EK Health: Denying Care Helps Injured Workers
%20(1).gif)
EK Health wants you to know that Utilization Review (UR) is not a soulless tool that payers use to deny injured workers the care recommended by their treating physicians.
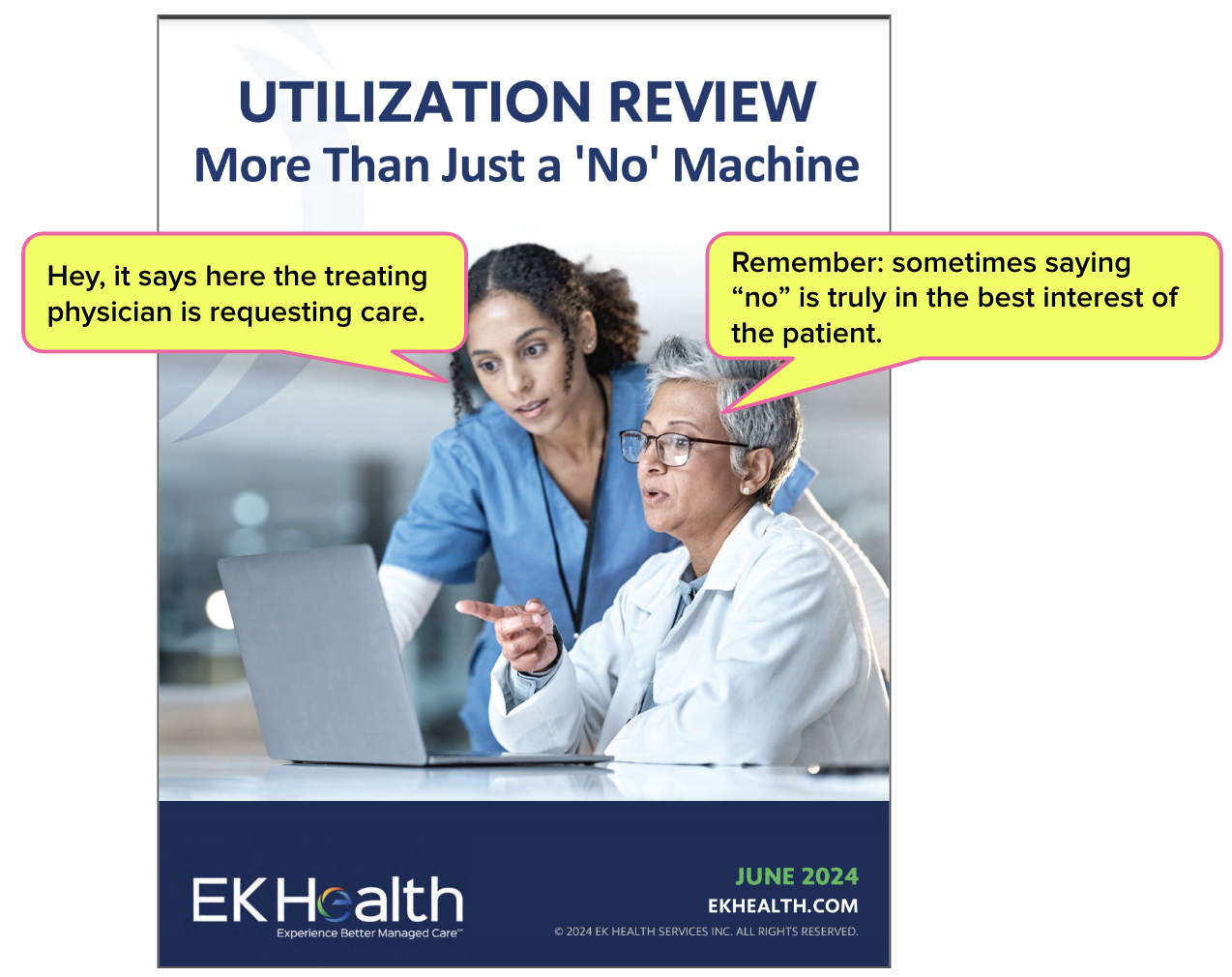
According to EK Health’s most recent work of corporate literary art, UR is “More Than Just a ‘No’ Machine.” EK Health presents UR as an essential tool in “mitigating unnecessary treatment” that “enhances patient outcomes and quality of care,” and proclaims that saying “no” can be “truly in the best interest of the patient.”
