SCIF Inept UR #6: Non-MTUS Guidelines Strike Again
Once again, State Compensation Insurance Fund (SCIF) and EK Health denied surgery for an injured worker by citing unadopted, alternative treatment guidelines outside of California’s designated Medical Treatment Utilization Schedule (MTUS).
With the worker reportedly in severe pain, a physician requested surgery with precise adherence to California workers’ compensation laws, regulations, and rules. In their response, SCIF and EK Health made up their own rules and applied treatment guidelines that kept appropriate treatment out of reach.
Worse, the denial details were a minefield of language seemingly designed to preclude any possibility of Independent Medical Review (IMR), the only recourse for an injured worker denied care deemed medically necessary by their physician.
The provider’s successful navigation of SCIF and EK Health’s nonsensical roadblocks — at great expense of time and practice administrative resources — is the only reason the surgery was ultimately approved after an agonizing, pointless delay.
As always, the injured worker (forced to endure months of suffering) is the only one on whom the consequences of California’s unregulated, indefensibly broken UR system fall.
Step by step below, we outline what this provider went through to overcome the obstacles created by SCIF and EK Health’s preference of undesignated treatment guidelines over the MTUS — all while the injured worker waited for relief.
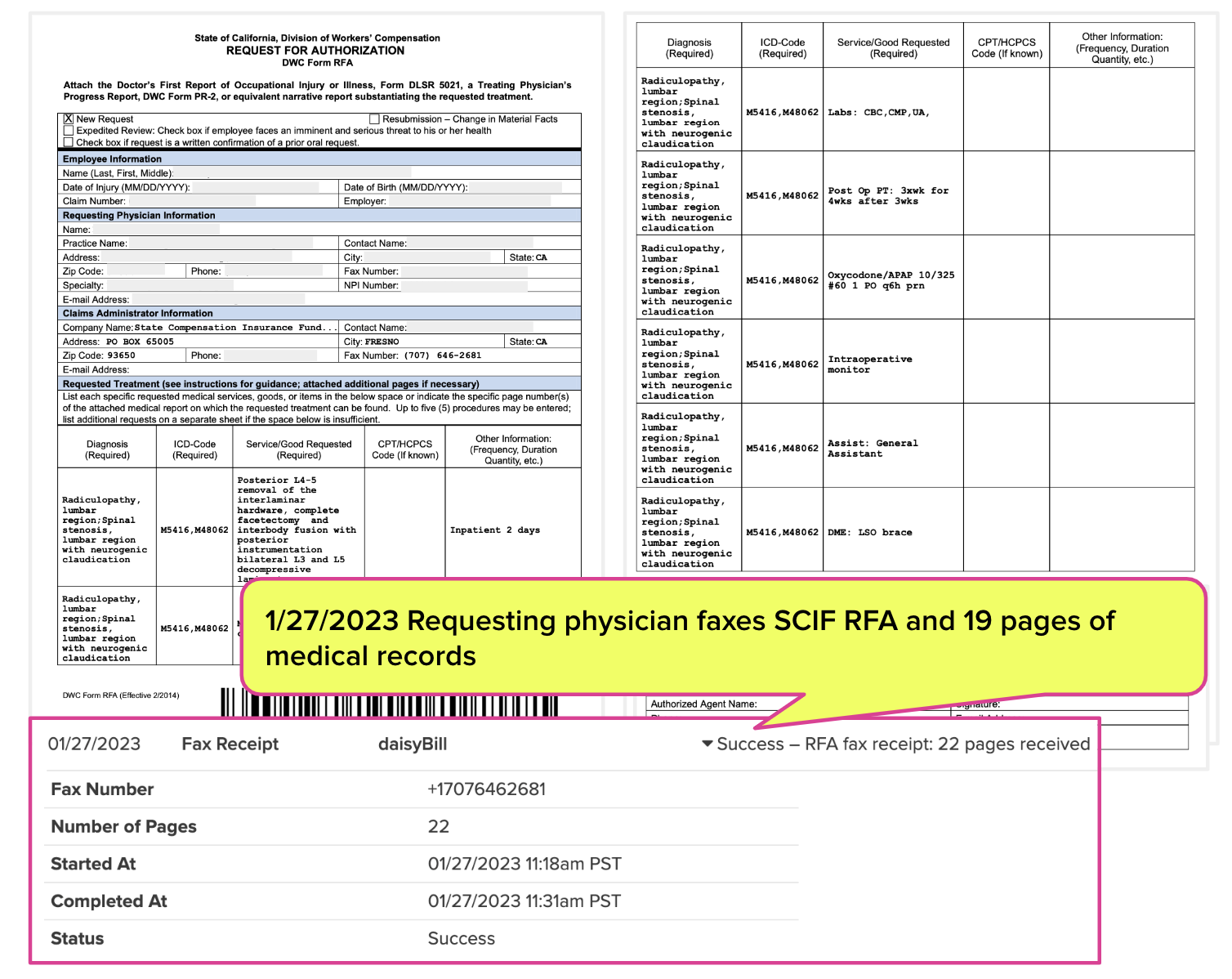
1. Physician Faxes SCIF 22 Page RFA
After sustaining a debilitating back injury lifting boxes in 2021, the worker received an initial surgery and returned to work. However, the worker began experiencing increasingly severe pain starting in December 2022.
