SCIF Inept UR #5: EK Health Ignores MTUS, Denies Surgery
Why is it so difficult to get treatment for a work-related injury? At least in California, most of the answer is a broken UR system that allows insurers to withhold potentially medically necessary care.
With zero regulatory oversight, this mangled UR system enriches insurers by allowing insurers and their Utilization Review Organizations (UROs) to deny paying for treatment with impunity.
After working for a quarter century at a California corrections facility, sustaining multiple injuries over the years (including during an attack by an inmate), and returning to work each time, a veteran corrections officer was injured again in a work-related car accident. Subsequently, State Compensation Insurance Fund refused to authorize surgery that the officer’s treating physician deemed necessary — for arguably dubious reasons.
According to the Utilization Review (UR) decision issued by EK Health (SCIF’s URO), the surgery was denied because the physician failed to provide documentation of a psych clearance as recommended by the “Official Disability Guidelines” (ODG).
However, California mandates that physicians adhere to California’s Medical Treatment Utilization Schedule (MTUS), not the ODG. Every accredited URO (and certified insurer) should know that the ODG are not the treatment guidelines adopted by California to determine medical necessity.
As demonstrated below, EK Health hassled a physician to provide a psych clearance required by (inapplicable) ODG criteria, even though the (applicable) MTUS guidelines require no such clearance. When the physician responded that the injured worker did not require a psych clearance, EK Health denied the surgery for “lack of information,” thereby precluding the corrections officer from seeking justice from (the extremely flawed) Independent Medical Review (IMR) system.
The plight of this corrections officer demonstrates (once again) that insurers and UROs make up their own rules, delaying or denying possibly medically necessary care. As always, the injured worker is the only one who will pay the price in the consequence-free UR environment California has established for payers.
SCIF/EK Health Send Late, 24-Page UR Decision
When more conservative treatments failed to resolve the corrections officer’s injury, the treating doctor determined that vertebral fusion of the lower back was warranted.
As required, the doctor submitted a formal Request for Authorization (RFA), to which the doctor attached 12 pages of supporting documentation to verify the necessity of the surgery.
In response to the RFA, EK Health faxed the physician a 24-page UR decision that was an illegible, barely intelligible heap of gobbledygook. Below, we present the EK Health UR decision to demonstrate two critical problems with California’s UR system:
- The illegible UR decision faxes torturing physicians and administrative staff. The lengthy blurred UR decision below is precisely as faxed to the provider. California, it’s 2023 — time to eliminate the fax machine as the preferred communication method.
