AmTrust/Genex Use ODG to Deny Pre-Op Clearance
.gif)
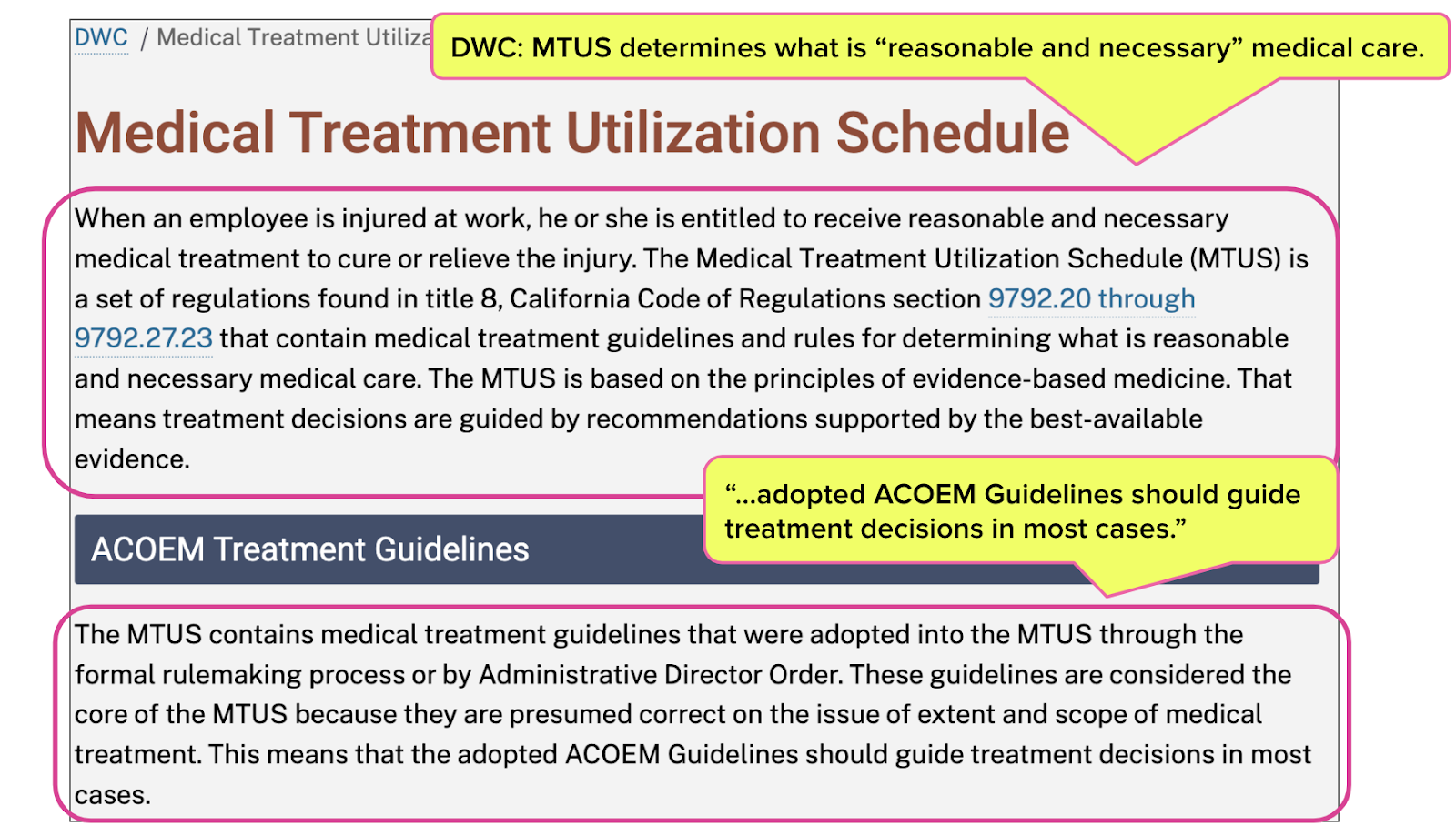
California law instructs physicians and claims administrators to consult the Medical Treatment Utilization Schedule (MTUS), adopted from the American College of Occupational and Environmental Medicine (ACOEM), to determine whether a treatment is medically necessary and appropriate for an injured worker.