Despite undergoing a slew of more conservative treatments (massage, physical therapy, chiropractic, acupuncture, epidural steroid injection, and daily at-home exercises), the injured worker’s pain increased significantly, necessitating multiple emergency room trips.
In January 2023, the physician faxed SCIF an RFA and 19 pages of medical records requesting approval for a new surgical treatment.
In the documentation, the physician specifically documented the requested surgery’s appropriateness and necessity according to the MTUS, stating:
“This patient satisfies ONE OR MORE of the ACOEM/MTUS guidelines necessary for approval of the recommended Lumbar Decompression and Fusion surgery as noted below.”
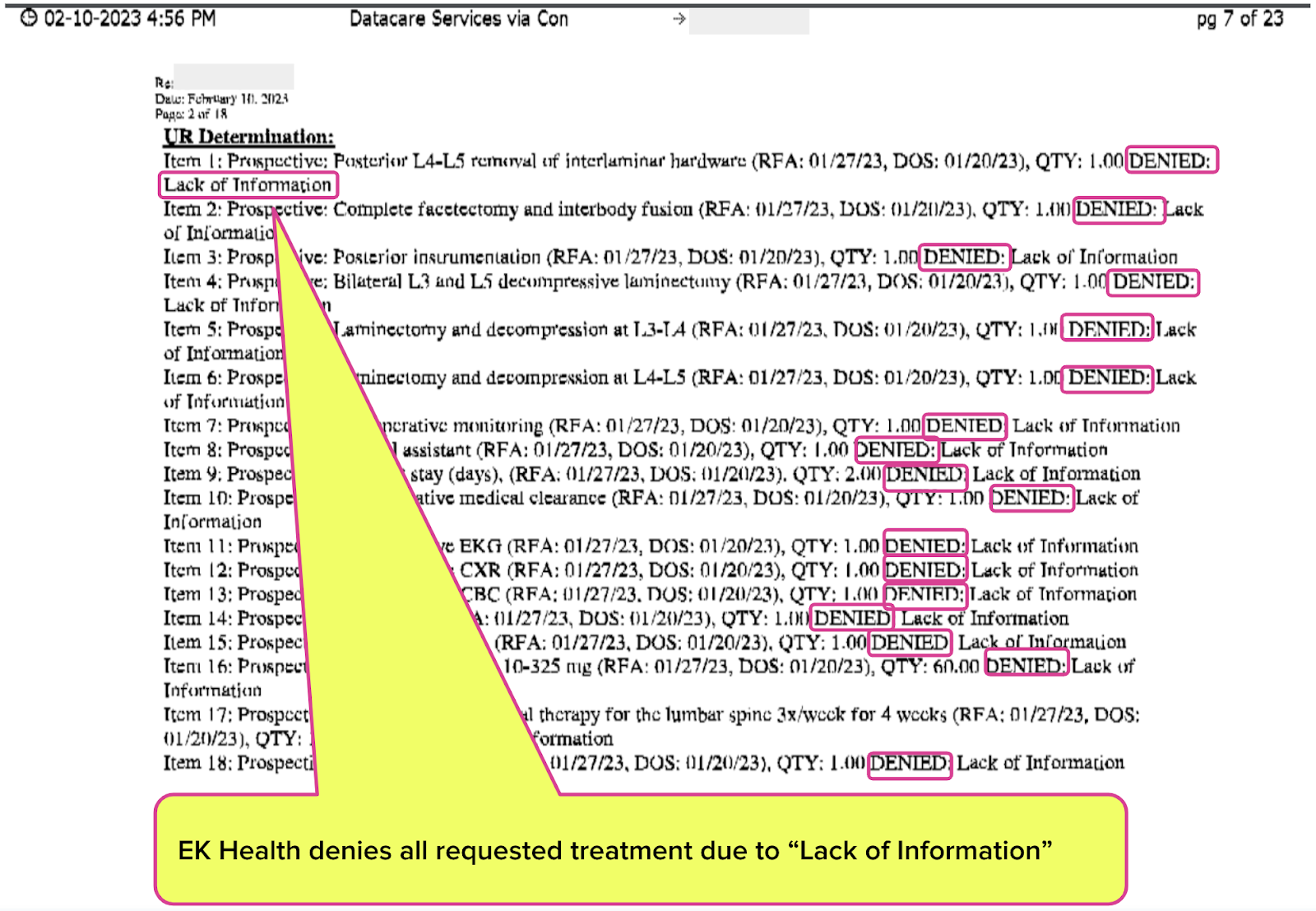
2. EK Health Denies Surgery for “Lack of Information”
SCIF forwarded the RFA to its Utilization Review Organization (URO), EK Health. EK Health faxed the requesting physician a 23-page UR decision denying the surgery due to a “Lack of Information.”