- The critical need to require standardized UR decisions. The EK Health UR decision exemplifies the medical rubble dumped on providers, who must submit RFAs in a strictly standardized format while insurers may respond however they wish.
Hiking up our sewer pants and wading deep into EK Health’s morass of obfuscating words, we see that EK Health refused to authorize surgery without a preoperative psych clearance — a clearance that the MTUS does not require.
Step by step, below is what doctors must go through in their attempts to get treatments authorized — all while the injured worker waits, and waits, and waits.
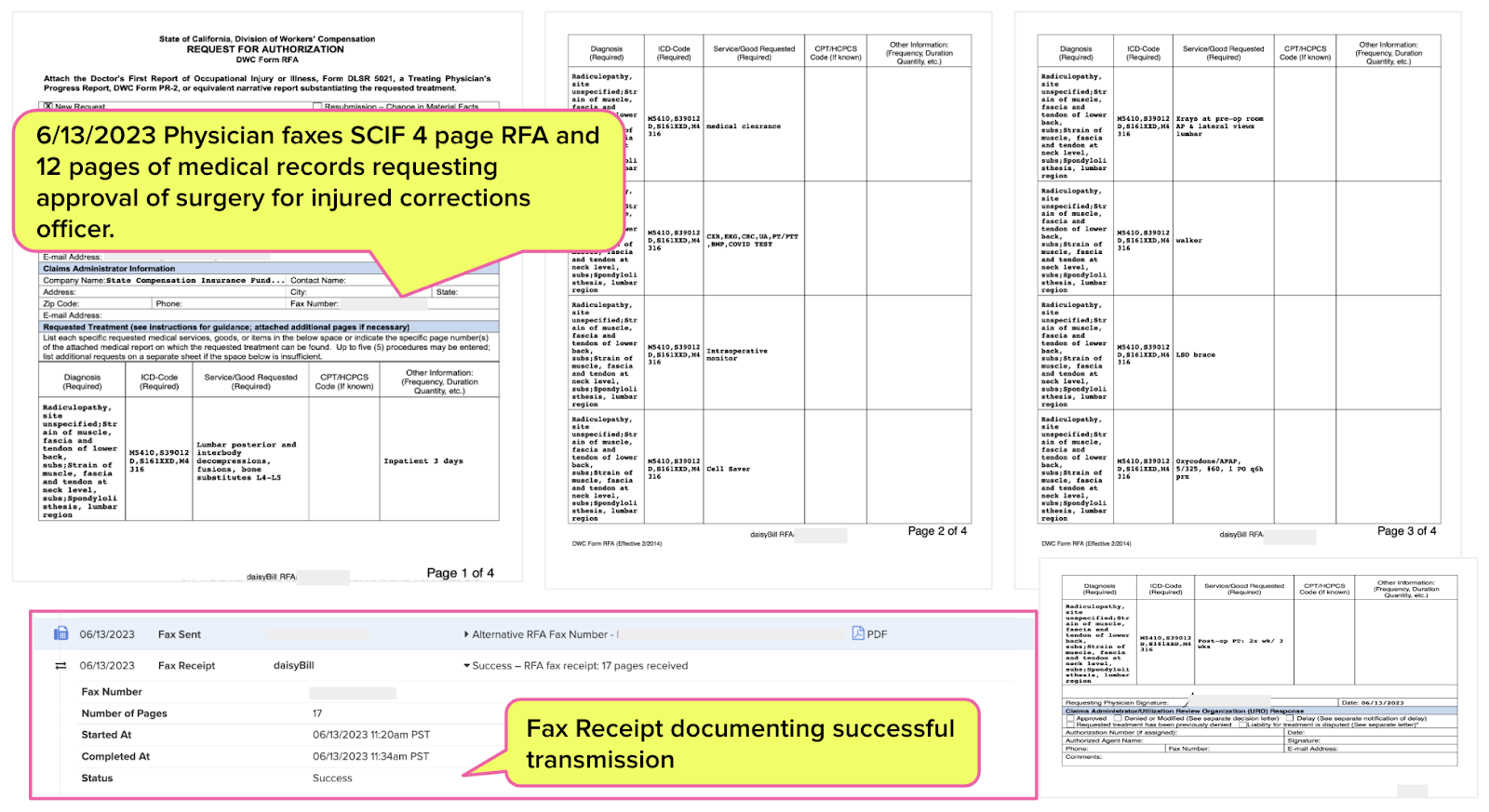
1. Physician faxed SCIF comprehensive 4-page RFA requesting spine surgery with 12 pages of medical documentation on 6/13/2023 @ 11:34 am PST
Per §9792.9.1. Utilization Review Standards: SCIF must respond with a Utilization Review (UR) decision within five (5) business days of receipt of the completed RFA – on or before 6/21/2023 @ 11:34 am PST.
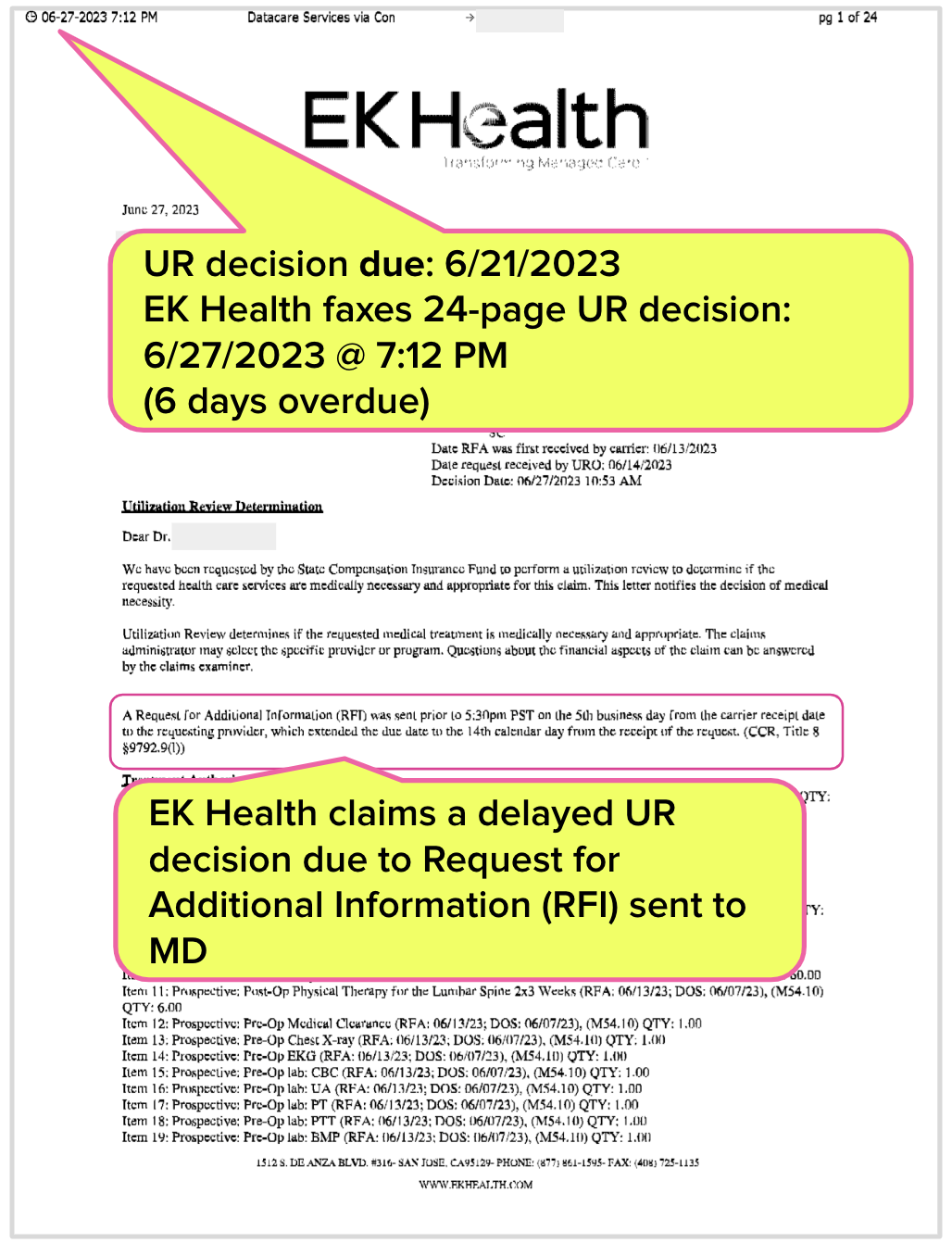
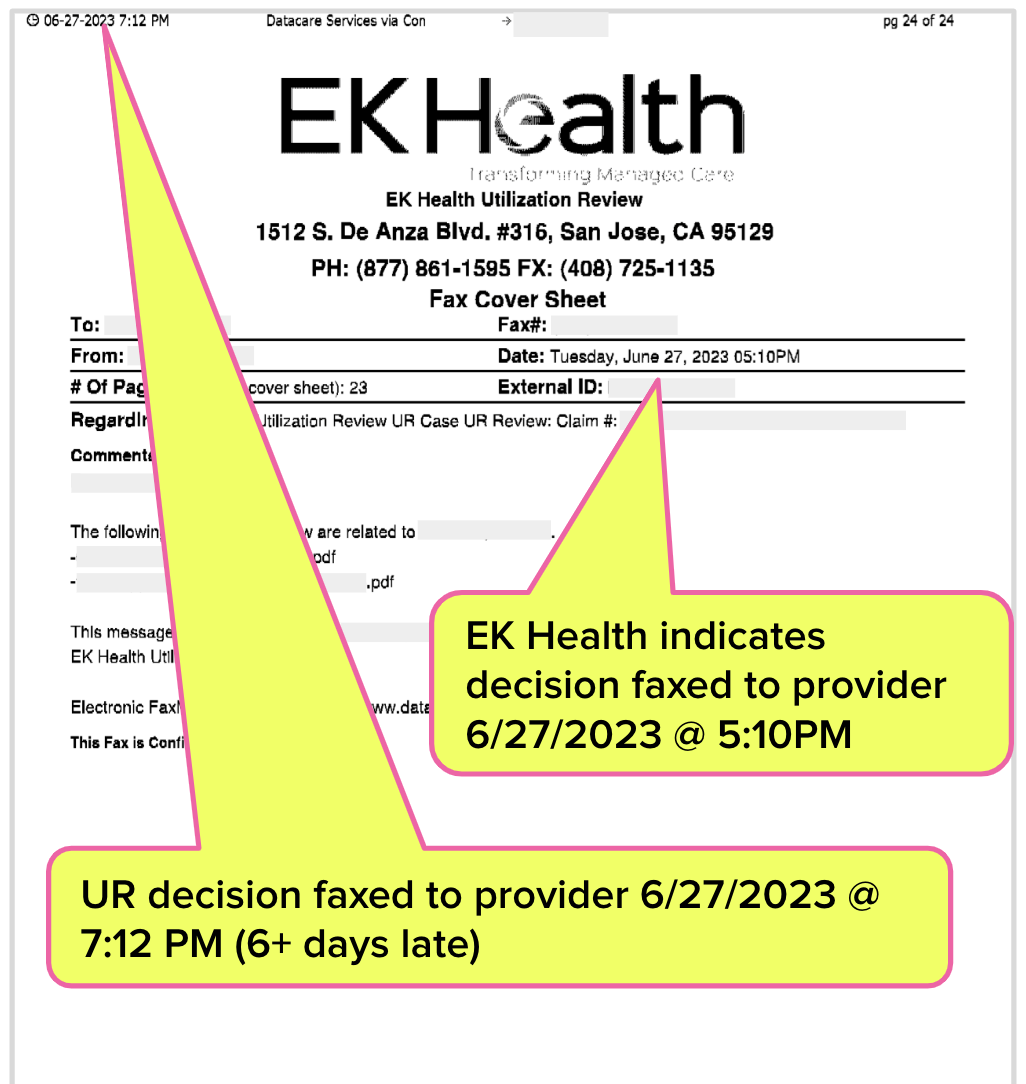
2. EK Health faxed physician a 24-page UR decision denying the requested surgery on 6/27/2023 @ 7:12 PM
Per §9792.9.1. SCIF may extend the UR decision timeframe up to 14 calendar days if the physician fails to send all of the information reasonably necessary to make a decision. In its UR decision, EK Health requested that the physician provide additional information.
Important Note: EK Health faxed the UR decision after working hours on 6/27/2023, making the delayed decision untimely. Fortunately for SCIF and EK Health, there is zero regulatory oversight to enforce the timely delivery of UR decisions.
