CA UR: AmTrust & Genex Deny Care With ODG (Again)
What suffering must befall injured workers before California bothers to enforce its meager Utilization Review (UR) requirements?
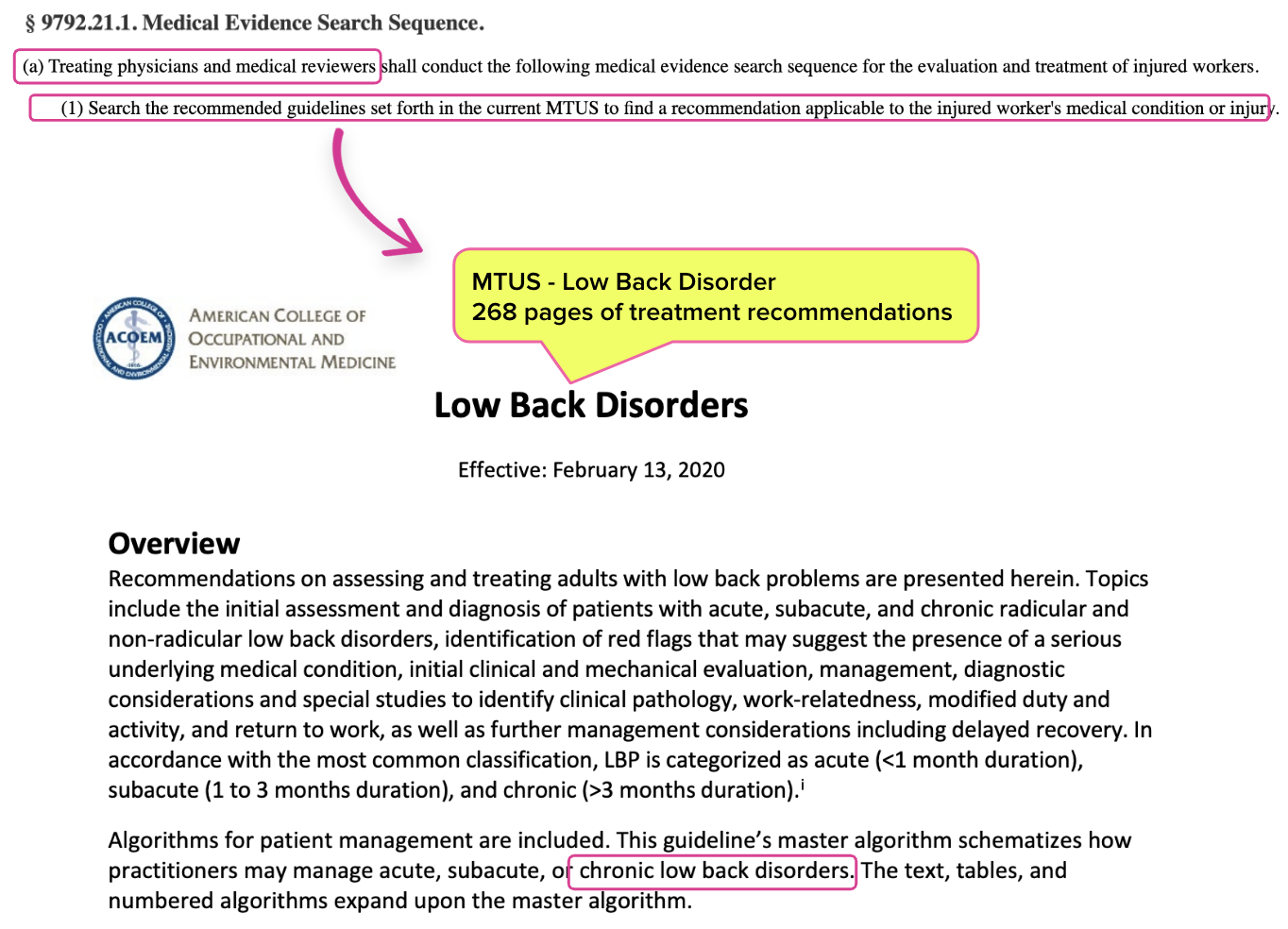
When considering which treatments are necessary and appropriate for injured workers, treating physicians and UR physicians are required by state law and regulations to consult and adhere to the recommendations listed in the Medical Treatment Utilization Schedule (MTUS).
