Albertsons Employee's Post-Amputation UR Nightmare

Two days before Christmas in 2022, an Albertsons Companies employee suffered “traumatic amputations” of three toes in a work accident. This worker lived alone on the third floor of a building without an elevator.
Following the amputations, on January 18, the treating physician submitted a Request for Authorization (RFA) recommending that Albertsons provide temporary home health assistance (4 hours daily for 30 days) to help the worker with the necessities of life.
Albertsons’ Utilization Review Organization (URO), EK Health, denied the request for home health care, citing a lack of medical necessity — despite the worker’s living situation, which presented obvious challenges for the injured worker, particularly when getting in and out of their home.
As billing experts and not physicians, we cannot make determinations of medical necessity or appropriateness. But as empathetic humans, we can’t help but ask aloud how Albertsons expected this injured worker to navigate their day-to-day life without at least some assistance.
MD Requests Home Health Care, Albertsons Denies
In the course of work at a warehouse, the worker’s foot was run over by a pallet jack, resulting in:
- Complete traumatic amputation of the great toe
- Complete traumatic amputation of one lesser toe
- Partial traumatic amputation of one lesser toe
- Contusion of the foot
The treating physician requested daily home health for only 30 days while the injured worker recovered from the traumatic amputations.
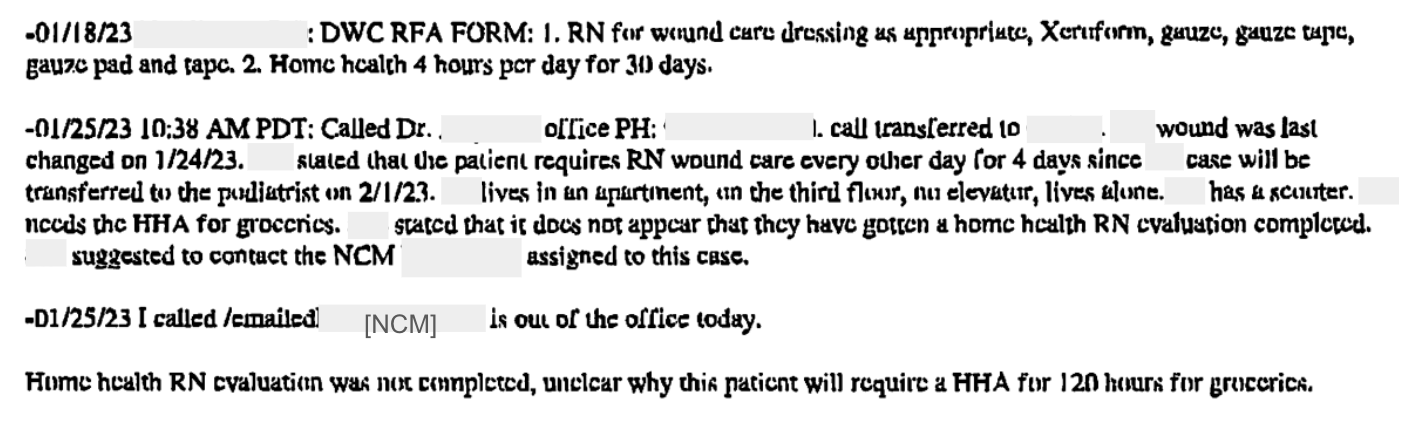
According to the UR decision issued by EK Health on behalf of Albertsons, the UR reviewer called the physician on January 25 — which was the due date of the Albertson UR decision. The physician was unavailable, so the reviewer spoke to an individual at the office.
This exchange reported in the UR decision reveals that the physician’s representative told the reviewer that the injured worker “lives in an apartment, on the third floor, no elevator, lives alone. [Worker] has a scooter.”
Below is the exchange reported by the reviewer (pardon the illegibility of EK Health UR decisions).
After failing to speak with the nurse case manager (NCM), the EK Health reviewer denied the request for home health care, stating that it was “unclear” why the injured worker needed the home care for “120 hours for groceries.”
Essentially, the reviewer used a comment about groceries by a non-physician representative to deny assistance to an amputee. Moreover, if Albertsons’ and EK Health’s objection to the request is the number of hours, why not modify the requested treatment to reduce the hours?
