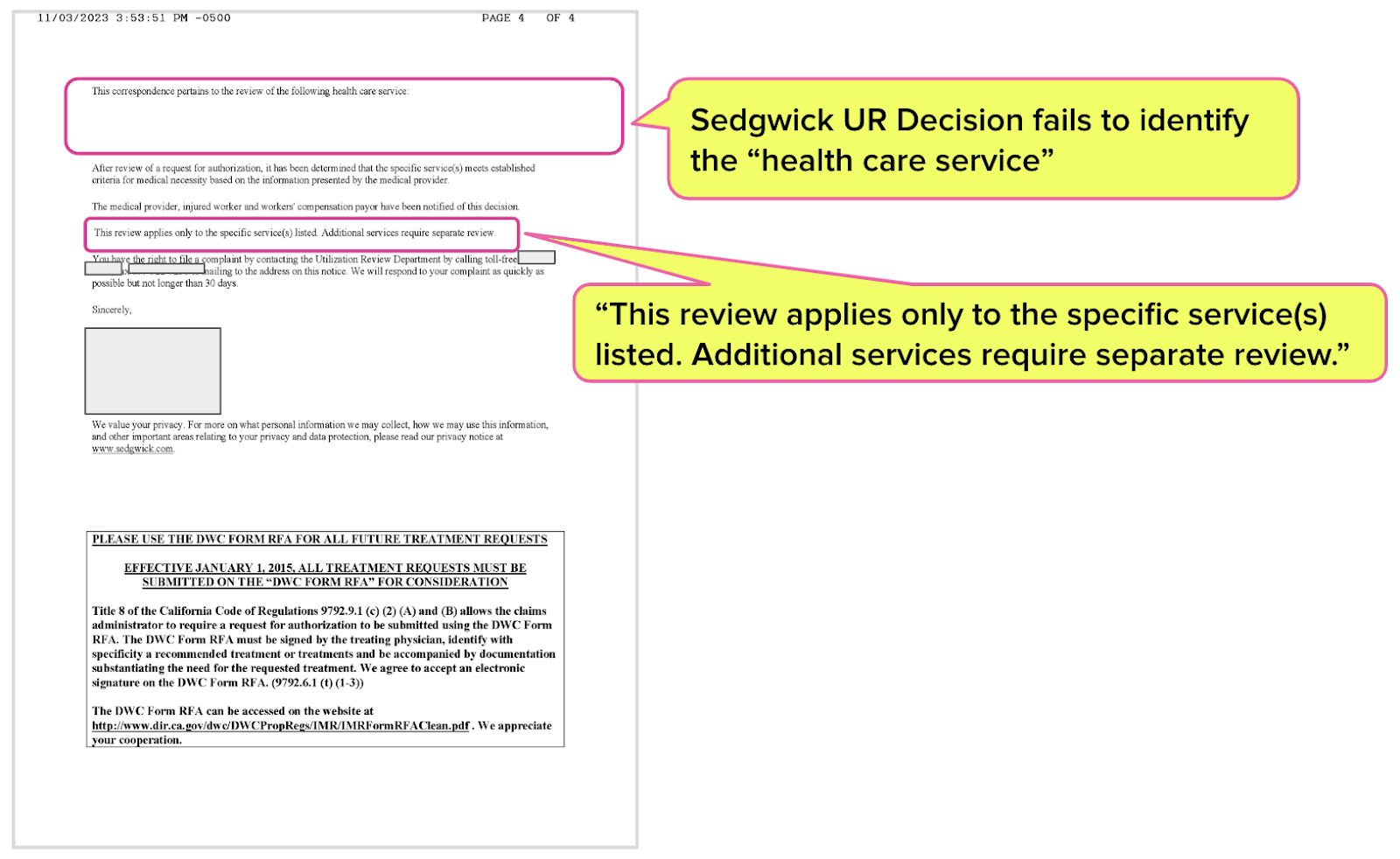
Even worse, the UR decision states, "This correspondence pertains to the review of the following health care service:” — followed by a blank space on the paper.
What can the doctor (or any rational human) make of this?
The Sedgwick UR decision states, “This review applies only to the specific service(s) listed. Additional services require separate review.” However, Sedgwick does not list the “specific service(s),” making it impossible to determine what services might require “separate review.”
This leaves three drugs approved and…no further information. Now what?