Per California workers’ comp regulations, UR physicians may refer to non-MTUS guidelines “In the limited situation where a medical condition or injury is not addressed by the MTUS…”
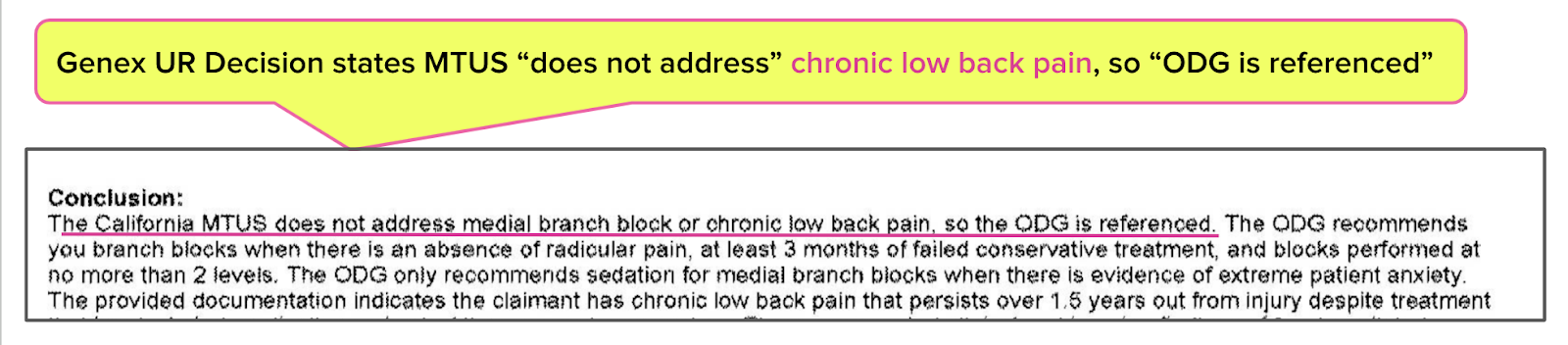
However, AmTrust and its URO, Genex, disregarded the MTUS and cited the “Official Disability Guidelines (ODG)” to deny physician-recommended care. As justification for citing the ODG, Genex incorrectly claimed that the MTUS does not address chronic low back pain.
Just as shockingly, AmTrust and Genex also failed to apply the ODG correctly, denying care that the ODG (though inapplicable) recommends.
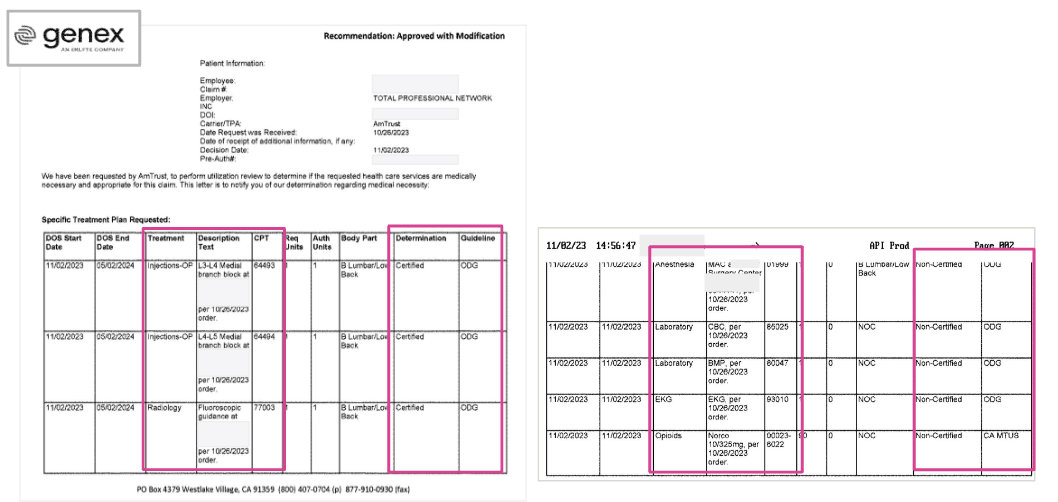
Below, see the harrowing example of an injured worker with multiple risk factors whom AmTrust and Genex approved for surgery but denied preoperative care and anesthesia services — all based on incorrect applications of the inapplicable ODG.
1. MTUS Addresses Low Back Injuries, ODG Irrelevant
As shown in the AmTrust/Genex UR decision below, the California-licensed UR physician reviewer asserted that the MTUS does not address the injured workers’ chronic low back pain. As a result, the physician reviewer claimed the right to refer to the ODG when approving or denying the treating physician’s recommended care.
