Medata Harrasses CA Provider for Requesting IBR
Medata, which conducts bill review for the City of Los Angeles, just gave a master class in how claims administrators’ vendors bully providers who are simply trying to receive payment for treating injured workers.
In California, some claims administrators and their bill review vendors engage in "IBR Chicken,” a tactic in which the bill review denies or underpays a provider’s bill, knowing the provider must either capitulate or engage in a costly and time-consuming appeals process. Here’s how it works:
- Initial Denial: The claims administrator’s vendor denies or underpays an original bill on often spurious grounds.
- Second Review Appeal: The provider must file a Second Review appeal within 90 days, requiring significant administrative effort.
- Further Denial: The claims administrator’s vendor denies the Second Review appeal, at which point the provider’s only option is to request IBR within 30 days, at a cost of $180.
If the provider won’t give up the fight, there’s one more move in IBR Chicken: pay the amount owed after the provider requests IBR, and demand that the IBR request be withdrawn.
IBR Chicken is intended to overwhelm providers with administrative burdens and costs, discouraging them from pursuing payment. Claims administrators have the advantage because if the provider makes any mistake in pursuing appeals, the claims administrator keeps the disputed funds by default.
IBR Chicken isn’t new—but Medata took it to an entirely new level in the incident detailed below.
After the provider dutifully paid $180 to file for IBR to dispute a payment denial, Medata reimbursed the provider (but not the $180 IBR fee). However, Medata then took extraordinary steps in demanding the provider withdraw the IBR request. Medata repeatedly requested the name of the biller who filed the request, and in a possible veiled threat, made repeated references to the provider’s membership in the City of LA’s Medical Provider Network (MPN) and Preferred Provider Organization (PPO).
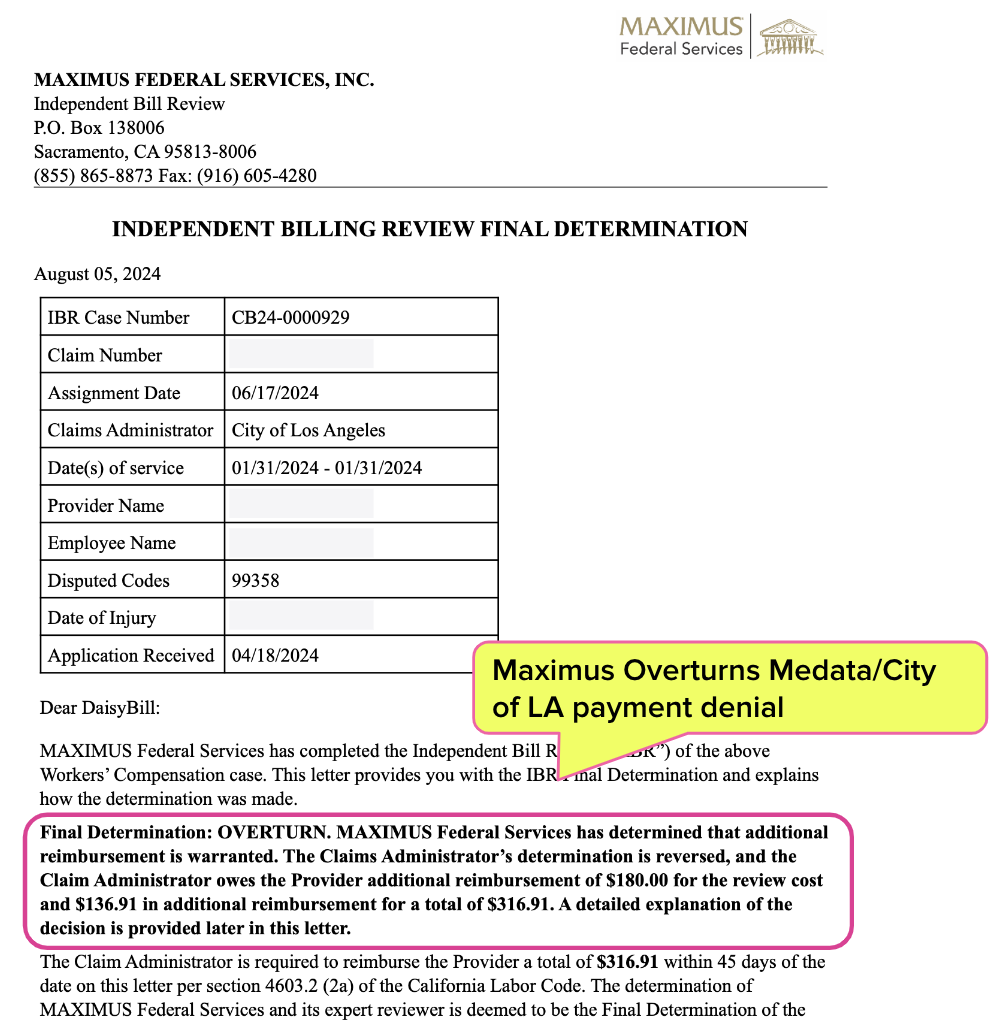
Wisely, the provider refused to capitulate, and Maximus overturned Medata’s payment denial and ordered the City of Los Angeles to reimburse the provider the $180 IBR fee.