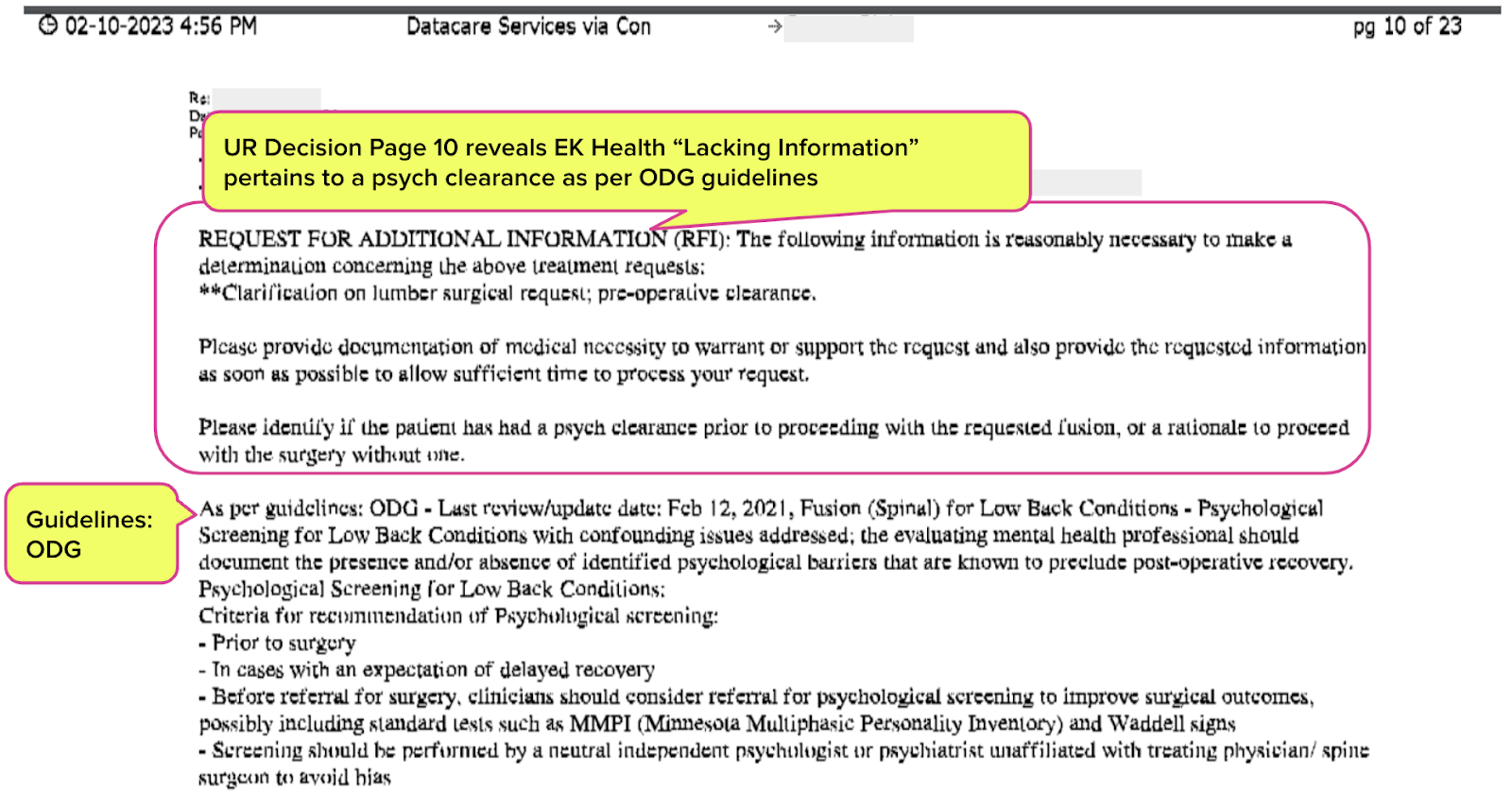
3. EK Health Applies ODG Guidelines Instead of MTUS
On page 10 of the faxed UR decision, EK Health lists the missing information that resulted in the denial decision:
“Please identify if the patient has had a psych clearance prior to proceeding with the requested fusion, or rationale to proceed with the surgery without one.”