MTUS - 268 Pages of Low Back Disorder Guidelines
As shown below, the MTUS addresses low back disorders, including chronic low back disorders. California Code of Regulations Section 9792.21.1 clearly states that the MTUS is the only guideline California physicians (treating or UR) may consult for this injured worker:
- “Treating physicians and medical reviewers” must consult the MTUS when considering any treatment.
- “In the limited situation where the MTUS does not address a medical condition or injury…” the physician may look to other guidelines.
Accordingly, the Genex physician reviewer should not consult the ODG or other guidelines when approving or denying the treating physician's recommended care.
However, Genex’s UR decision (below) cites the ODG to deny several treatments, including monitored anesthesia and pre-operative clearances.
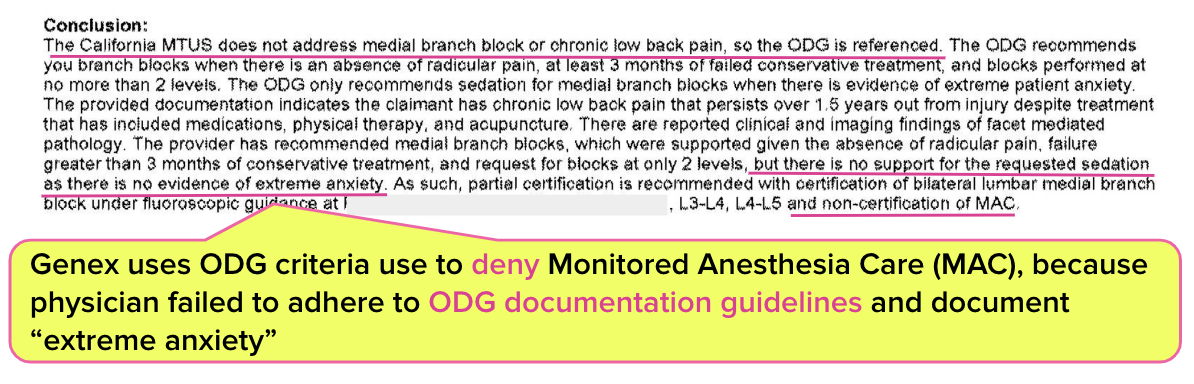
2. Genex Denies Monitored Anesthesia
As acknowledged in the UR decision, the injured worker is a 69-year-old suffering from comorbidities including “advanced age, cardiac disease, hypertension, depression,” and other medical issues.
One may assume the treating physician, who is most intimately familiar with the worker’s physical and emotional condition, is best positioned to determine whether a service like Monitored Anesthesia Care (MAC) is warranted when performing a procedure on their patient.