Providers should take this as a lesson: stand firm, even in the face of apparent bullying. Claims administrators should take note of the manner in which Medata treats providers who simply want to be paid correctly.
Medata Denies Payment, Reverses Course After IBR Request
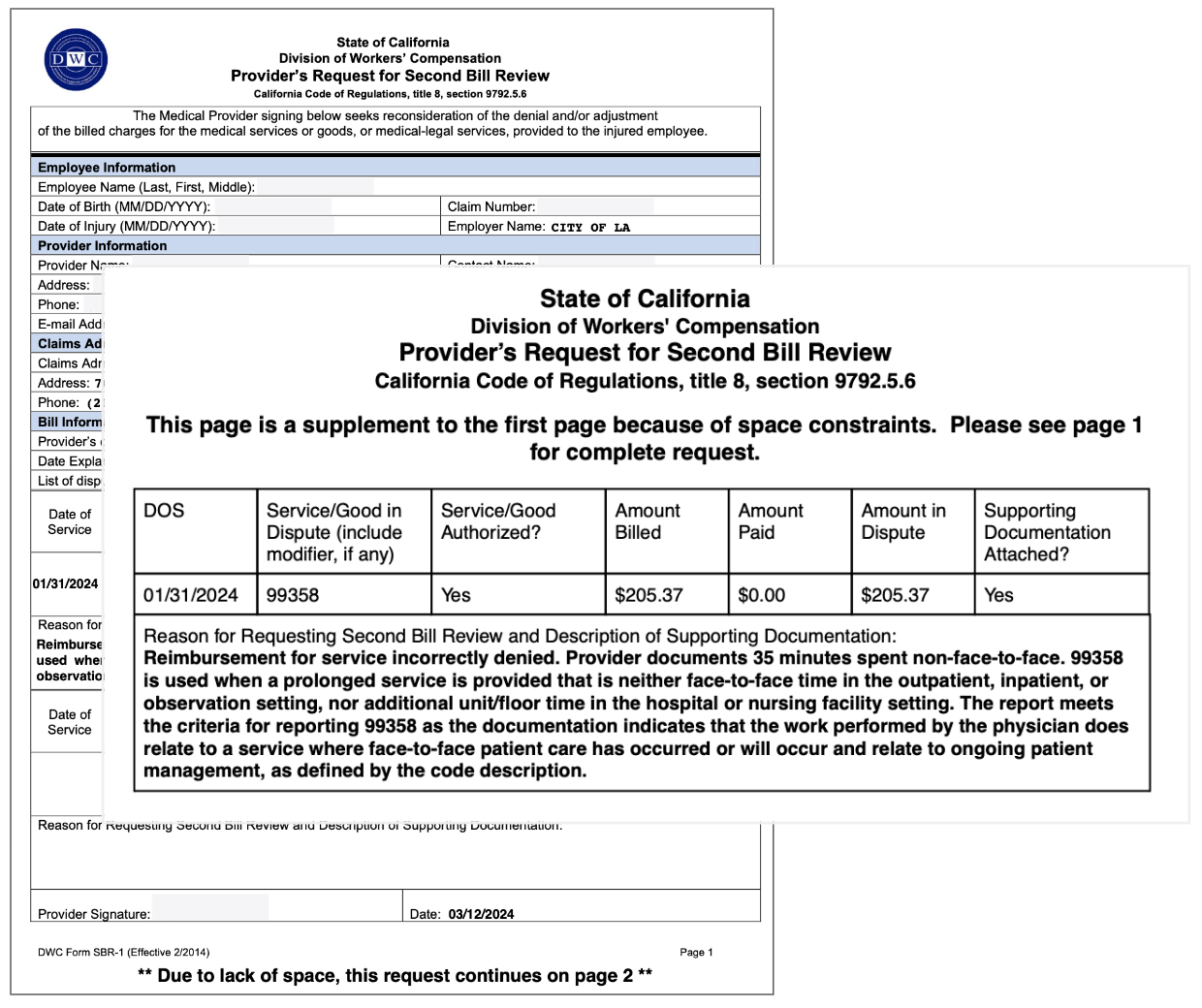
In January of 2024, a Primary Treating Physician (PTP) reviewed medical records as part of standard Evaluation and Management (E/M). Appropriately, the provider billed the City of LA for prolonged non-face-to-face services using billing code CPT 99358.
