DWC Cracking Down on Late Responses to Requests for Authorization

On February 10th, 2016, the DWC issued DIR Newsline 2016-19 reminding claims administrators that adhering to Utilization Review (UR) timelines is mandatory and that failure to observe timelines triggers compliance penalties. The newsline alerted claims administrators that the DWC Audit Unit intends to pursue more Target Audits for reported utilization review complaints.
If a claims administrator violates the rules governing Utilization Review (UR), the DWC applies a mandatory penalty for “each failure to comply with the utilization review process.” In this article, I break down the penalties for untimely and unanswered UR responses to expedited RFAs, concurrent RFAs, prospective RFAs, and retrospective RFAs.
Mandatory Penalties for Late or Missing RFA Response
On its UR FAQ page, the DWC details specific UR penalties for a claims administrator that fails to meet mandated timeframes for RFA response.
- Unanswered RFA penalties:
- Concurrent RFA: $2,000
- Prospective RFA: $1,000
- Retrospective RFA: $500
- Expedited RFA: $15,000
- UR decision not communicated within the appropriate timeframe:
- Concurrent, prospective, or retrospective RFA: $100
- Expedited RFA: $15,000
Up to $50,000 in Other UR Penalties
The DWC gives the highest penalties to claims administrators who fail to establish any kind of UR plan. Failure to establish a UR plan warrants a mandatory $50,000 penalty.
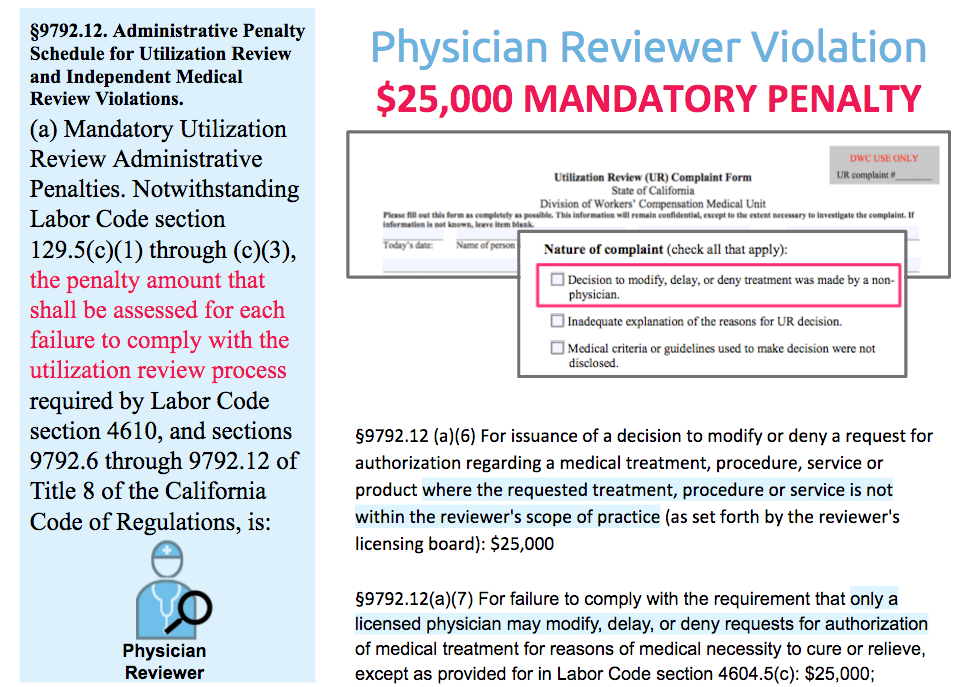
A physician reviewer violation causes the second highest penalty. A physician reviewer violation occurs when a non-physician delays, denies, or modifies a treatment request, or when the UR decision is outside the scope of the reviewer’s practice. A physician reviewer violation warrants a mandatory $25,000 penalty for each failure.
Claims Administrators: To prevent UR penalties, pay close attention to UR timelines and DWC regulations. For free help, contact daisyBill.
Providers: To report UR complaints, use the DWC UR Complaint Form. When reporting an untimely decision or response, include the dates of RFA submission and due date. daisyBillers can use daisyBill’s RFA History as supporting evidence of missed timelines.
For more information on RFAs, watch our free workers’ comp RFA webinar:
VIDEO AND SLIDES
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.gif)