UR Decision Cites MTUS Justifying Home Health Denial
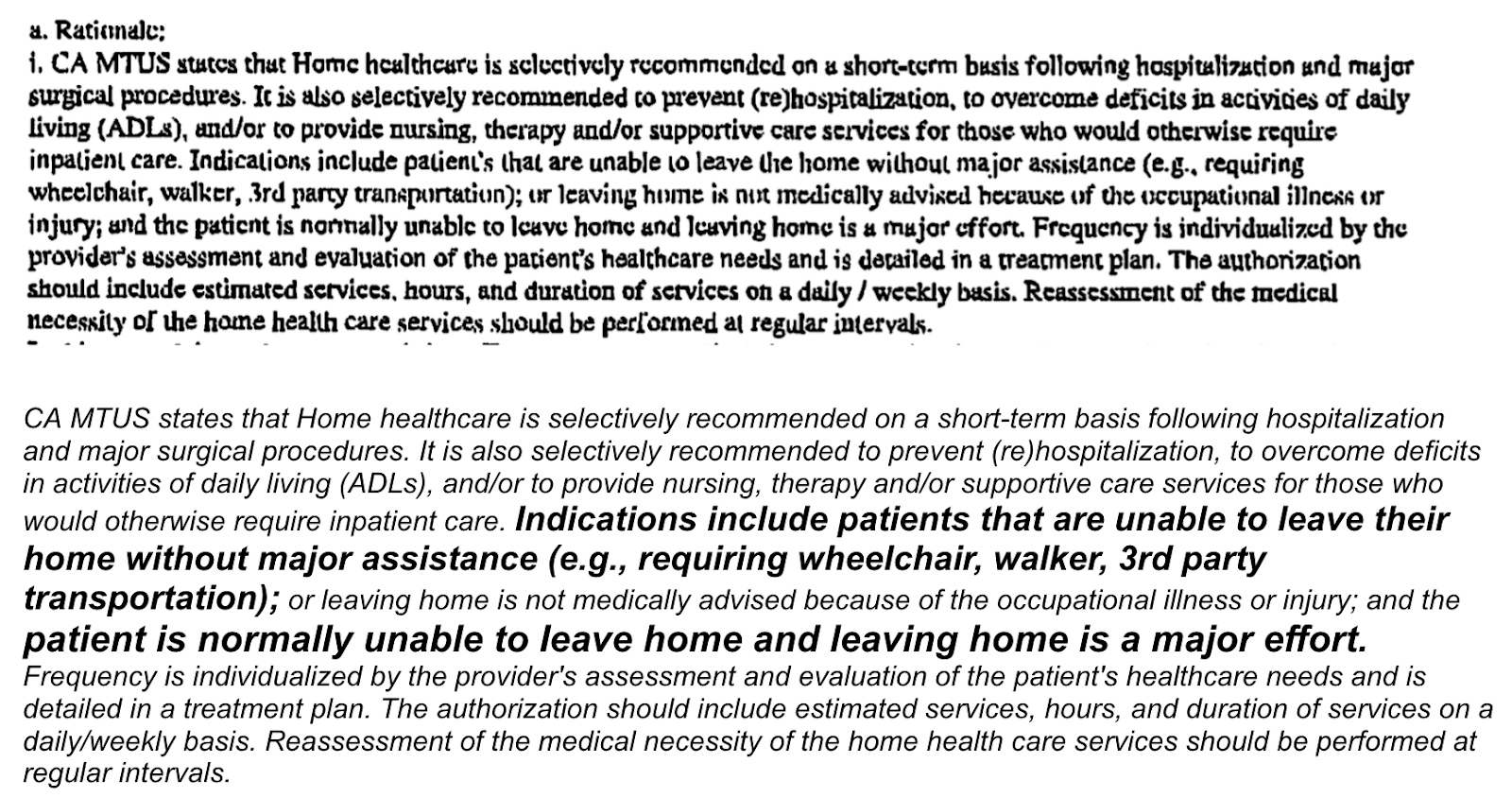
EK Health sent the physician a UR decision citing the following 2017 guidelines, which the URO used when determining that home healthcare was not medically necessary.
The CA MTUS guidelines EK Health cites describe criteria for home health care that, to all appearances, the injured worker may have met. Below is the faxed UR decision’s rationale for denial, followed by our more legible transcription (with emphases added).
According to the MTUS that EK Health provided in the UR decision, home health care is recommended to overcome “deficits in activities of daily living,” with indications specifically including an inability to leave the home without “major assistance.”
It is hard to argue that the loss of multiple toes for someone living alone in a third-floor walkup using a scooter does not meet this description.
By way of preventing fraud or overtreatment, claims administrators and their UROs may be inclined to deny treatment reflexively or to limit care as much as can be justified under treatment guidelines. Laws and regulations designed to err on the side of saving claims administrators money can create obstacles and lay miles of red tape between injured workers and the care they need.
Injured workers ultimately pay the price for this climate of suspicion — and decisions like this do little to discourage the perception that cost control outranks recovery in the brutal arithmetic of UR.
Further, lax regulatory oversight of UR decisions allows claims administrators to improperly deny or delay treatment with little (read: zero) threat of penalty. Either way, California’s injured workers are at the mercy of a deeply flawed UR system.
Submit RFAs in 30 seconds and automatically track UR decisions with daisyAuth. Request a demo below!
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.gif)



