Med-Legal Diagnostic Testing Is Reimbursable

FAQ: Is diagnostic testing, as part of a Medical-Legal evaluation, separately reimbursable?
A: Yes, as long as the testing is necessary to complete the evaluation.
Nevertheless, we continue to see claims administrators refuse payment for diagnostic testing when ordered by the physician as part of a Medical-Legal evaluation.
As a result, providers (understandably) repeatedly ask DaisyBill if claims administrators must reimburse diagnostic tests in a Medical-Legal context — and if the employer’s Utilization Review (UR) must authorize the testing. Below, we explain how to obtain reimbursement for Medical-Legal diagnostic tests, and how to dispute incorrect denials thereof.
Med-Legal Diagnostic Testing (and How to Bill For It)
Reimbursement for diagnostic testing procedure codes is not included in the existing Medical-Legal Fee Schedule (MLFS) billing codes. However, diagnostic testing is sometimes necessary to complete a Medical-Legal evaluation and prove or disprove a disputed fact.
For that reason, for Medical-Legal evaluations, California regulations allow physicians to perform diagnostic tests without obtaining authorization from the claims administrator. The bill for the physician’s medical-legal evaluation should include any diagnostic tests performed for the evaluation. These diagnostic tests are reimbursed using the Official Medical Fee Schedule (OMFS) rates.
California Code of Regulations (CCR) Section 9794, Reimbursement of Medical-Legal Expenses, states in subsection (a)(1):
“X-rays, laboratory services and other diagnostic tests shall be billed and reimbursed in accordance with the official medical fee schedule adopted pursuant to Labor Code Section 5307.1.”
§9794(a)(1) also requires the physician to document in the evaluation report that the diagnostic testing was genuinely called for, as evidenced by the patient’s complaints and the findings of a physical examination:
“In no event shall the claims administrator be liable for the cost of any diagnostic test provided in connection with a comprehensive medical-legal evaluation report unless the subjective complaints and physical findings that warrant the necessity for the test are included in the medical-legal evaluation report. [emphasis added]”
Finally, §9794(a)(1) warns physicians that diagnostic tests are not reimbursable when the medical records sent to the physician already contain the information that a given diagnostic test would provide:
“Additionally, the claims administrator shall not be liable for the cost of diagnostic tests, absent prior authorization by the claims administrator, if adequate medical information is already in the medical record provided to the physician.”
Regarding authorization, the Division of Workers’ Compensation (DWC) affirms that authorization is not required for Medical-Legal diagnostic testing on their UR FAQ page, stating:
“...Diagnostic tests ordered as part of a medical/legal evaluation are medical/legal expenses, not treatment expenses. A claims administrator must pay for a diagnostic test ordered by an AME or QME as long as the subjective complaints and physical findings that warrant the necessity for the test are included in the medical/legal evaluation report…”
In summary, to ensure reimbursement for a diagnostic test as part of a Medical-Legal evaluation, be sure to:
- Review the medical records before ordering any diagnostic test, to ensure that the testing is not redundant or otherwise unnecessary based on existing information.
- Include in the evaluation report the subjective complaints and physical findings that warrant the testing.
- Bill separately for any testing at OMFS rates.
