CA Appeals: Sutter Health Pays for Frankenreport
In our previous article, daisyNews detailed how Sutter Health authorized a California provider to create a strange combination of a Permanent and Stationary (P&S) report and a Medical-Legal evaluation report. Sutter agreed to reimburse the provider “at the medical-legal rate” for this odd (and legally suspect) document.
Subsequently, Sutter Health refused to pay the provider's $8,942 bill, inaccurately citing “insufficient documentation.” Fortunately, this provider is a client of daisyCollect, which immediately submitted a Second Review appeal. Sutter Health paid the appeal within three days of receipt.
While technically, this tale has a happy ending, it is actually a critical warning for California providers.
California law essentially incentivizes claims administrators to deny payment reflexively for any reason, false or legitimate. If this provider failed to send a timely or compliant Second Review appeal to dispute the denial, Sutter Health would owe the provider exactly $0. By denying payment for these authorized services, Sutter Health stood to save almost $9,000.
Many California providers (and interpreters) are unaware of the imperative of appealing improper denials or lack the tools to do so efficiently—and claims administrators like Sutter Health can profit handsomely.
Payment “DISALLOWED”
As explained in our previous article, Sutter authorized the provider to prepare a report that was neither a P&S nor a Medical-Legal report but a strange mashup of the two. Moreover, the provider was not eligible to furnish either of those reports.
Still, Sutter Health authorized the report with “payment at the medical-legal rate.” However, Sutter Health subsequently denied the provider’s bill, claiming they didn’t receive the documentation necessary to review it.
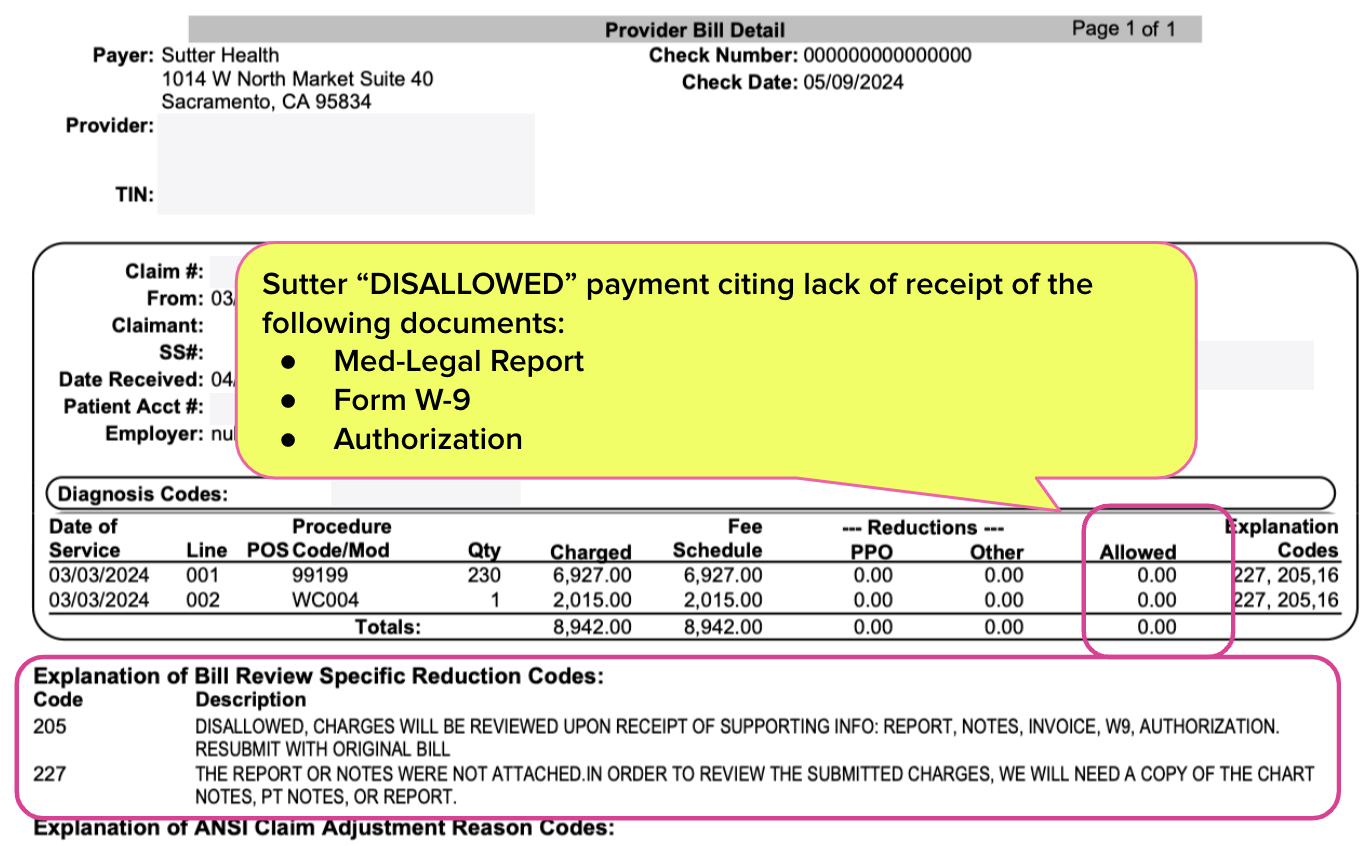
As shown in the EOR below, Sutter Health “DISALLOWED” the charges for failure to submit the supporting report, a W-9 tax form, and proof of authorization.