The City of LA sent the provider an Explanation of Review (EOR) denying payment for the prolonged non-face-to-face services, claiming the provider’s documentation was insufficient—despite the fact that the documentation submitted with the bill perfectly substantiated the charge as billed, as shown below.
To dispute the incorrect payment denial, the provider submitted a timely Second Review appeal (shown below), explicitly outlining how the documentation submitted supported the CPT 99358 charge.
The City of LA denied payment again, sticking to its untrue claims of insufficient documentation.
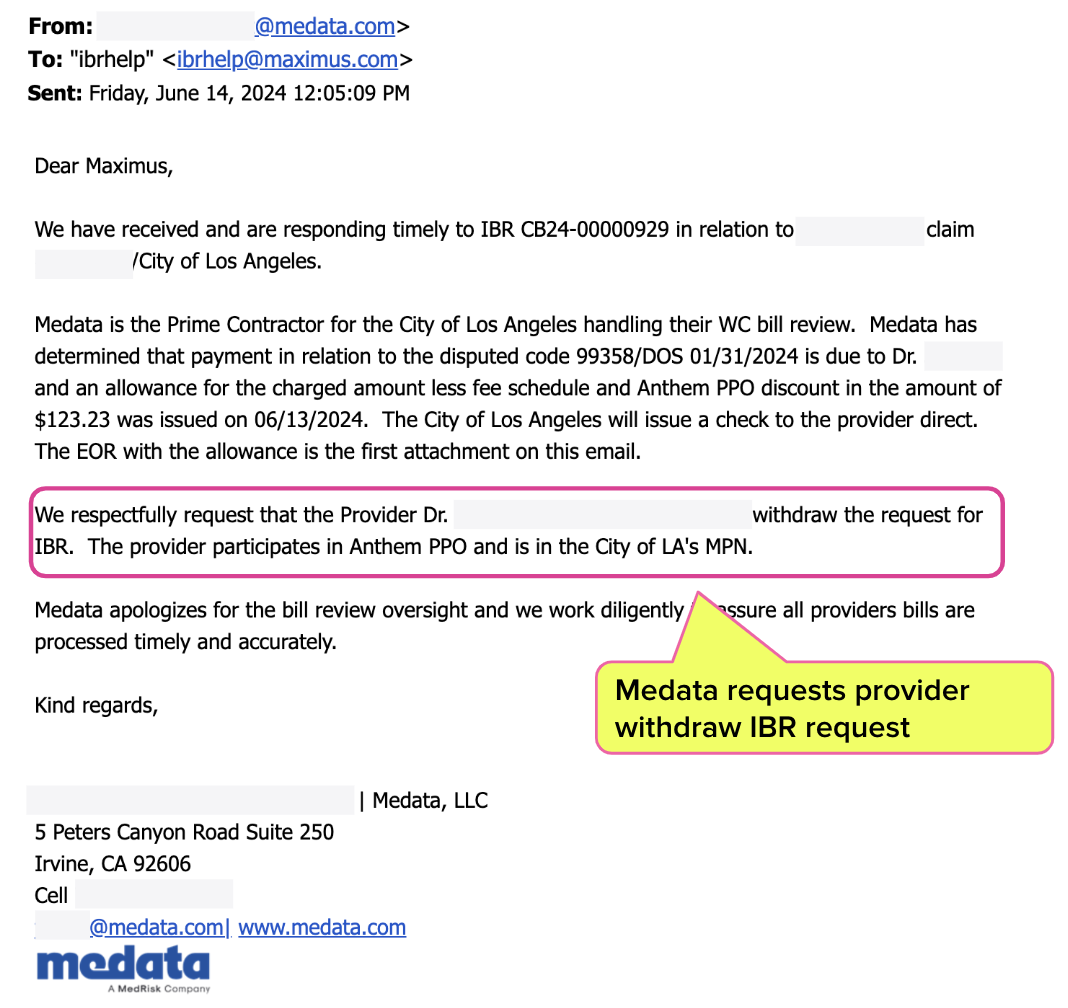
With no other option, the provider paid $180 to request IBR. And as is (too) often the case, the threat of intervention by the state caused a sudden, inexplicable reversal of the denial. Medata, whose bill review error was the basis for the City of LA’s improper payment denial, emailed Maximus and the provider stating (emphasis ours):
“Medata has determined that payment in relation to the disputed code 99358/DOS 01/31/2024 is due to [the provider] and an allowance for the charged amount less fee schedule and Anthem PPO discount in the amount of $123.23 was issued on 06/13/2024…
…We respectfully request that [the provider] withdraw the request for IBR. The provider participates in Anthem PPO and is in the City of LA's MPN.”
