Stop Faxing! Send Supporting Documents With e-Bills
Provider FYI: If you’re paying an electronic billing vendor, but still using a fax machine (or even worse, a mailbox) to send supporting medical documents, you’re not getting what you paid for.
Many (non-client) providers complain of denied e-bills due to “missing documentation.” That’s because rather than electronically submitting PDFs of supporting documents with each e-bill, these providers fax the documents separately.
When medical documents are sent electronically as PDFs with e-bills, the documents do not get “lost” or go “missing.”
Read on to see how workers’ comp e-billing software should handle supporting medical documents — and why any software product that doesn’t include electronic document submission doesn’t qualify as workers’ comp e-billing technology.
Medical Documents: Required for Workers’ Comp e-Billing
Most states require providers to send workers’ comp e-bills with PDFs of the medical documents substantiating the treatments. Sending this documentation should be as simple as uploading the PDFs to the e-billing software.
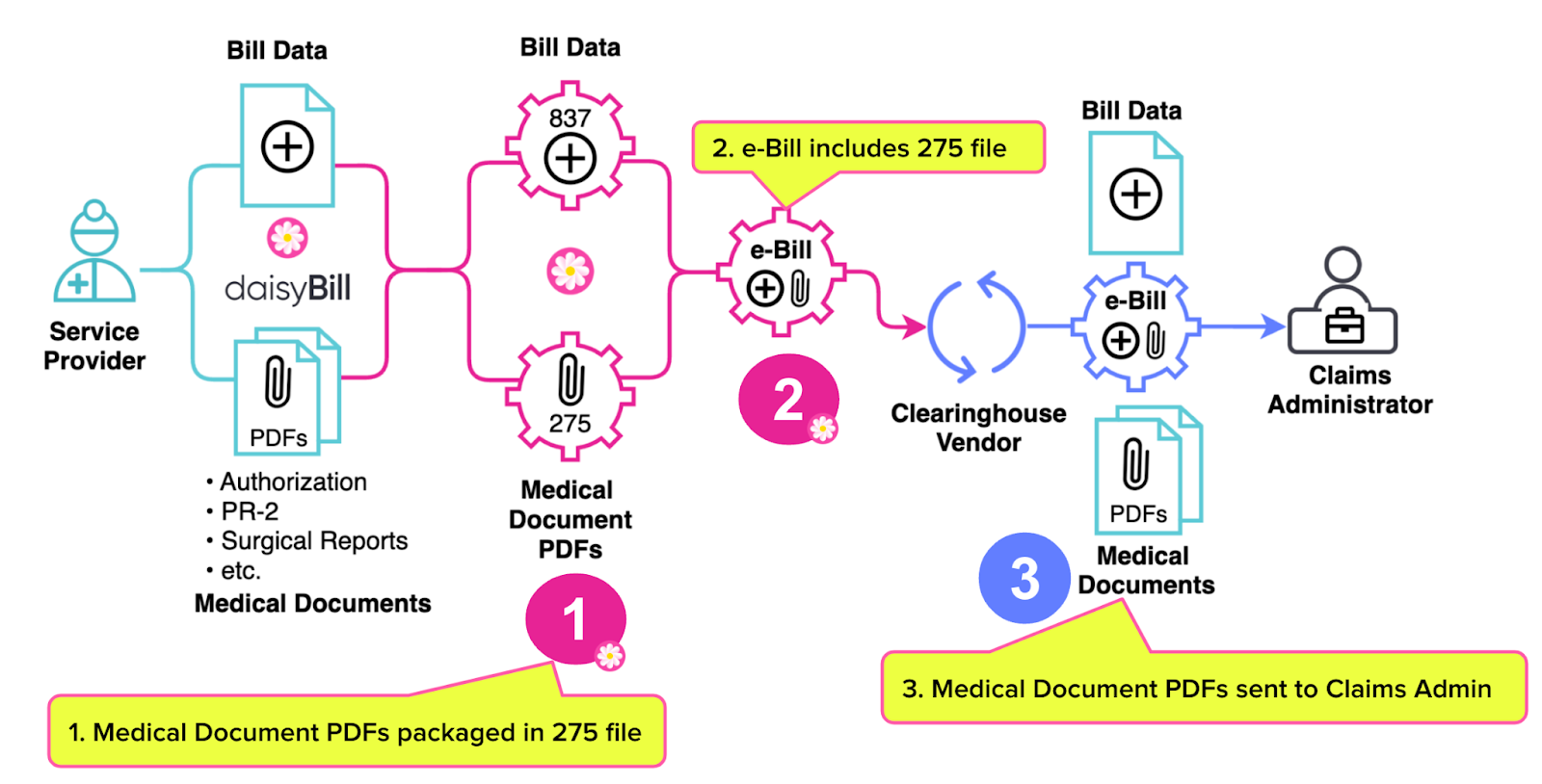
Once the provider uploads the PDFs:
- The e-billing software packages the medical documents into a ‘275’ file.