To support the request for a psych clearance, the EK Health UR decision listed the surgical guidelines from the “Official Disability Guidelines” (ODG) offered by a subsidiary of the Hearst Health Network that requires a psych clearance. Per the ODG:
“Before referral for surgery, clinicians should consider referral for psychological screening to improve surgical outcomes.”
California law and regulations direct treating physicians, UR physicians, and IMR expert reviewers to follow the guidelines outlined in the MTUS for medical necessity determinations. Accordingly, the medical documentats the physician included with the RFA referenced MTUS guidelines.
Of course, the physician did not include the psych clearance information required by the completely inapplicable ODG. In an attempt to obtain the (inapplicable) psych clearance, EK Health repeatedly hassled the requesting physician as follows:
- 2/3/2023 faxed a Request for Information (RFI)
- 2/7/2023 left a voicemail @ 10:59 AM regarding the RFI
- 2/7/2023 faxed a copy of the RFI
- 2/9/203 left a voicemail @ 3:52 regarding the RFI
- 2/9/2023 faxed a copy of the RFI
- 2/10/2023 called physician (no voicemail left)
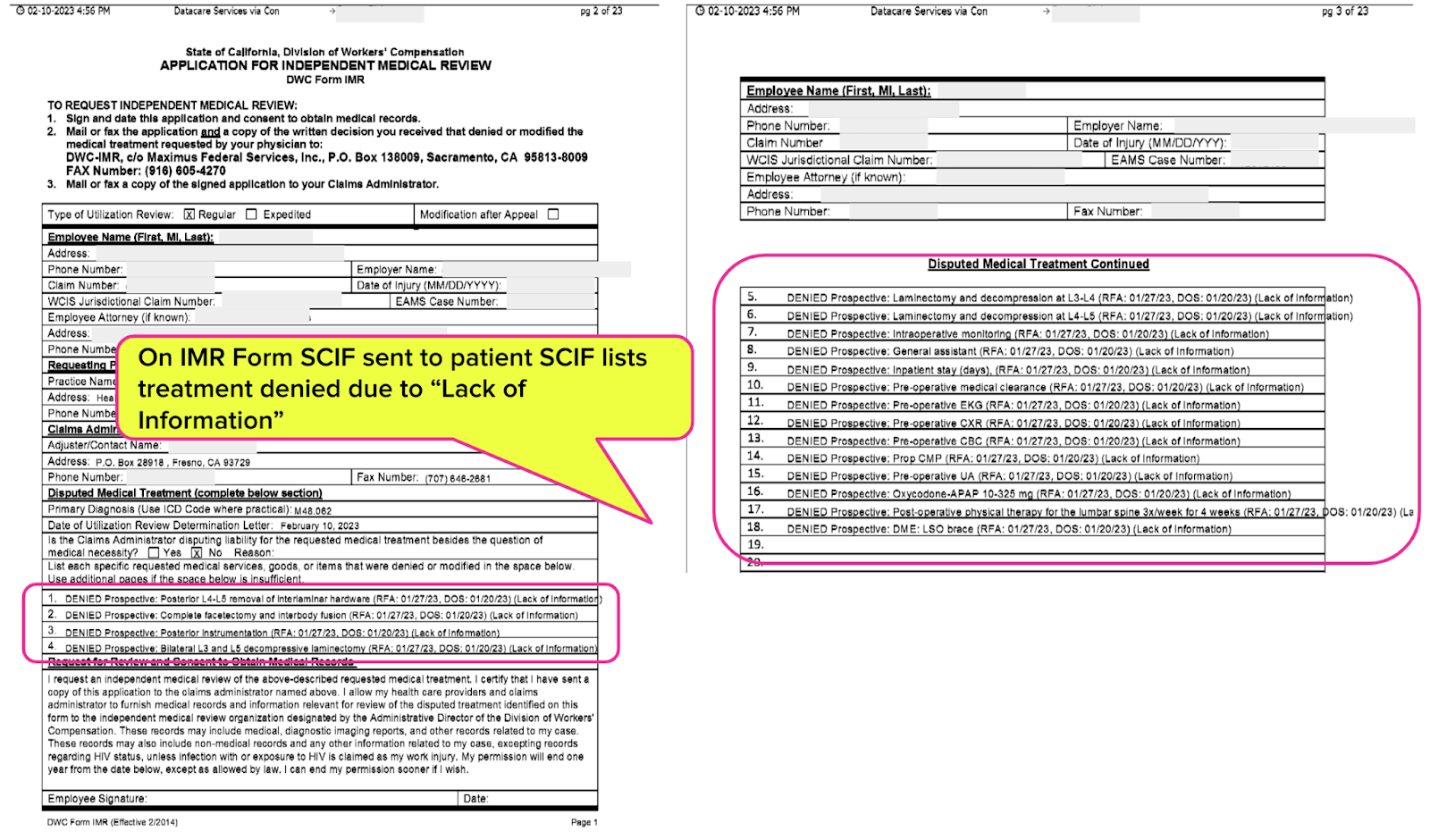
4. SCIF’s IMR Form Precludes IMR
Upon denying or modifying medical care, California Labor Code Section 4610.5. dictates that the insurer must send the injured worker an IMR form completed by the insurer so the injured worker can appeal the UR decision.
Below is the IMR form SCIF completed and sent to the injured worker, which cited “Lack of medical information” as the denial reason.
According to DWC IMR rules, an authorization dispute is deemed ineligible for IMR if the UR decision “does not reflect a determination of medical necessity (conditional non-certification).” As further explanation, the DWC defines a “conditionally non-certified decision (CNC)” as follows [emphasis added]:
“A UR decision that has been denied because the treating physician has not provided the medical information requested by the claims administrator that is required to make a medical necessity determination on the treatment recommendation.”