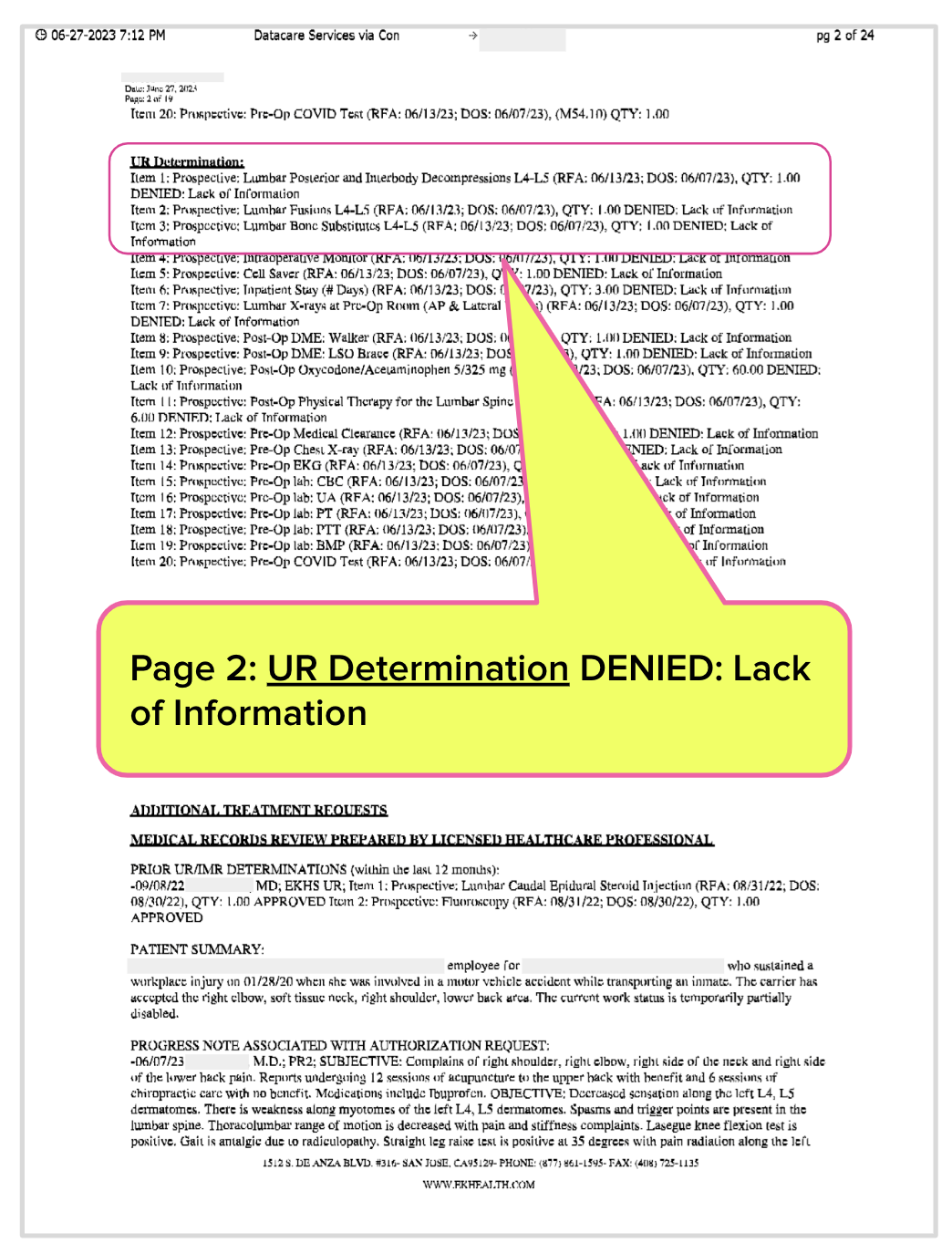
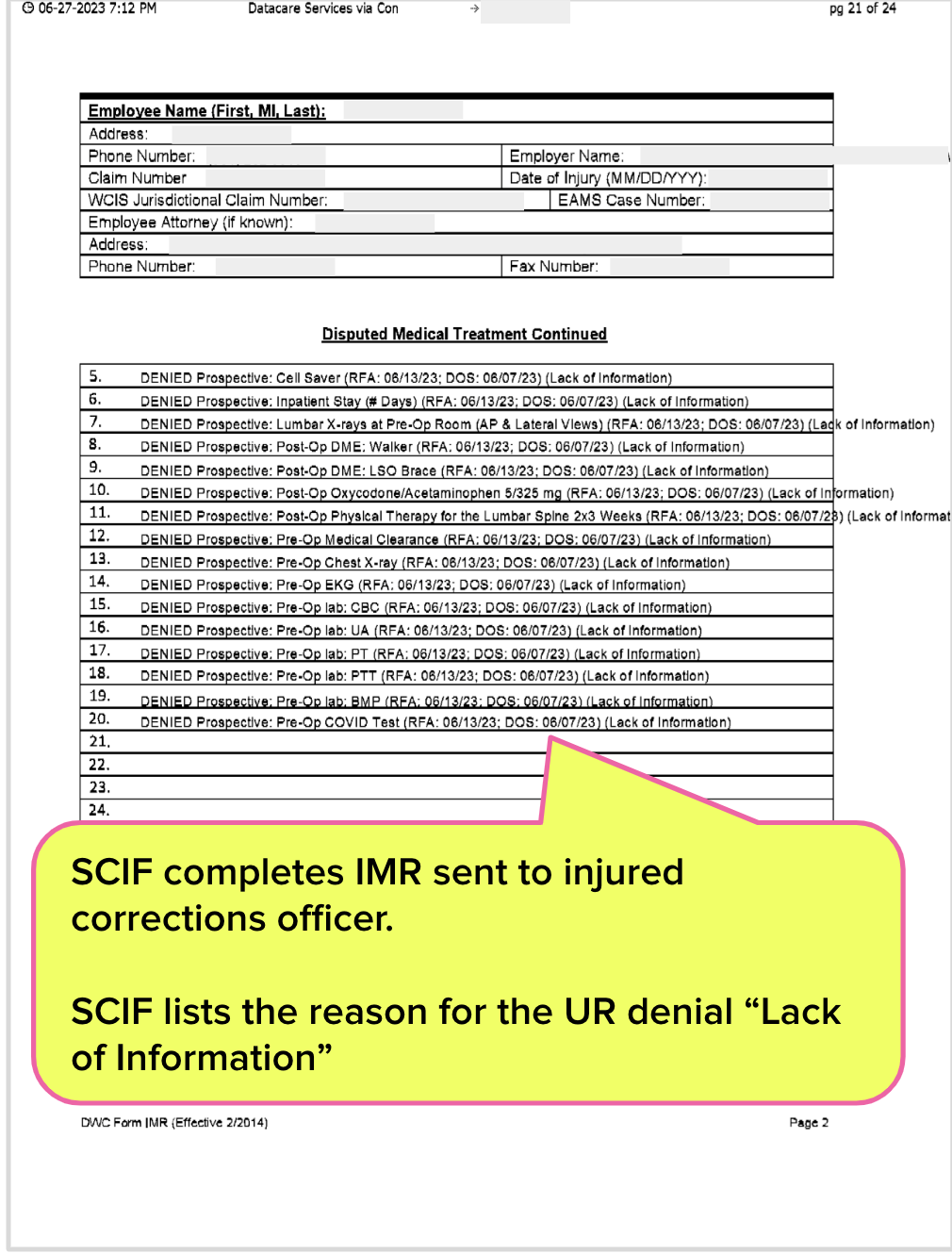
3. UR Decision: EK Health denies surgery due to “Lack of Information”
The EK Health UR decision denies the surgery for “Lack of Information.” Yet, pages 1 and 2 of the UR decision fail to inform the physician as to the details of the alleged missing information.
4. EK Health hassles MD demanding proof of psych clearance
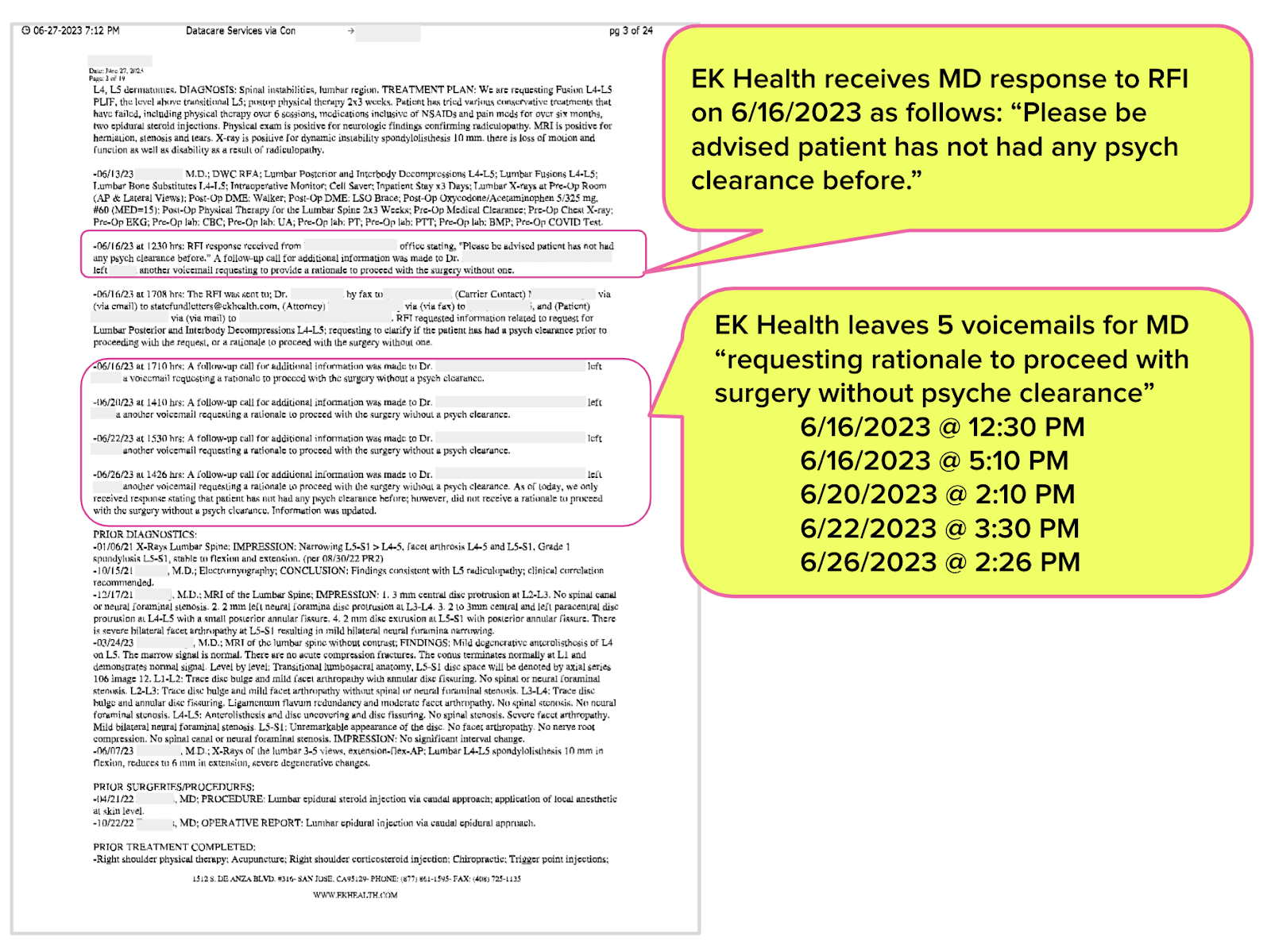