Proof Sutter Received Documents
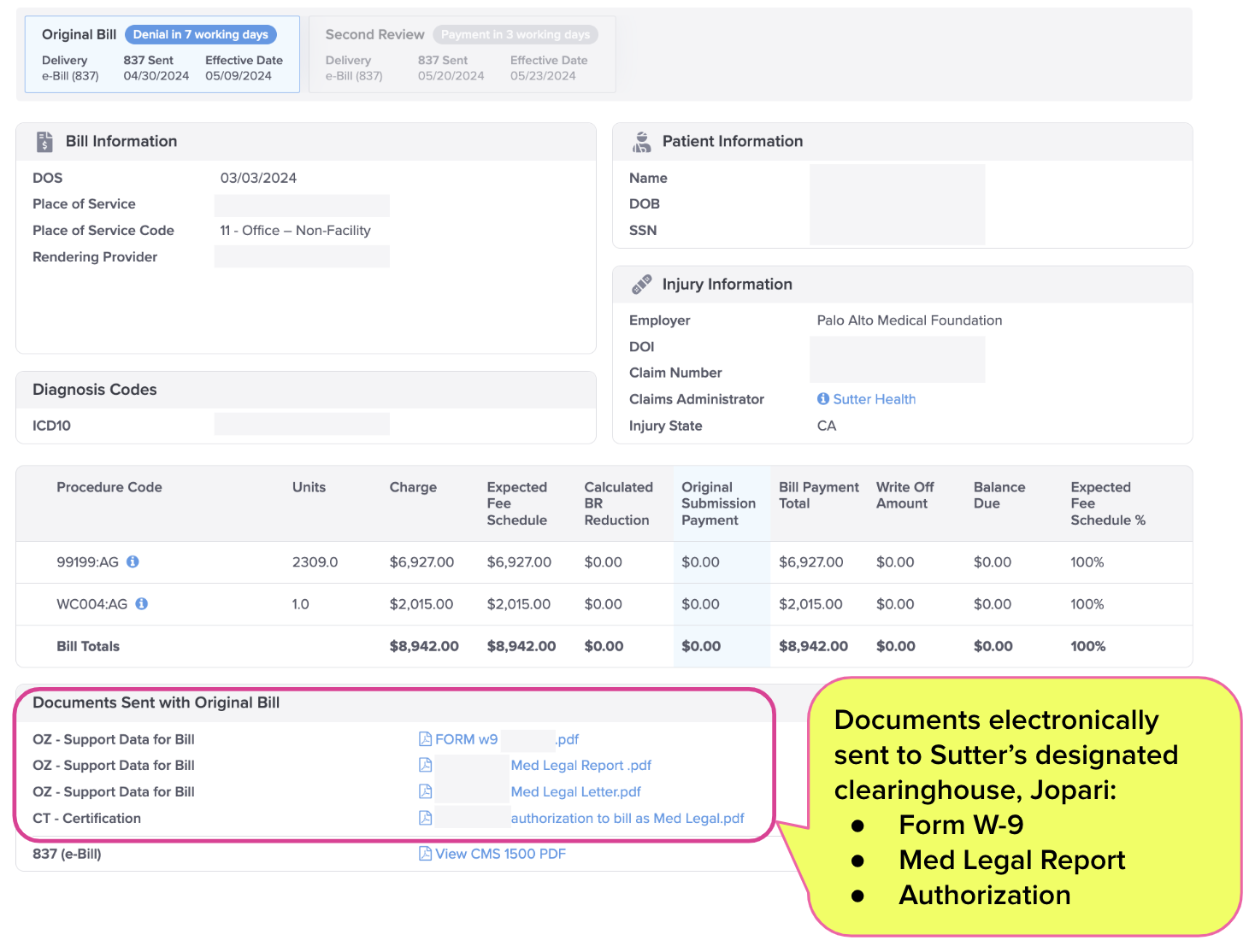
Sutter Health’s claim of missing documents was as wild a contortion as the Frankenreport they authorized. daisyBill sent the provider’s e-bill directly to Sutter Health’s designated clearinghouse, Jopari, using the assigned payer ID number. As with all e-bills submitted using daisyBill, all required documentation was attached.
The screenshot below shows that the provider sent Sutter Health the exact documents alleged to be missing.