SCIF alleges that the physician failed to provide the medical information necessary to make a medical determination, presumably referring to the superfluous psych clearance recommended by the inapplicable ODG guidelines. Therefore, according to DWC rules, the dispute is ineligible for IMR.
Conveniently for SCIF, the DWC has devised IMR rules which allow SCIF to:
- Complete the IMR form on behalf of the injured worker
- Assert non-receipt of inapplicable medical documentation
- Circumvent IMR by claiming missing medical information
What Does It Take to Get Care Authorized?
Instead of receiving the care considered medically necessary and appropriate by the treating doctor, this injured worker had to wait for:
- The treating doctor to submit another RFA requesting the ODG-imposed psych clearance
- A psychologist appointment to conduct the screening
- The treating doctor to submit yet another RFA again requesting the surgery
- EK Health (of the notoriously late UR decisions) to conduct UR and communicate approval to the treating doctor
As noted, this added three months to the process for this injured worker.
Three months of continuing, worsening back issues. Three months of continued uncertainty about the future. Three months of, presumably, significant physical pain. All because EK Health and SCIF found treatment guidelines they prefer over those designated by California law.
For SCIF and EK Health to make the purposeful decision to stray from the MTUS and impose significant obstacles to care seems less like prudence and more like heartlessness. How much work must the doctor undertake to obtain approval for medically necessary treatment? How many trips to the ER does the injured worker have to make?
What have SCIF and EK Health accomplished besides adding to an injured worker’s torment by creating this delay?
Injured workers deserve answers to these questions and a less blatantly corrupted UR system.
Authorization is the first hurdle in the workers’ comp obstacle course. Enjoy 30-second RFA submission and automatically tracked UR decisions with daisyAuth — request a demo below!
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.



That is absolutely infuriating and disgusting. I feel terrible for the patient and his family. Shame on SCIF and EK.
This is why we are refusing to see certain carriers. The hoops they require us to jump through is ridiculous.