- The e-billing software sends the 275 file with the e-bill to the clearinghouse vendor used by the claims administrator.
- The clearinghouse forwards the medical document PDFs to the claims administrator.
No faxing is required, ever.
More importantly, submitting PDFs with the e-bill eliminates the possibility of “missing” medical documents, because the provider can prove that 1) the documents were sent and 2) the clearinghouse received the documents.
In the event a claims administrator reports to a daisyBill provider that medical documents are missing, our agents contact the clearinghouse to determine why:
- The clearinghouse failed to transmit the documents correctly, or
- The claims administrator failed to receive the documents.
Tracking down supposedly “missing” documents is never a daisyBill provider’s responsibility. Never.
Workers’ comp providers who do not use daisyBill often report payment denials resulting from supporting documents getting lost in the mail, or PDFs lost due to the inability of standard group health e-billing software to attach and transmit these documents correctly.
This missing documents problem is extremely common, and one of the top reasons workers’ comp providers abandon e-billing and revert to slow, expensive paper billing. But it’s not a problem for daisyBillers.
Secure Document Transmission Explained (With Video)
When a practice staff member imports or enters billing data into daisyBill, our software automatically prompts the provider to upload PDFs of the required supporting documents. daisyBill packages the PDFs into a 275 file, accepted by most clearinghouses (and by payers that do not use a clearinghouse).
Important note: daisyBill also transmits the e-bill and documents to the specific clearinghouse hired by the payer where applicable, avoiding the sloppy rerouting of files caused by software that sends all bills and documents to a single clearinghouse.
Both the bill file (in ‘837’ file format) and the document file (in 275 format) are assigned the same unique “attachment control number.” This allows the clearinghouse to match the bill file (837) with its corresponding document file (275). The attachment control number ensures that the bill arrives with its documents.
With the correct submission of supporting documents, the promises of workers’ comp e-billing comes to fruition. The provider gets paid faster, treating injured workers becomes more manageable, and workers’ comp becomes a better financial proposition.
daisyBill makes workers’ comp billing easier, faster, and less costly. Request a free demonstration below.
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.





This just makes me shake my head to these Insurance companies. My recent experience.......This is the response I got from the adjuster in regard to a denied bill for reduction code 197: Precertification/authorization /notification absent. The bill was sent electronically with all the attachments........The adjuster said, "I reached out to our bill review company, after looking at the claim they confirmed it was a HUMAN error where the reviewer missed the preauthorization in between the medical notes. They have re-reviewed it and allowed payment and once it hits my desk I will authorize payment." Once again, I am so sorry for the mistake and thank you for bringing it to my attention."
We have successfully broken the ties of PPO reductions, with the help of Daisybill and all the wonderful topics you post. The feeling I get when I see a real payment come in for treating an injured worker at the amount we are entitled to, (again thanks to Daisybill Work Comp Calculator), it gives satisfaction that we are now being paid for treating injured workers and not losing revenue every time we treat one. Shout out to Daisybill for sharing all these situations with help for providers to help themselves! Thank you Daisybill!!