Claims Administrators Correct Incorrect Adjustments
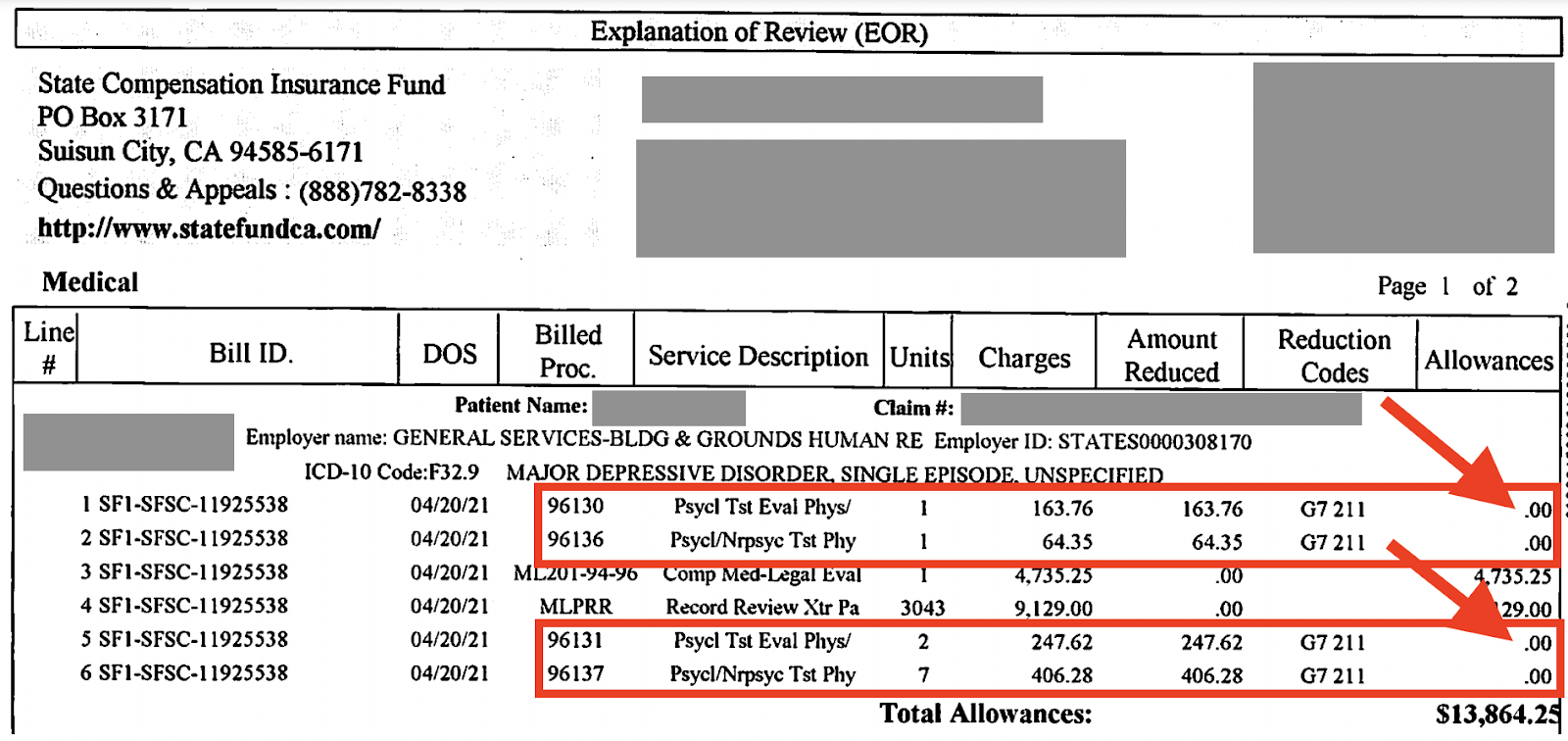
Recently, the State Compensation Insurance Fund (SCIF) provided a perfect example of an incorrect denial of charges for Medical-Legal diagnostic testing. In the Explanation of Review (EOR) below, SCIF allowed $0.00 for each test, with the rationales:
“THIS PROCEDURE IS INCLUDED IN THE VALUE OF ANOTHER PROCEDURE PERFORMED ON THE SAME DATE.”
“No separate payment was made because the value of the service is included with the value of another service performed on the same day.”
SCIF declared the diagnostic testing to be “included” in the cost of the Medical-Legal evaluation the provider reported with ML201. This is incorrect.