Page 3 of the UR decision describes the physician’s response to EK Health's Request for Information (RFI) ) which allowed EK Health to delay the UR decision. The UR decision states that the physician’s office responded to the RFI with the following information: “Please be advised patient has not had any psych clearance before.”
From this snippet of information, we can deduce that EK Health demanded that the physician provide additional information about a “psych clearance.”
Not satisfied with the physician’s RFI response, EK Health left the physician six voicemails “requesting rationale to proceed with surgery without psych clearance.”
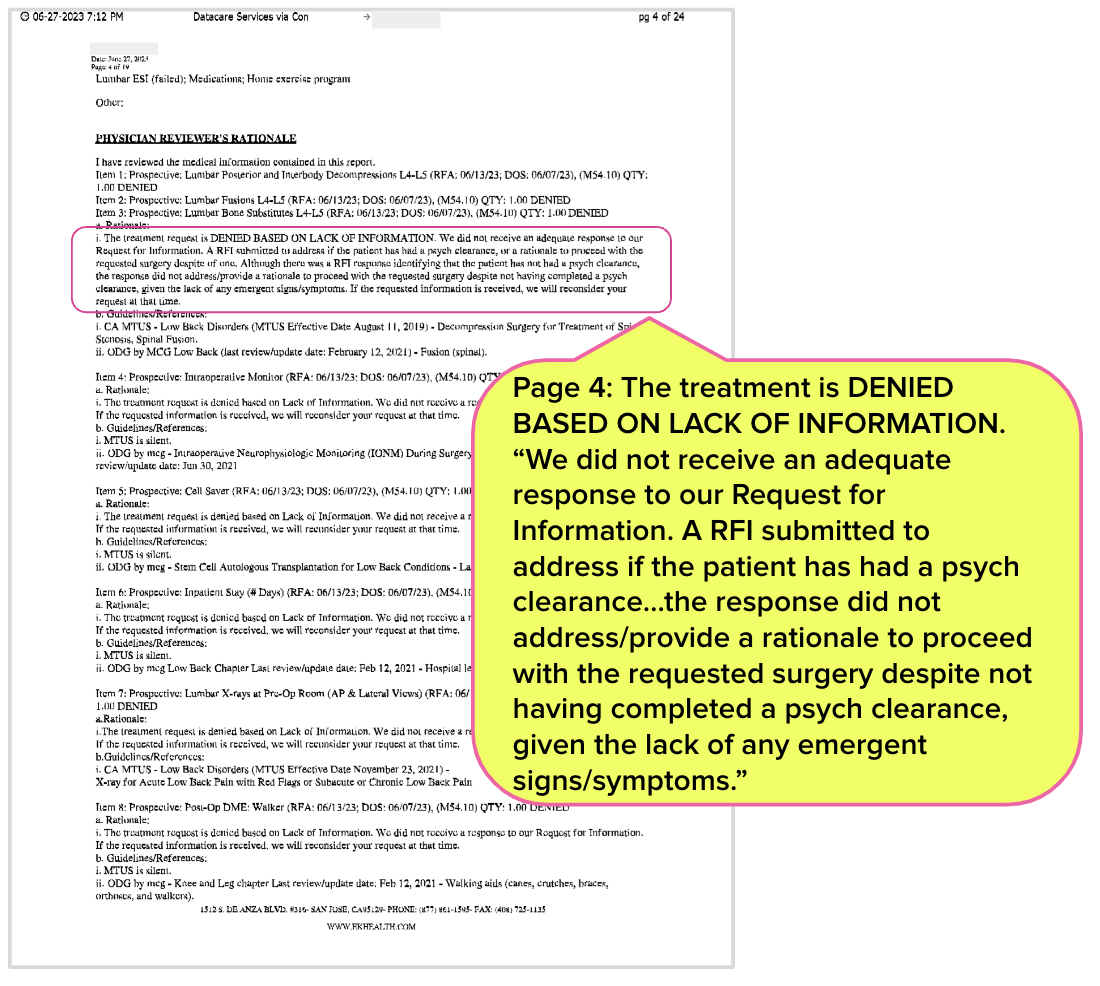
5. UR Decision: Details of “Lacking Information” provided
Page 4 of the UR decision finally (if incoherently) explains the denial is due to the physician failing to provide a “rationale” for not completing a psych clearance for the surgery, even though the injured worker did not exhibit any “emergent signs/symptoms.”