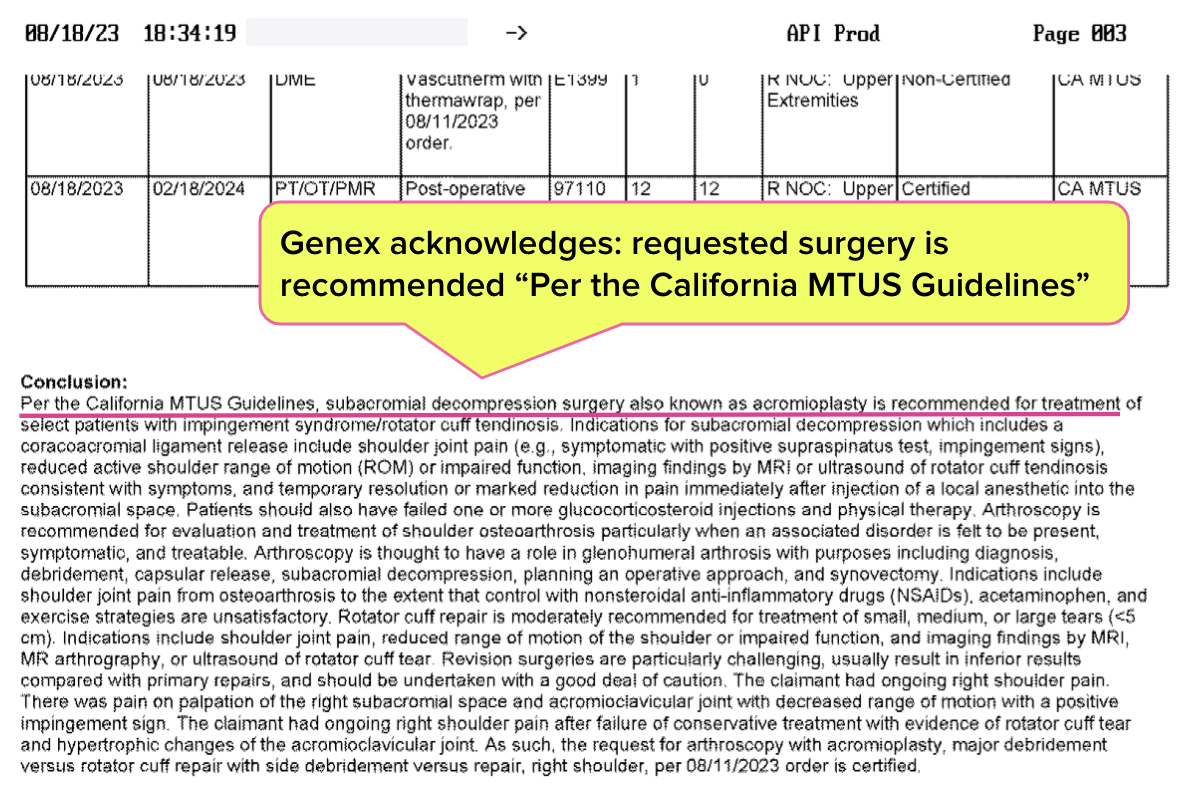
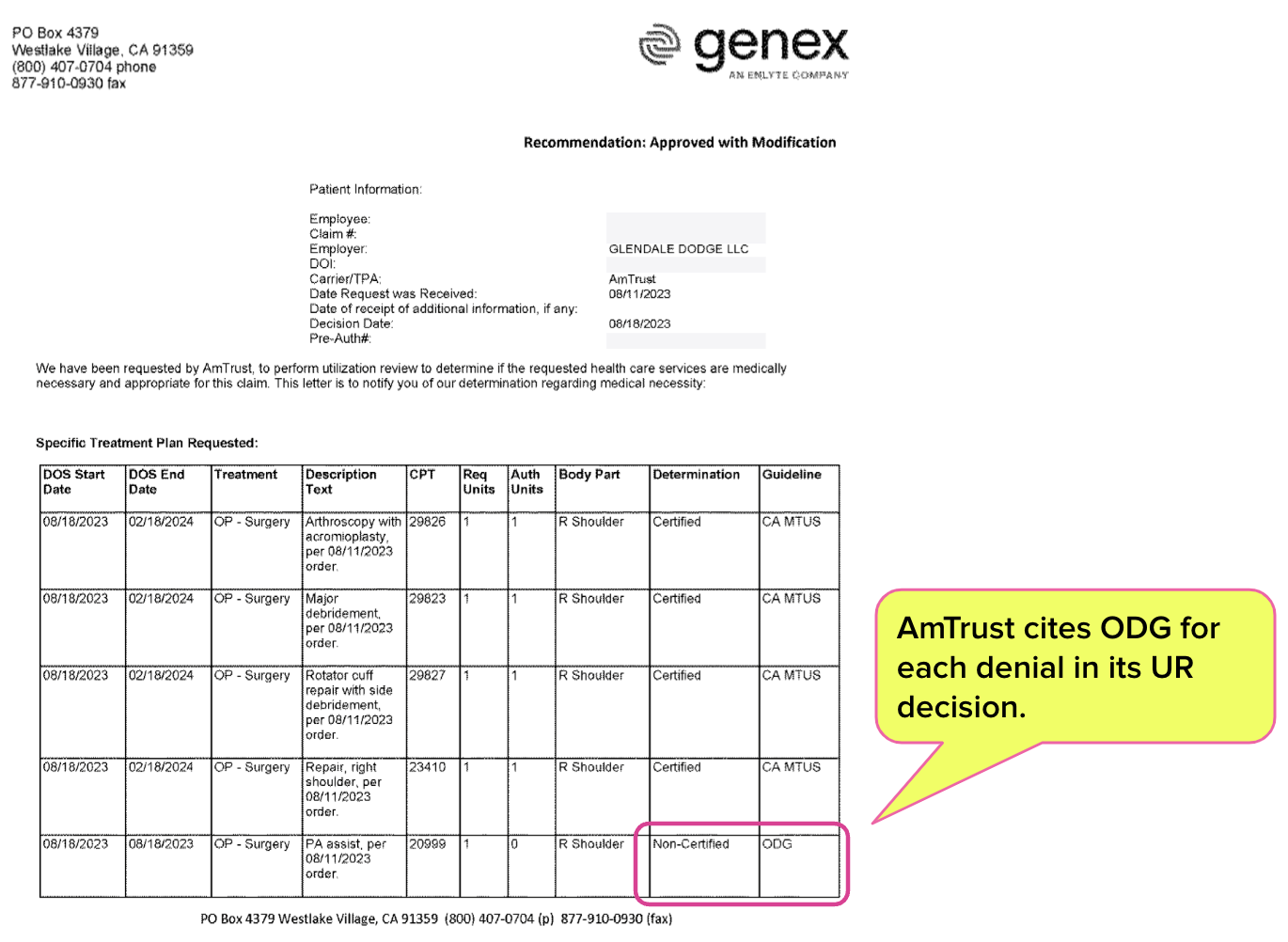
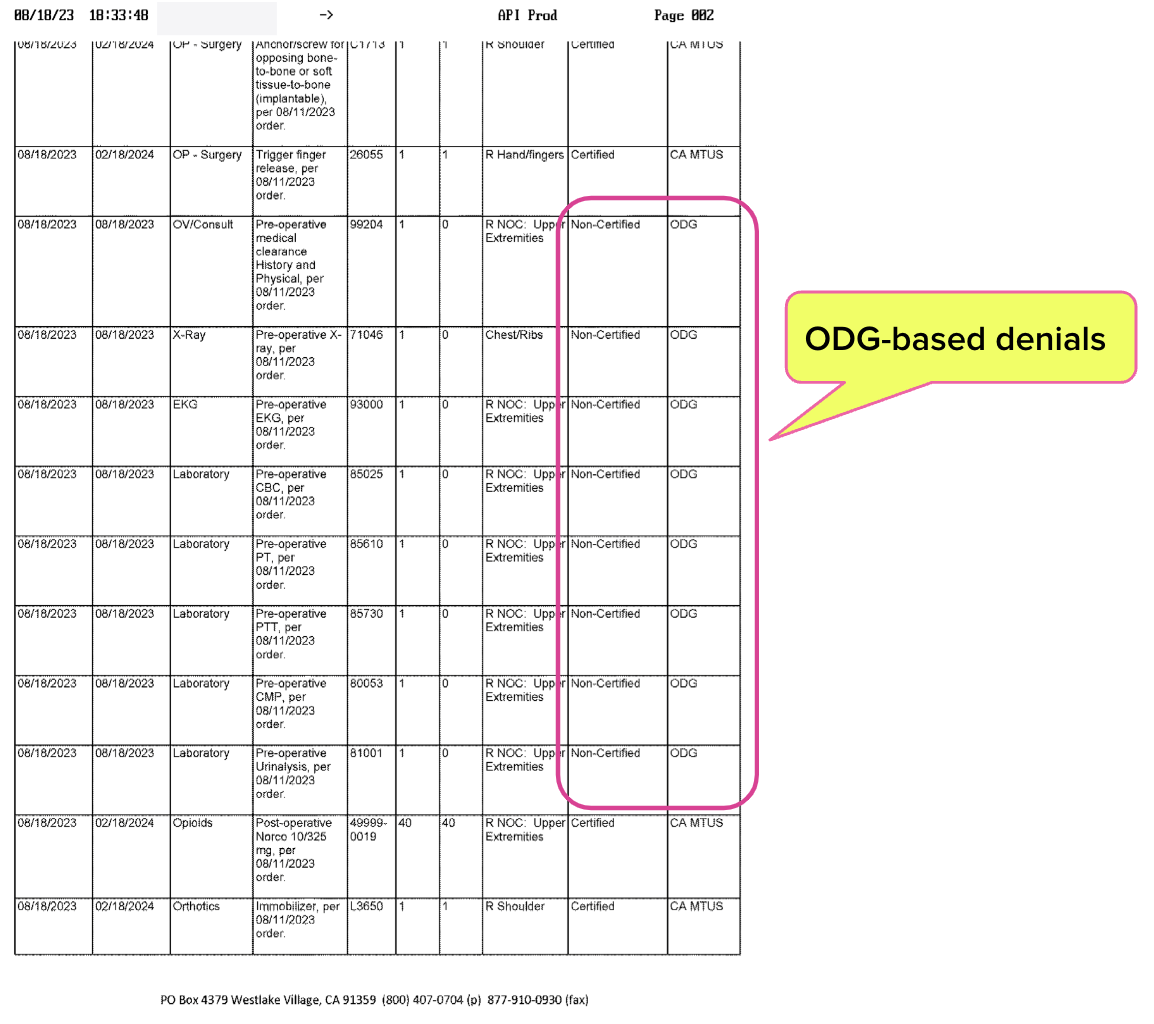
However, Third-Party Administrator (TPA) AmTrust and its Utilization Review Organization (URO), Genex issued a Utilization Review (UR) decision denying care requested by a treating physician, citing that the care did not adhere to the “Official Disability Guidelines” (ODG).
Once again, a claims administrator and its URO disregard California law to create needless obstacles to care.
AmTrust/Genex Cite ODG to Deny Care
For an injury that the MTUS addresses, a recent AmTrust/Genex UR decision presents a mixture of MTUS and ODG citations. The UR decision approves the requested surgery and acknowledges that “Per the California MTUS Guidelines,” the surgery is “recommended” for the injury in question.
There’s one (huge) problem: the MTUS, not the ODG, is the mandatory go-to reference for UR decisions in California workers’ comp.
MTUS: The CA Standard
California Code of Regulations Section Section 9792.21 instructs (emphases ours):
“The MTUS shall be the primary source of guidance for treating physicians and physician reviewers for evaluating and treating injured workers.”
The Division of Workers’ Compensation (DWC)’s MTUS web page (shown below) is clear that the MTUS is the standard for determining appropriate care for injured workers.
Moreover, §9792.21(d) allows AmTrust/Genex to use a guide other than the MTUS only “...if a medical condition or injury is not addressed by the MTUS…”
AmTrust/Genex acknowledged that the MTUS applies to the injury listed in the provider’s Request for Authorization (RFA). However, AmTrust/Genex denied the pre-operative care and surgical assistance recommended by the physician as not meeting ODG requirements.
