Costco: Helmsman Tries to Skirt Missed Appointment Fee

Denying payment to a Medical-Legal physician by falsely deeming a service non-compensable is a common — and contemptible — transgression. But Helmsman Management Services, a third-party administrator (TPA) acting on behalf of the self-insured employer Costco, added a peculiar denial twist.
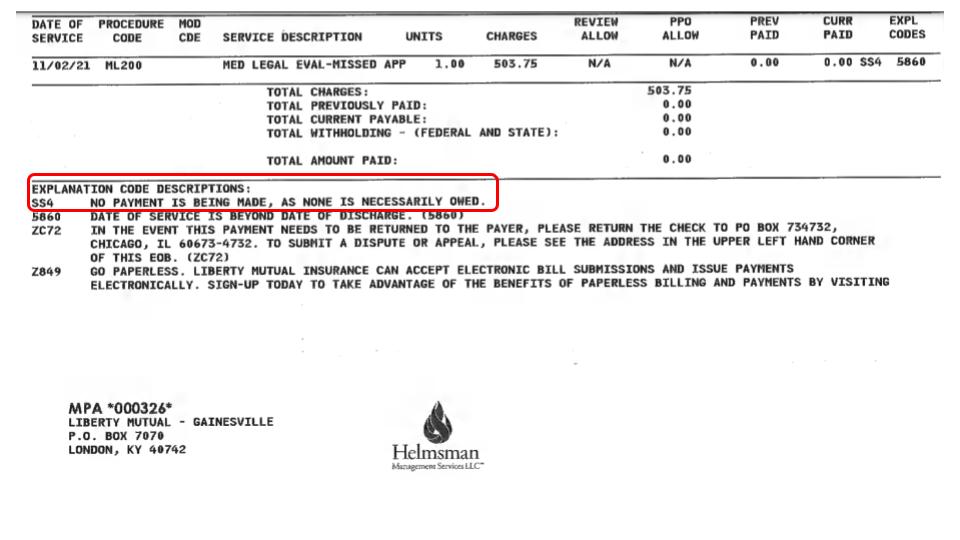
Recently, Helmsman denied payment to a medical-legal evaluator with the following denial reason: “No payment is being made, as none is necessarily owed.”
Believe it or not, Helmsman offered no further substantive explanation as to the reason Costco did not “necessarily owe” reimbursement for a missed medical-legal evaluation.
Missed Medical-Legal Appointment
The physician scheduled a Costco employee’s Medical-Legal evaluation for November 2, 2021. One day prior to the scheduled evaluation, the physician received notification that the injured worker couldn’t make the appointment.
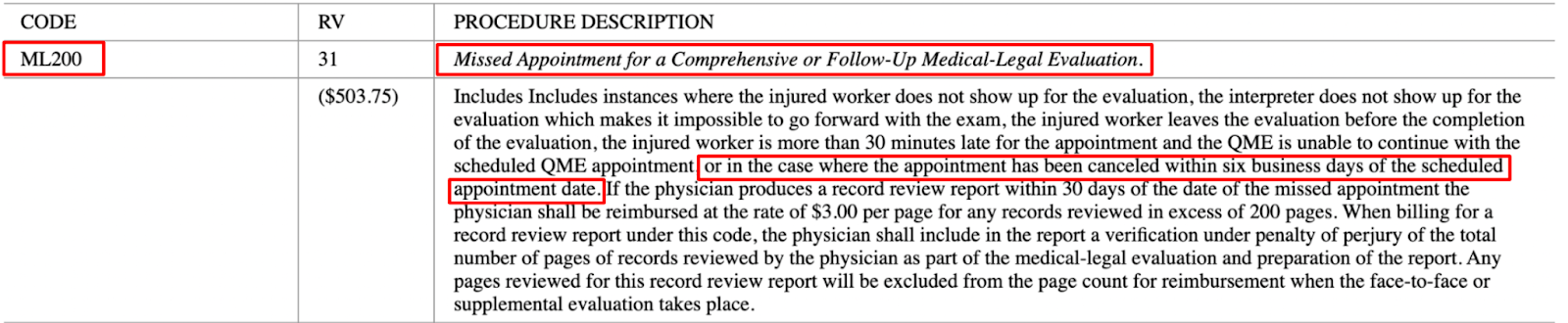
California Code of Regulations Section 9795 specifies that for missed medical-legal evaluation appointments, an evaluator is allowed to bill ML200 when an evaluation appointment is canceled with less than 6 days advance notice.
The required advance notice was not provided, so the evaluator billed Helmsman ML200 for the missed appointment.
Helmsman’s Faulty EOR Reasoning
In response to the ML200 bill, Helmsman sent the Explanation of Review (EOR) pictured below, claiming that “NO PAYMENT IS BEING MADE, AS NONE IS NECESSARILY OWED.”
As seen below, missed comprehensive or follow-up Medical-Legal appointments are billable under ML200 in a variety of circumstances.
The procedure description for code ML200 allows physicians to bill for missed Medical-Legal Appointments when:
- The injured worker does not show up for the evaluation
- The interpreter does not show up for the evaluation, which makes it impossible to go forward with the exam
- The injured worker is more than 30 minutes late for the appointment and the QME is unable to continue with the scheduled QME appointment
- The appointment has been canceled within six business days of the scheduled appointment date
Bottom line: Helmsman’s denial of payment for the service is in clear violation of CCR §9795. When an injured worker fails to appear for an evaluation appointment without at least 6 days of notice, reimbursement under ML200 is due.
Second Review Success
The provider submitted a Second Bill Review appeal to dispute the improper denial.
Helmsman paid the balance.
Wise decision. Backed by documentation from daisyBill, the provider was prepared to meet the claims administrator’s failure to properly reimburse ML200 with a request for Independent Bill Review (IBR).
Nevertheless, this is yet another example of how critically important it is for California workers’ comp providers to carefully track of improper bill adjustments, and always submit a timely Second Review appeal to dispute absurd denials justified by absurd reasons (“No payment is being made, as none is necessarily owed.”)
Claims Admins’ Waiting Game is Grueling for Providers
The provider won this round of what we’ll call “SBR Chicken.” Still, the victory feels hollow.
Without a Second Review appeal, this provider would have missed out on payment clearly called for by the Medical-Legal Fee Schedule. California workers’ comp should penalize claims administrators’ for engaging in these costly “games'' that drive doctors to abandon treating injured workers.
Claims administrators continue to flout and bend DWC regulations with little to no fear of repercussion.Playing chicken is played out. It’s past time the DWC makes claims administrators, like Helmsman (or Costco), pay for their noncompliance — without the games.
Make it harder for claims admins to improperly deny payment. Your office deserves to get paid, in full and on time. daisyBill has the tools — reach out to learn more.
CONTACT DAISYBILL
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.

.gif)