We can assume the reference to the Preferred Provider Organization (PPO) and MPN were meant to justify the PPO discounts Medata applied to the payment. But it wouldn’t be the last time Medata pointedly reminded all parties of the provider’s MPN status.
Medata Hunts Down Biller
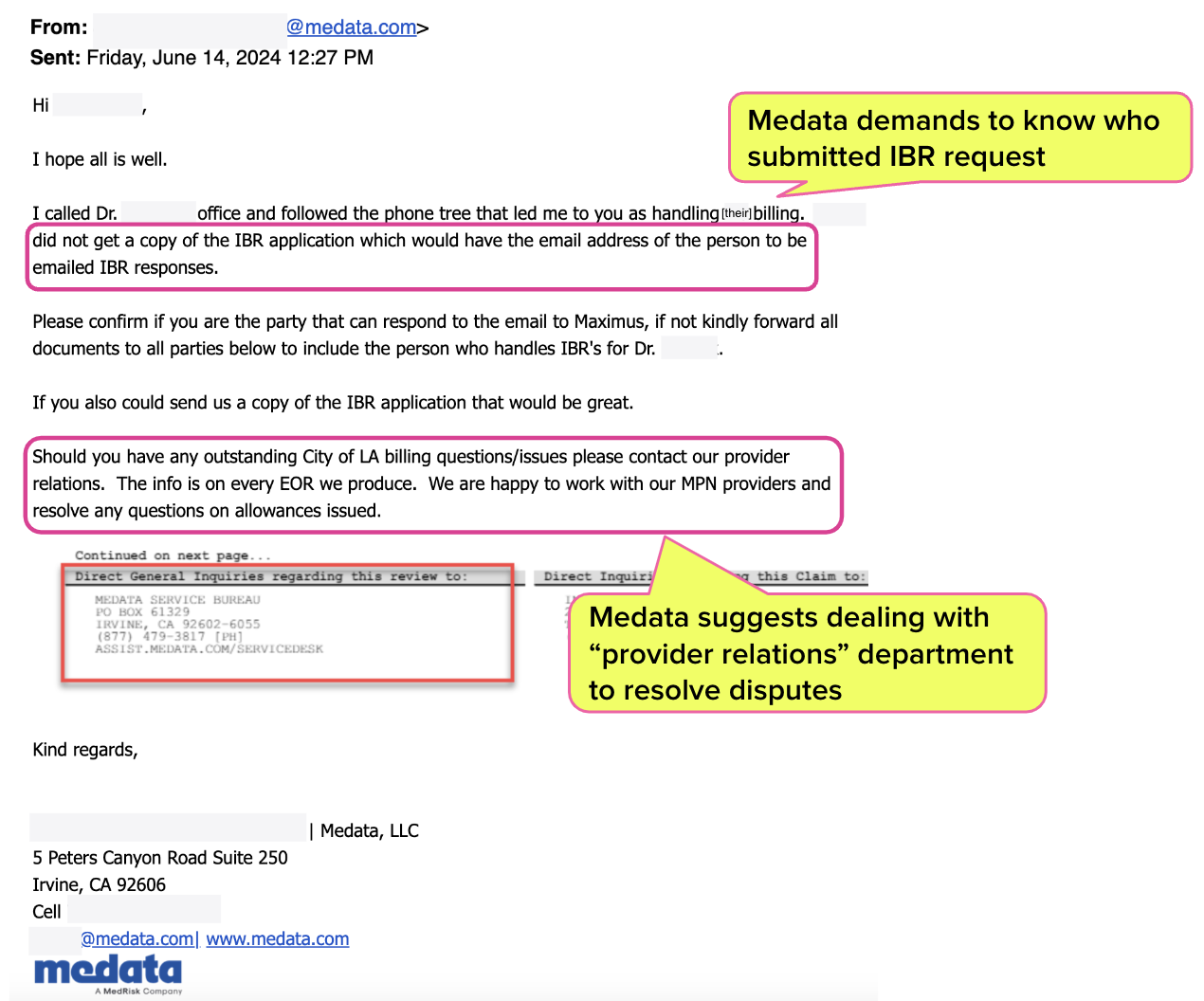
Medata went beyond asking for the IBR case to be dismissed.
Medata emailed the provider inexplicably demanding to know the name of the person who specifically requested IBR on the provider’s behalf and requested contact information for this person. While Medata attempts to justify this demand, there are no “Maximus IBR purposes” under which Medata needs the billers’ name.
“...kindly forward the email you sent to the person who handles IBRs for [the provider] and cc all with all documents. I need documentation and the person's information for Maximus IBR purposes.”
Further, rather than respect California law, which mandates providers must file Second Review appeals and IBRs to dispute incorrect payments, Medata claimed that its in-house “provider relations” is the appropriate way to resolve payment disputes:
“Should you have any outstanding City of LA billing questions/issues please contact our provider relations. The info is on every EOR we produce. We are happy to work with our MPN providers and resolve any questions on allowances issued.”