Yet Genex denied MAC because the (inapplicable) ODG only allows for MAC in this scenario when “extreme anxiety” is documented.
Putting aside whether it’s wise to countermand a treating physician’s anesthesia recommendation for an elderly patient in marginal health (once more for the cheap seats), California adopted the MTUS guidelines, not the ODG. There was no reason for the treating physician to support their anesthesia recommendation with respect to ODG standards.
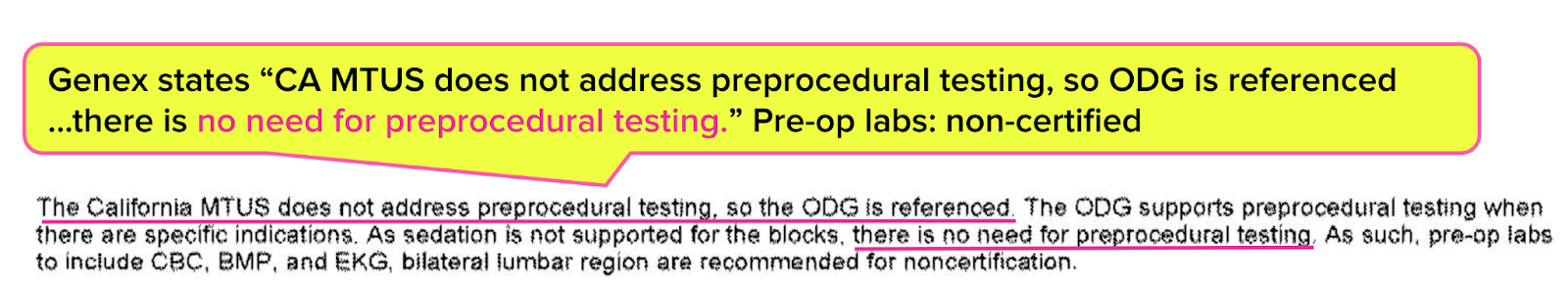
3. Genex Denies Pre-Op Testing
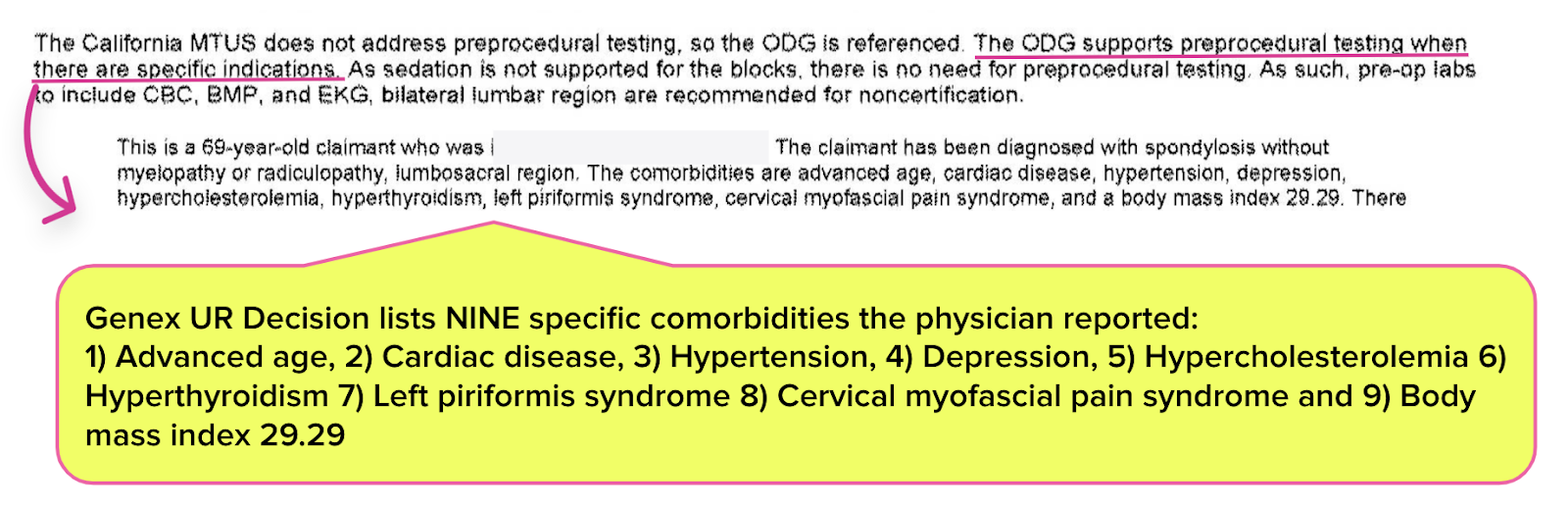
Given the injured worker’s list of comorbidities, the treating physician also requested preoperative testing to ensure the injured worker’s fitness for the approved procedure. The UR decision states, “there is no need for preprocedural testing.”
Once again, the UR decision cited the ODG.
Yet, the same UR decision also states, “The ODG supports preprocedural testing when there are specific indications. ”
The UR decision lists nine significant comorbidities the requesting physician reported for the 69-year-old — including cardiac disease, hypertension, and more. Still, the Genex UR physician denied pre-operative care for this injured worker as unnecessary.
