Why Specificity Matters: ICD-10 Billing for Workers’ Comp
On October 1st, both the U.S. health system and the California Division of Workers’ Compensation officially adopted ICD-10 diagnosis codes.
Specifically, the California Division of Workers’ Compensation Medical Billing and Payment Guide, Section 3.0 (a)(2) states that:
Although ICD-10 coding is required on or after October 1, 2015, for a twelve month period ending October 1, 2016, no medical treatment shall be denied based solely on an error in the level of specificity of the ICD-10 diagnosis code(s) used.
But what exactly does “specificity” mean?
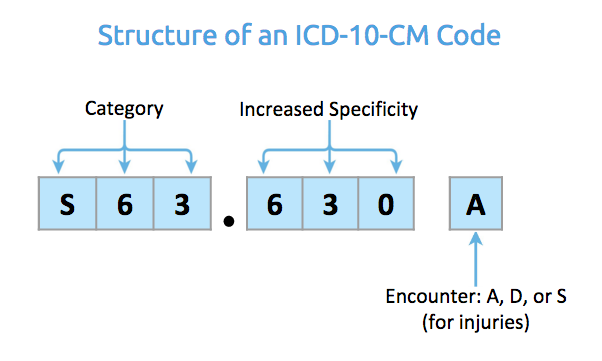
Take a look at our breakdown of the structure of an ICD-10-CM code.
An ICD-10-CM code is anywhere from 3 to 7 characters. The more characters present, the higher the level of specificity.
The first three characters of an ICD-10-CM code indicate the diagnosis category and the affected body part. In the example above, for characters 1-3:
- “S” indicates an injury.
- “S6” indicates an injury to the wrist, hand, and fingers.
- “S63” indicates a dislocation or a sprain to the wrist, hand, and fingers.
The second set of three characters offer further specificity about about the diagnosis: etiology, severity, laterality, and other important details that make the diagnosis even more specific. In example above, for characters 4-6:
- “S63.6” indicates an “other and unspecified” sprain.
- “S63.63” indicates a sprain of the interphalangeal joint.
- “S63.630” refers to a sprain of the interphalangeal joint of the right index finger.
Finally, the last character indicates whether the treatment was for an initial encounter, a subsequent encounter, or sequela (a complication that arises as a direct result of a condition). In the diagnosis example above:
- “A” indicates a diagnosis for an initial encounter.
Although the ICD-10 diagnosis codes guide may indicate a higher level of specificity is required, denial of a medical treatment bill based on a lack of ICD-10 code specificity is not allowed.
For California workers’ comp billing, an incorrect 4th, 5th, and 6th character--the part of the ICD-10 code that indicates increased specificity--cannot lead to a denial of a bill for treatment until October 1st, 2016.
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.