ODG: NOT the CA Standard
The MTUS comprises guidelines from the ACOEM as adopted by the DWC, and is free for California physicians. Conversely, the Hearst Health Network sells the ODG in several states as a set of:
“...highly configurable, industry-specific medical treatment and return-to-work solutions that are used for managing workers’ compensation, disability, and auto liability claim outcomes with evidence-based, data-driven decision support.” [emphases ours]
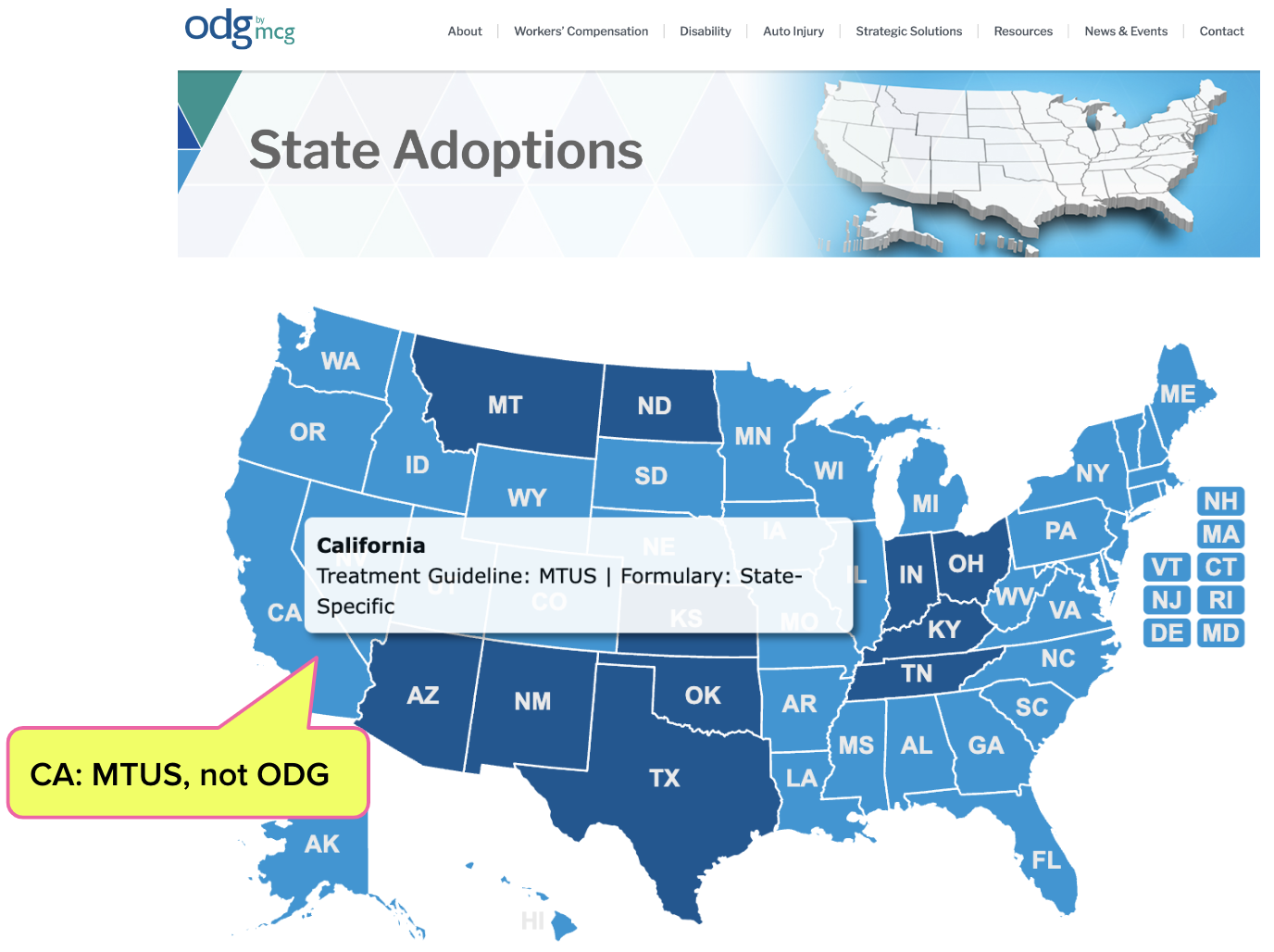
California has not adopted the ODG guidelines, as the ODG’s own website (shown below) acknowledges:
Only physicians are qualified to determine the medical necessity and appropriateness of a given treatment (we argue that the treating physician is much better positioned to make such determinations, as opposed to a far-off UR doctor working for the payer).
However, even physicians require evidence-based guidance.
It is troubling to see decisions about the health of injured workers made based on treatment guidelines that are openly advertised as “highly configurable” with the stated goal of “decision support,” especially when those guidelines were not adopted for California workers’ comp.
Submit RFAs in 30 seconds and automatically track UR decisions with daisyAuth. Request a demo below!
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


Touché