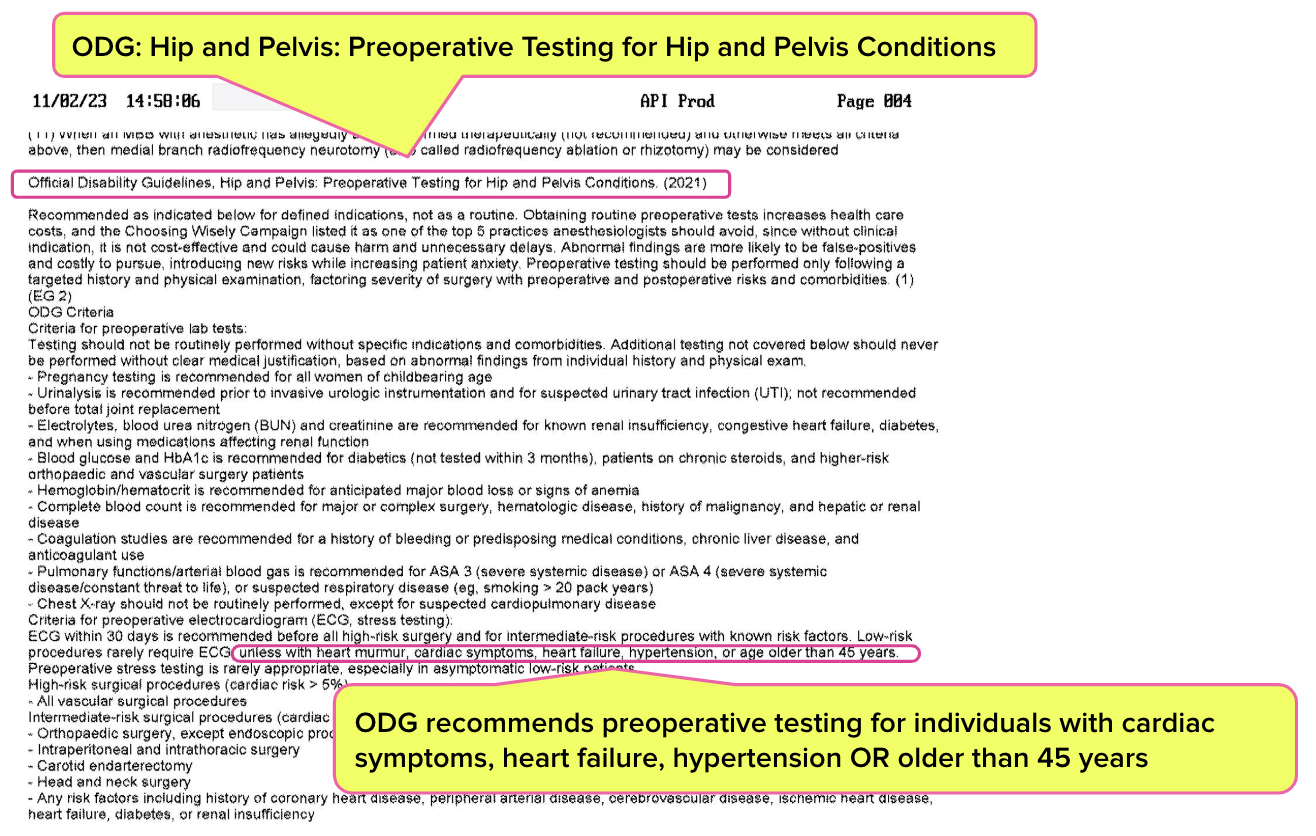
The decision also includes an excerpt from the ODG on preoperative testing (though inexplicably, Genex chose guidelines for hip and pelvis conditions rather than low back issues). According to the excerpt, the ODG recommends preoperative testing for patients with conditions like — wait for it — ”cardiac symptoms, hypertension, or age older than 45 years.”
To recap, Genex approved a procedure, then cited the wrong treatment guidelines to overrule the doctor’s pre-operative testing — even though those (wrong) treatment guidelines actually supported the doctor’s recommendation.
This is UR in California workers’ comp.
4. Genex Denies Medication for Pain Level 9/10
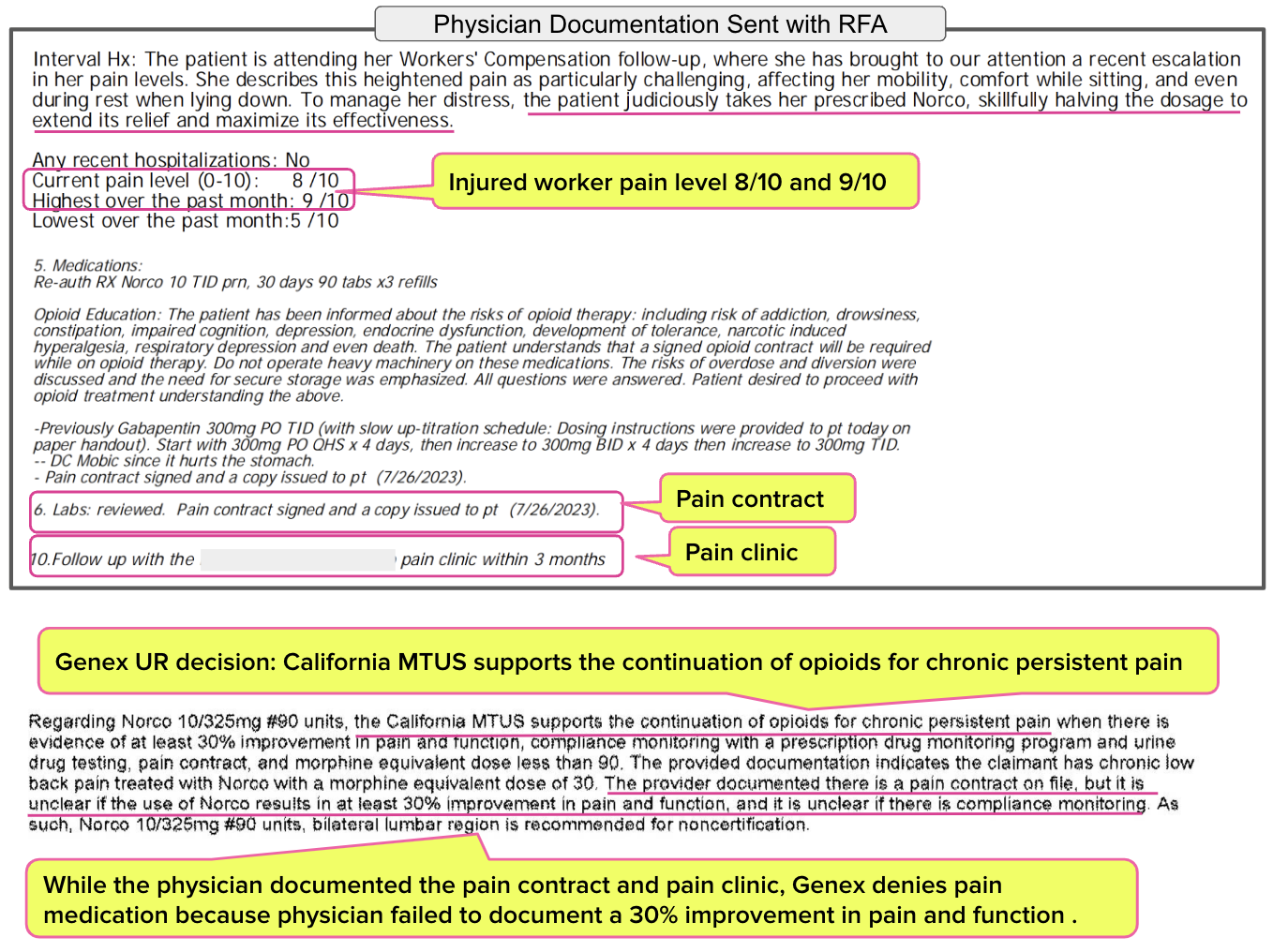
Finally, the Genex UR decision denied an opioid for pain management, this time citing the MTUS.
While we certainly understand the need to err on the side of caution about opioid over-prescription, the fact remains that such medications are considered appropriate for some patients in some situations. As Genex’s UR decision acknowledges, the MTUS “supports continued use of opioids for chronic persistent pain.”
However, Genex denied the requested medication, Norco, because the treating physician did not document a “30% improvement in pain” and function or sufficient compliance monitoring to prevent abuse.
Genex denied the pain medication despite the physician documenting the following facts:
- Pain level is reported at 8/10, with a high of 9/10
- Patient signed a contract regarding opioid use and its dangers