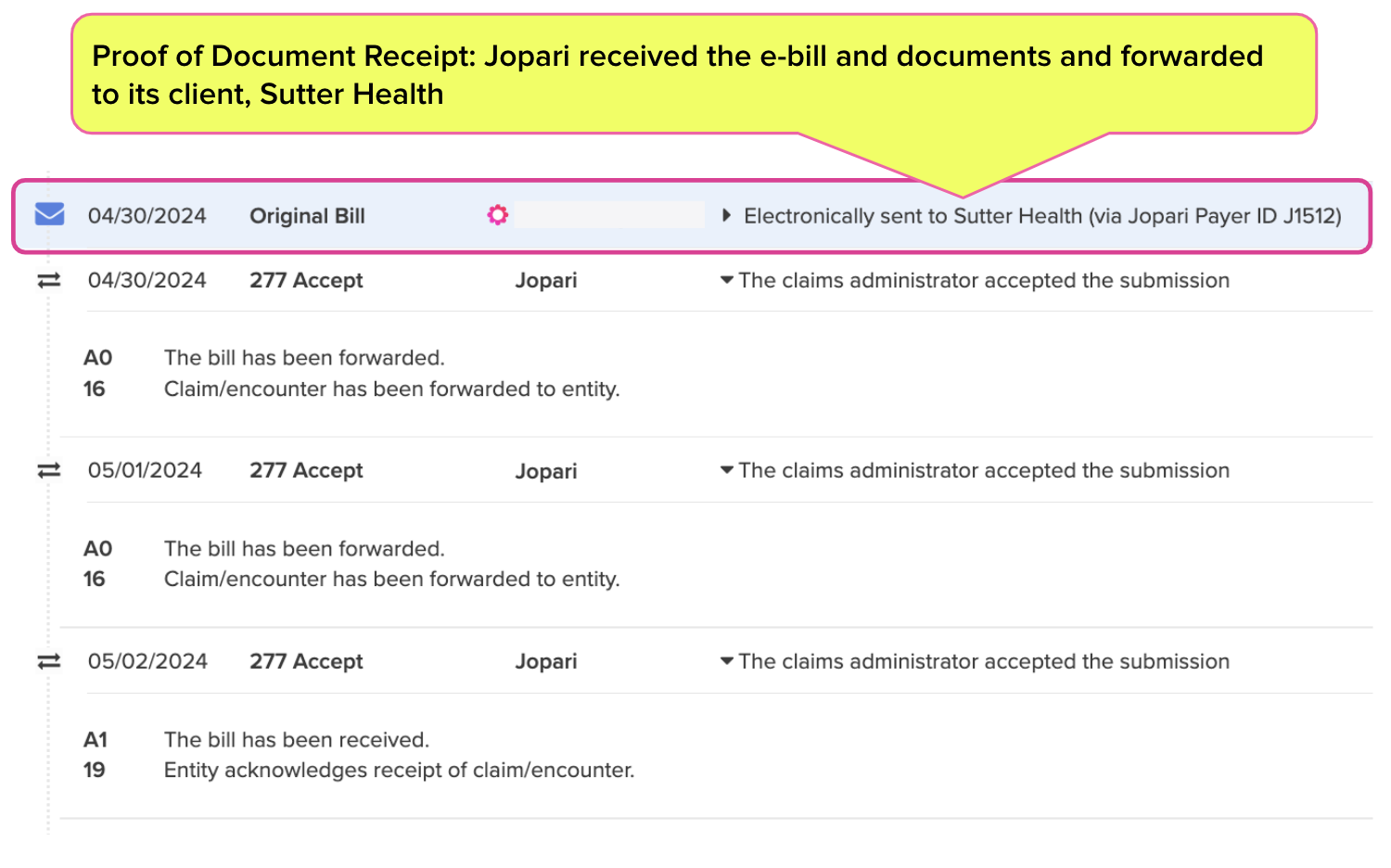
The Bill History (screenshot below) clearly indicates Jopari, as the designated clearinghouse, accepted the e-bill and documents on Sutter Health’s behalf. Jopari sent daisyBill a ‘277 Acknowledgement’ indicating Jopari forwarded the e-bill and documents to Sutter Health.
In this case, Sutter Health ultimately did the right thing and paid the bill upon Second Review.
However, too many providers fail to exercise their right to appeal improper payment denials, because they lack either the knowledge or the resources and technology to do so efficiently.
Essentially, California law monetarily incentivizes claims administrators to deny bills improperly. If the provider fails to follow the mandated appeals process or makes any mistake along the way, the claims administrator owes nothing.
Providers (and interpreters) must be aware of this payment dynamic and act accordingly to protect their practices.
Med-Legal billing requires specialized expertise. daisyCollect pros use our advanced software (and years of experience) to protect your practice. Schedule a demo below:
SCHEDULE DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.gif)