Putting aside the Orwellian leaps of logic required to imagine UR protecting injured workers from receiving too much treatment, EK Health’s missive ignores a critical reality: no one knows if UR is being conducted appropriately by any organization.
No one knows because the California Division of Workers’ Compensation (DWC) has failed to implement two state laws instructing the DWC to collect employer UR data and present it to legislators and the public.
Since 2016, the DWC has simply ignored the California law that requires it to collect UR decisions and document the frequency of denials by each employer/insurer. Even though gathering this data would protect injured workers from the UR “No Machines” that EK Health seems to acknowledge exist, the agency offers no reasons for pooh-poohing legislators’ directive.
Further, in 2019, California amended the Labor Code to mandate that the DWC publicly post detailed data on individual workers’ comp doctors by January 1, 2024—including how many of each doctor’s treatment requests were denied or modified by the claims administrator. The DWC scoffed at this law as well, and produced no such data.
Instead of adhering to UR laws, the DWC uses its powers to impose new reporting forms on providers who already struggle with the administrative costs of treating injured workers. The DWC offers no substantive justification for these form changes while openly admitting the transition will be costly for providers.
EK Health’s UR blather magnifies the fact that California’s DWC is not a functioning agency that protects injured workers from UR “No Machines.” Instead, the DWC guards the profits of claims administrators, their side-kick vendors, and their private equity owners while ignoring laws that would expose predatory UR practices.
CA DWC: Failing to Collect UR Data Since 2016
Eight years ago, California legislators understood that by abusing UR, claims administrators could refuse medically necessary and appropriate care to save a buck. Therefore, these legislators wisely amended Labor Code Section 4610 to mandate that the DWC collect UR data to monitor for non-compliance and abuse.
The amended Labor Code requires the DWC to establish “mandatory electronic reporting of documents related to every utilization review performed by each employer [or employer’s insurer].” That’s “mandatory,” not optional.
The only problem? The DWC has ignored this UR law for the better part of a decade, allowing claims administrators to build monster-sized UR “No Machines” without any regulatory oversight. This abdication of one of its most basic administrative duties is despicable, but perfectly on-brand for the DWC, which has amply demonstrated its preference for letting claims administrators run wild.
Rather than focusing on injured workers’ access to care by enforcing UR compliance, the DWC instead spent its time crafting burdensome new reporting forms for providers. While claims administrators and their Utilization Review Organizations (UROs) operate without fear of repercussions for non-compliance, the DWC forces providers to expend time and resources complying with ill-conceived demands for new paperwork.
EK Health Explains it All
Feast on the prose below from EK Health describing how a UR physician (who has never met the injured worker) can actually help the worker by saying “no” to the care recommended by the treating physician.
“In actuality, sometimes saying “no” is truly in the best interest of the patient. UR ensures that an appropriate standard of care is delivered.”
The DWC’s refusal to gather UR data makes it easy for companies like EK Health to paint UR in any light they choose—no one can argue, since this system is effectively unmonitored. Without the DWC tracking UR decisions in any meaningful way, the “No Machines” reign.
Submit RFAs in 30 seconds and automatically track UR decisions with daisyAuth. Request a demo below!
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.




It's time a Writ of Mandamus was filed, requiring the AD to comply with LC 4610(q): "The administrative director shall contract with an outside, independent research organization to evaluate the impact of the provision of medical treatment within the first 30 days after a claim is filed, for a claim filed on or after January 1, 2017, and before January 1, 2021. The report shall be provided to the administrative director, the Senate Committee on Labor and Industrial Relations, and the Assembly Committee on Insurance, pursuant to Section 9795 of the Government Code, before July 1, 2023."