- Patient reportedly “judiciously takes her prescribed Norco, skillfully halving the dosage to extend its relief and maximize its effectiveness.”
- Patient was instructed to follow up with a pain clinic.
In denying pain medication for this injured worker, exactly how do Amtrust/Genex expect this injured worker to manage their pain?
AmTrust/Genex UR Medical Guideline Chaos
Only physicians are qualified to determine any treatment's medical necessity and appropriateness. Here at daisyBill, we are not physicians.
However, one does not need a medical degree to know that the ODG should not affect UR decisions in California when the state-established MTUS addresses the injury. Nor does one need to be a physician to see the blatant contradictions in how Genex incorrectly applied the (inapplicable) ODG.
Yes, AmTrust/Genex authorized the procedure. Still, this duo denied a 69-year-old injured worker the physician-recommended anesthesia, pre-op testing, and pain medication.
This AmTrust/Genex UR decision is emblematic of the wholly inadequate monitoring of California’s UR system.
Genex has successfully controlled costs for AmTrust by overruling a doctor who may be erring on the side of caution before operating on a senior with heart trouble. Without ascribing any intention to any URO, examples like this and others make it impossible not to question whether UR (by default or by design) better protects the interests of injured workers or payers.
daisyBill makes treating injured workers easier, faster, and less costly. Request a free demonstration below.
REQUEST DEMO
Page
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.
.gif)