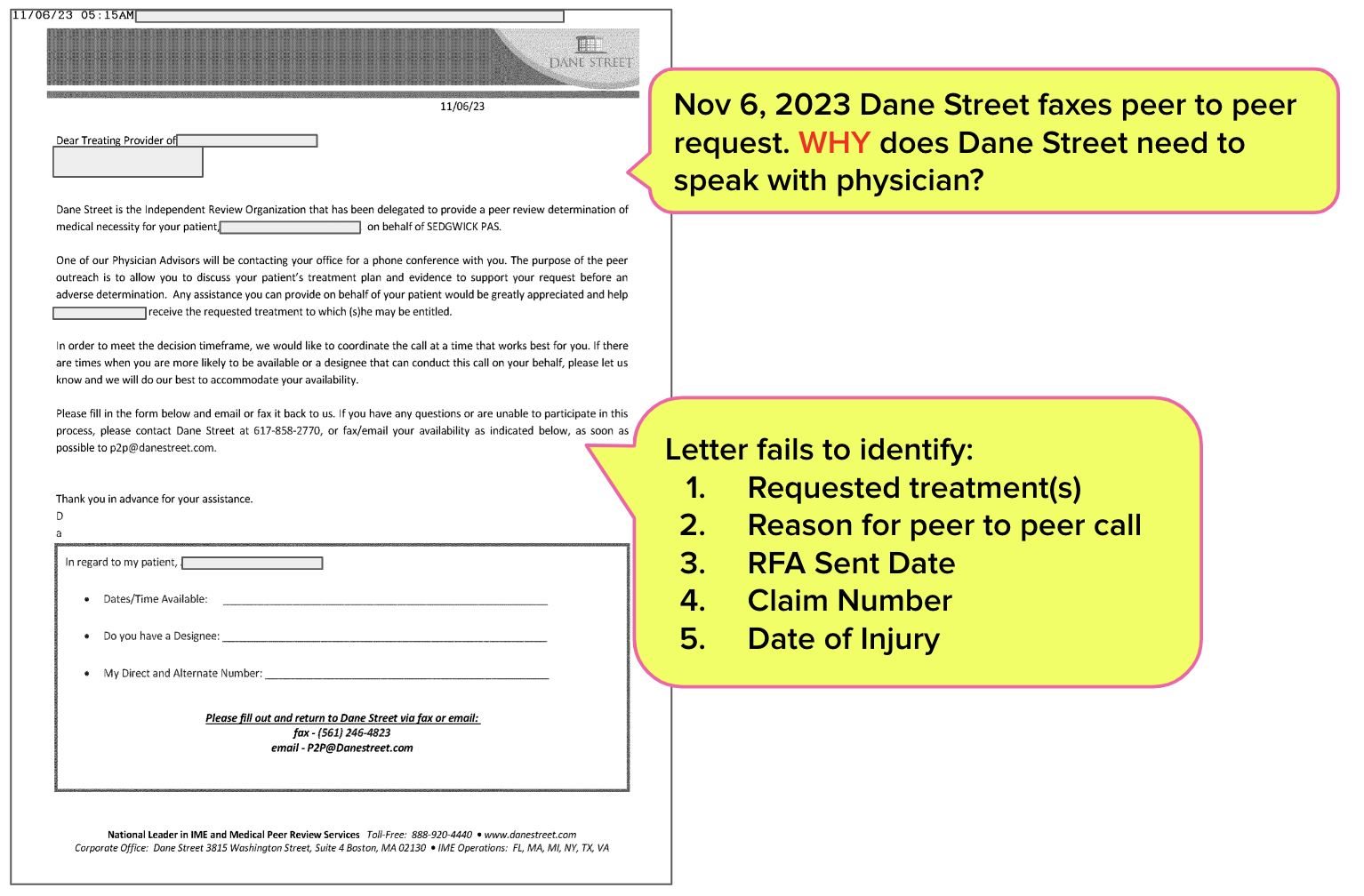
Sedgwick & “Dane Street” Request Peer-to-Peer Call
Somehow, this story gets even weirder.
Following the nonsensical and incomplete UR decision, the doctor received a letter from “Dane Street.” The letter claims that Dane Street is an organization Sedgwick “delegated to provide a peer review determination of medical necessity” for the patient.
No specific reason for the peer review is identified — no reference to the RFA, the claim number, or the date of injury; only the injured worker’s name indicates whom the “review” is about. The letter states:
“The purpose of the peer outreach is to allow you to discuss your patient’s treatment plan and evidence to support your request before an adverse determination.”
Of course, nothing in the letter identifies precisely which treatments are in danger of an “adverse determination.”
The doctor knows only that a third-party “Independent Review Organization” wants them to set aside time in their schedule to chat about…something…on behalf of Sedgwick.
This is yet another case study in how UR in California is a hot-buttered mess — mainly because there are no rules or standardized procedures regarding how claims administrators must respond to RFAs, and seemingly inadequate enforcement of what little standards of UR compliance exist.
While the doctor continues to expend invaluable time and practice resources navigating this unholy UR obstacle course, the injured worker waits, presumably in continued pain.
There’s one way to make UR easier. daisyAuth gives you 30-second RFA submission and automatically tracked UR decisions. Get a demo below!
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.



I'm not sure this is necessarily news, as this happens every day. UR is a bureaucratic sham.
This is exactly what I fear as we pulled out from MPN's. I hope we do not encounter these types of issues. If we do, we may just pull out of treating WC people altogether. I fear we might be in the middle of a non-payment situation right now for no prior auth for treatment as I write this. Even though I sent with the claim the authorization. Preferred Employers Ins has denied for no prior auth. They are making me send SBR-1 (BY MAIL) to them with the needed documentation that had accompanied the claim when it was sent electronically. So now I have to print, assemble the required docs and mail by snail mail for reconsideration for payment.