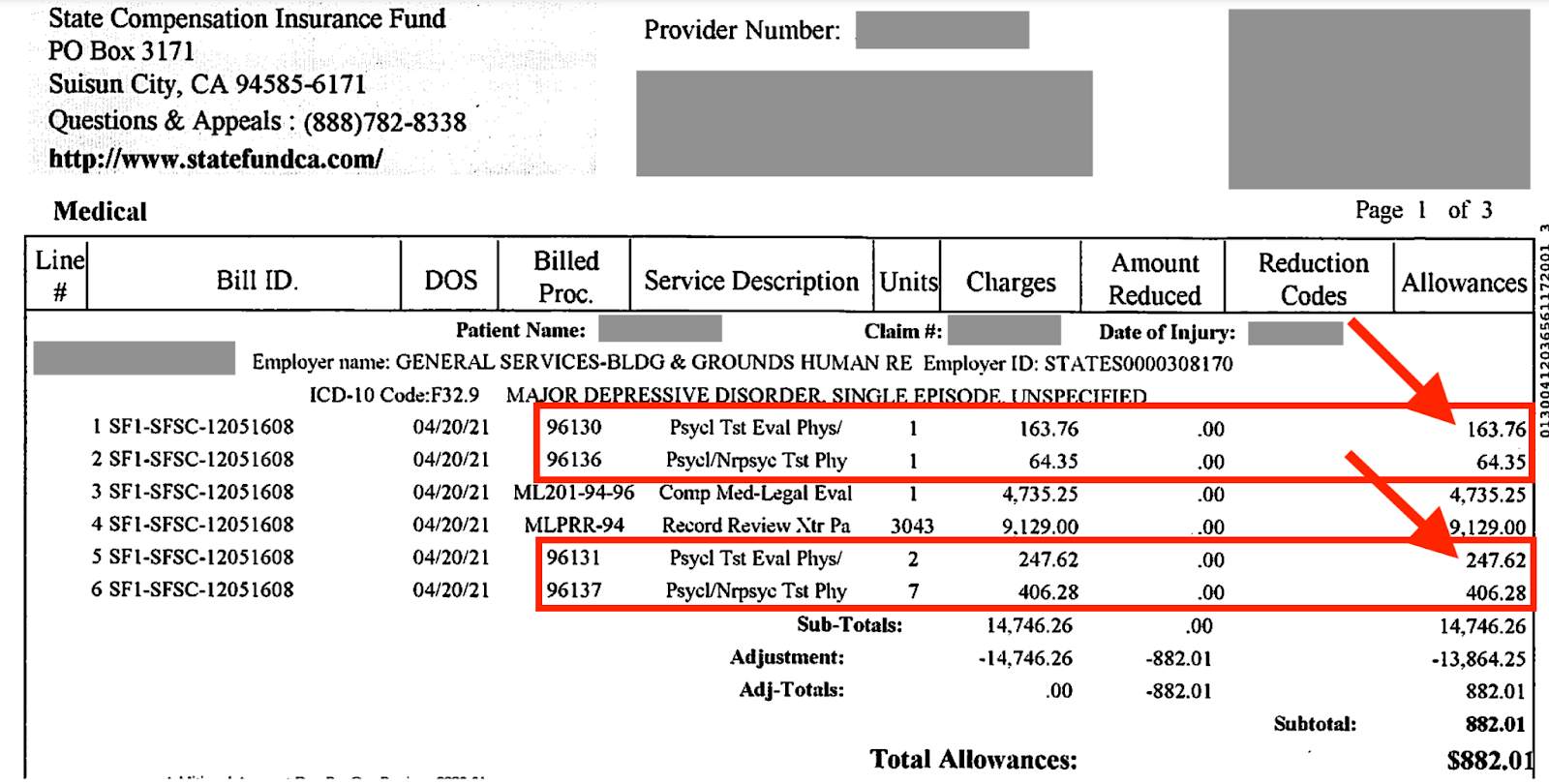
To their credit, SCIF realized their mistake, even before the physician had a chance to appeal for proper reimbursement. In an act of self-correction, SCIF remitted a second EOR and a second check for the diagnostic testing:
Notably, Zurich Insurance also made this mistake, and just like SCIF, corrected their incorrect adjustment before the provider sent an appeal.
Unfortunately, relying on claims administrators to police themselves is not an ideal revenue management strategy. If your practice is improperly denied payment for diagnostic testing necessary to complete a Medical-Legal evaluation, recover the owed revenue by submitting a Second Review appeal within 90 days, with the following language:
For the medical-legal evaluation, adequate diagnostic tests were not included in the medical information (i.e. current and relevant test results) sent by the parties. To complete the medical-legal evaluation, the evaluator performed diagnostic tests. Per the DWC reimbursement is due for said testing: “A claims administrator must pay for a diagnostic test ordered by an AME or QME as long as the subjective complaints and physical findings that warrant the necessity for the test are included in the medical/legal evaluation report.”
If the claims administrator denies the diagnostic charges, request Independent Bill Review (IBR). Include the language above, as well as documentation supporting the necessity of the diagnostic testing, in your IBR submission.
Get paid in full and on time. With quick & easy tools for authorization, billing, and appeals, DaisyBill helps protect your bottom line. Reach out to learn more.
CONTACT DAISYBILL
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.



.png)