This Medata instruction is laughable, considering the fact that Medata and the City of LA had a chance to address the error before IBR was invoked. Most importantly, California law allows the claims administrator to retain the provider’s reimbursement if the provider fails to adhere to the mandated appeal steps.
The provider followed California requirements and submitted a timely, compliant Second Review appeal, which Medata unceremoniously denied. Why would any rational provider attempt to resolve a dispute with Medata’s “provider relations” when the company had already refused to adjudicate the bill properly—twice?
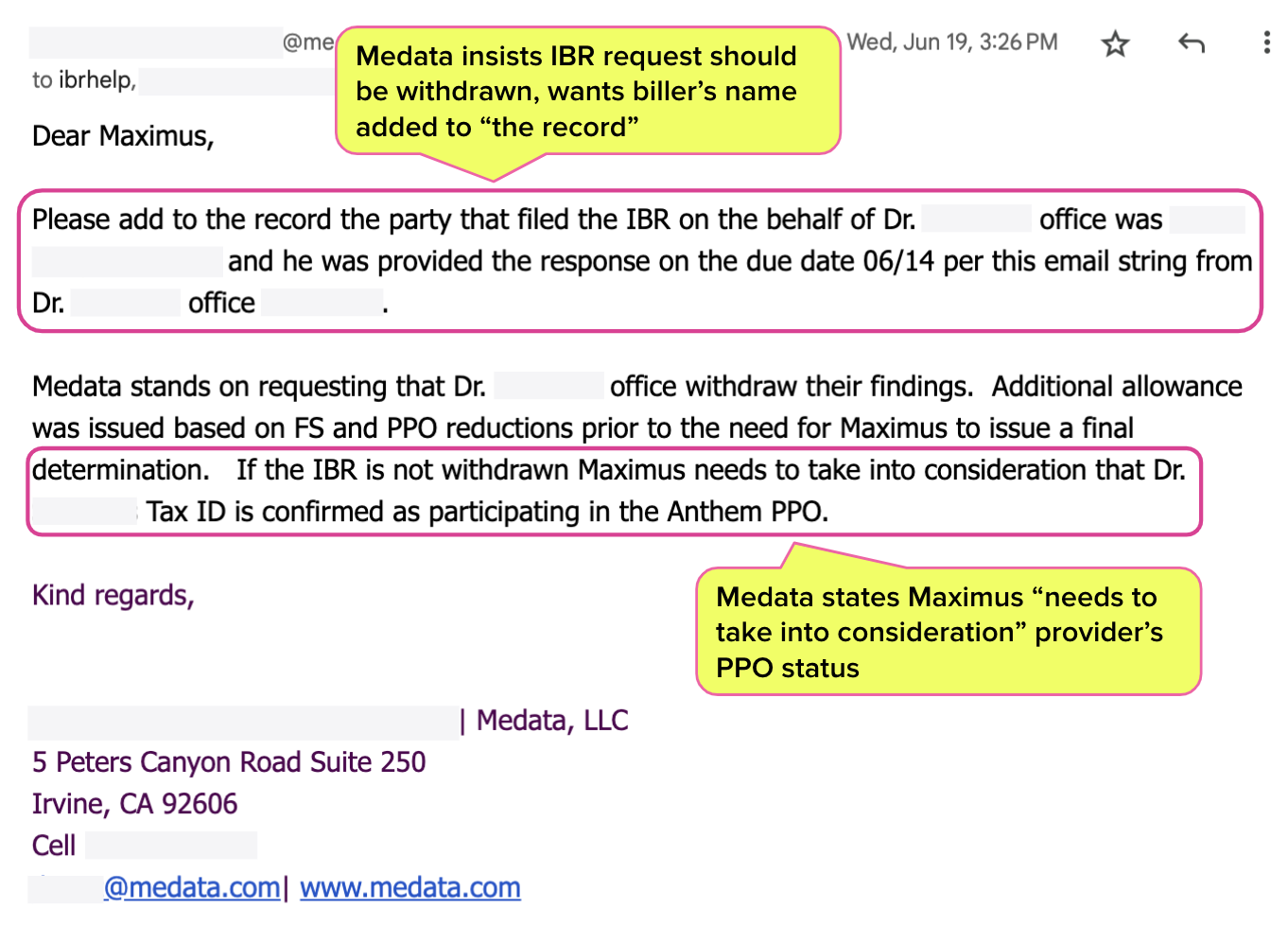
Strangely, once Medata had the biller’s name, Medata emailed Maximus, asking that the biller’s name be made part of the official record for…well, for no rational reason we can think of.
Again, Medata noted that if the IBR was not withdrawn, Maximus “needs to take into consideration” the provider’s PPO status. Medata’s message is below.
This strange and frankly inappropriate Maximus email raises two questions:
- Why was Medata so fervent about documenting the individual biller who (quite appropriately, compliantly, and legally) requested IBR on the provider’s behalf.
- Why did Medata insist that if the IBR request wasn’t withdrawn, “Maximus needs to take into consideration” the provider’s PPO/MPN status?
If this was an attempt at intimidation, it was an awkward one—but no less acceptable for being so. The simple facts of the matter are that Medata screwed up, and the City of LA failed to pay a provider as a result. The provider then took the required, established recourse to pursue payment.
Pro tip for Medata: when you make a mistake, own it. Correct your errors at the Second Review stage. Otherwise, providers must pay $180 to request IBR.
Maximus ruled in the provider’s favor, overturning the payment denial and ordering the City of LA to pay the amount owed plus the $180 IBR filing fee. Stay tuned as to whether City of LA reimburses the provider the $180 IBR fee…
With tools for quicker, easier appeals, daisyBill helps your practice demand full reimbursement — with just a few clicks. Learn more or request a demo below:
LEARN MORE
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.

%20(1).gif)


.gif)
Threshold issues throw this process out the window. A simple objection outlining how SBR and IBR are premature due to threshold issues, after receiving assignment from Maximus, stops this whole process from getting started(I’ve done this plenty)That’s what the city should have done when bringing up MPN.
Medata is not entitled to the name and contact info of the person who requested IBR, just like the provider is not entitled to the identity of the medical bill reviewer. Nor is the provider entitled to ask for a copy of the medical bill reviewer's biannual educational designation certificate proving the bill reviewer is allowed by law (Ins. Code 11761) to perform their job.