This EK Health decision forced the physician and their administrative staff to wade through almost four pages of tiny, illegible fax font simply to ascertain the reason SCIF refused to pay for the surgery.
6. UR Decision Pages 5 through 7: 3 Pages of UR Gibberish
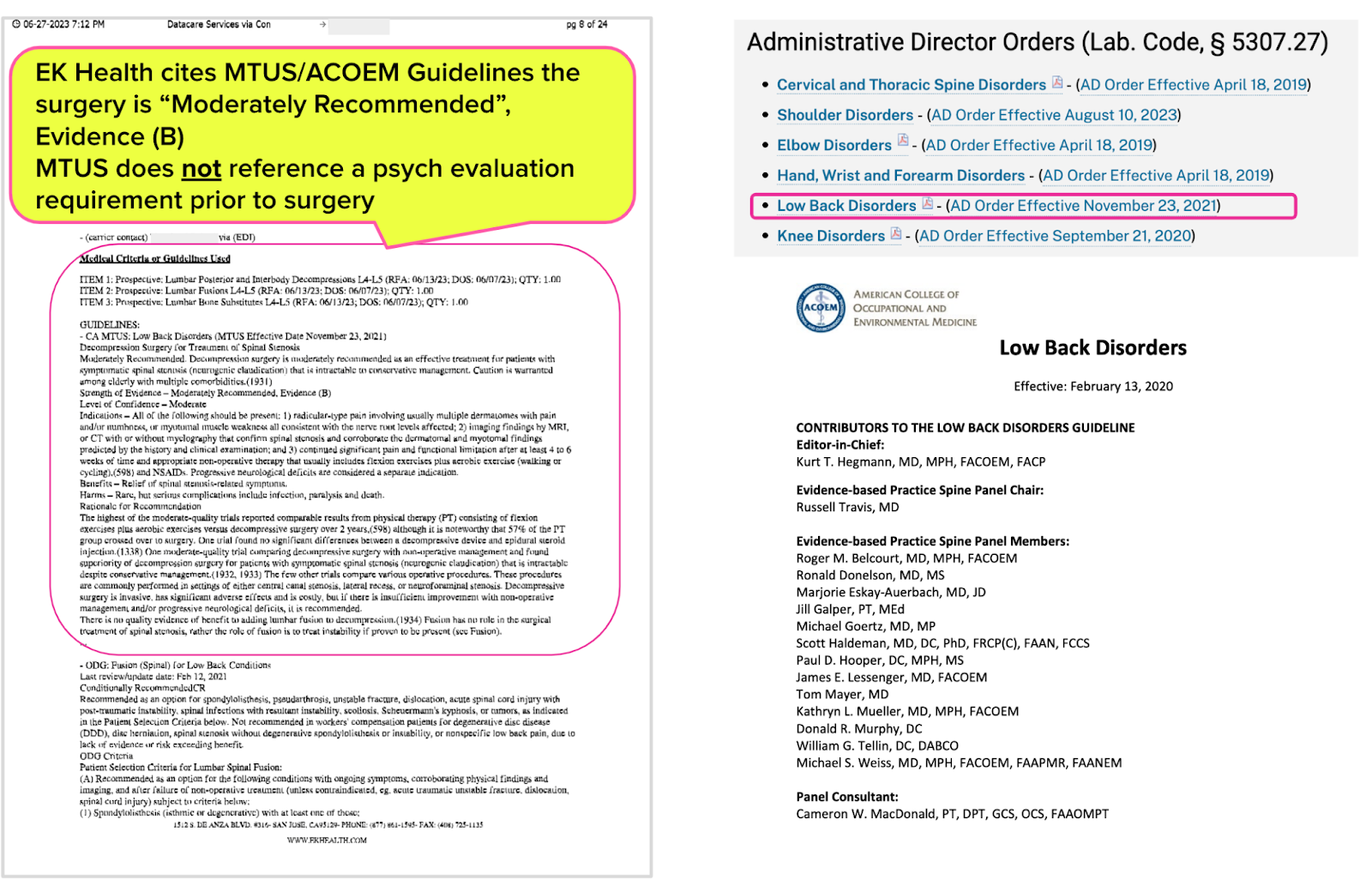
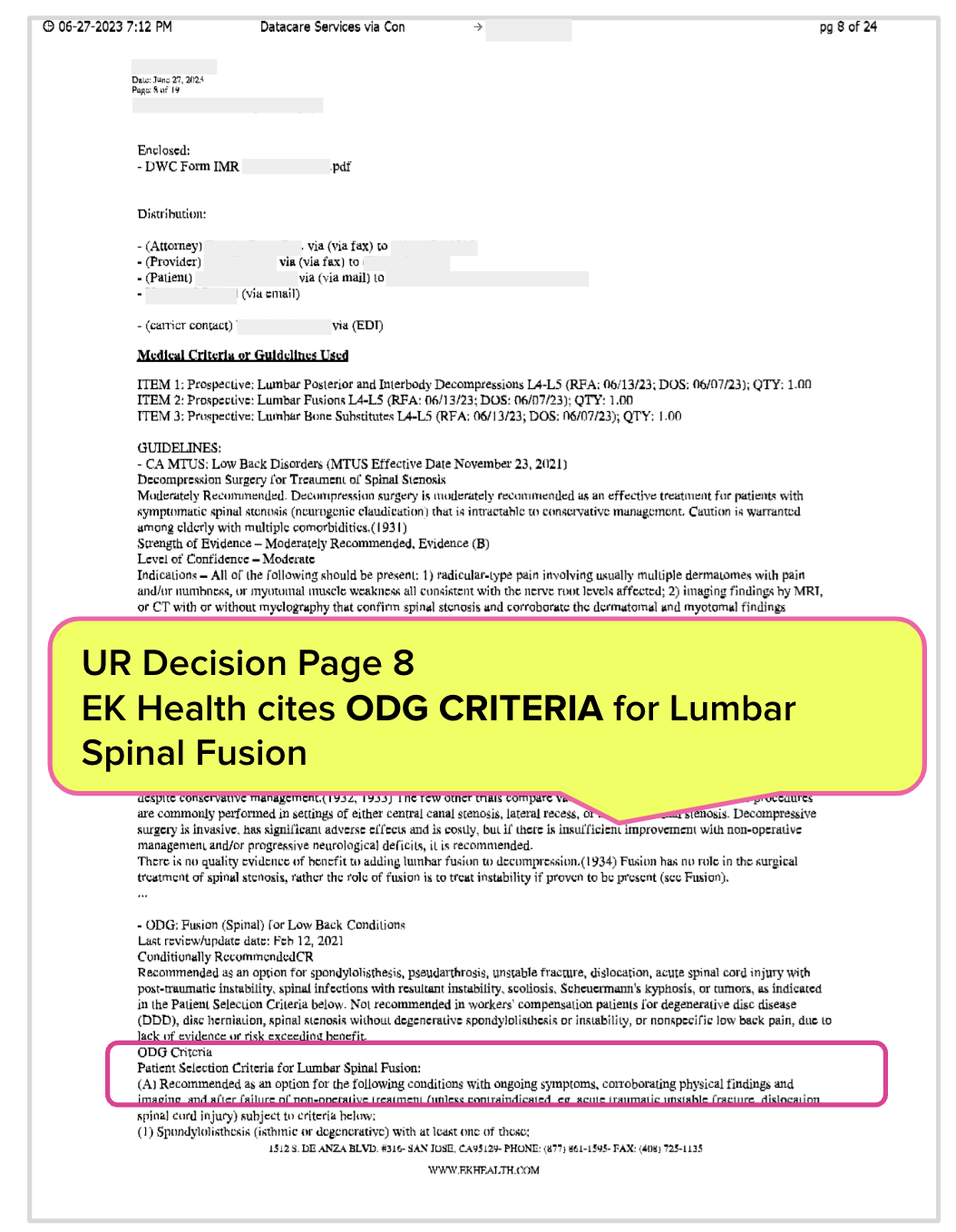
7. UR Decision: MTUS Guidelines applicable to surgery requested by the physician
California law and the Division of Workers’ Compensation (DWC) mandate:
“When an employee is injured at work, he or she is entitled to receive reasonable and necessary medical treatment to cure or relieve the injury. The Medical Treatment Utilization Schedule (MTUS) is a set of regulations found in title 8, California Code of Regulations section 9792.20 through 9792.27.23 that contain medical treatment guidelines and rules for determining what is reasonable and necessary medical care.”
Page 8 of the UR decision lists the Low Back Disorders MTUS guidelines adopted by the DWC effective November 23, 2021. The MTUS recommends the surgery and does not (repeat: NOT) require a psych evaluation/clearance before surgery.
However, because the physician failed to provide a “rationale to proceed with surgery without psych clearance” (which the MTUS does not require), EK Health and SCIF
- Delayed a timely UR decision in pursuit of a pointless Request for Information (RFI) for psych clearance
- Repeatedly hassled the physician with voicemails demanding an inapplicable psych clearance
- Denied the injured worker access to care deemed medically necessary and appropriate by the physician and the MTUS
8. Why does EK Health list ODG Guidelines?
Page 8 of the EK Health UR decision also lists the ODG guidelines applicable to the surgery requested by the physician. Listing the ODG criteria seemingly makes little sense, given the applicability of the MTUS in California.
The ODG is produced by the former Work Loss Data Institute (WLDI), currently, a part of Milliman Care Guidelines, LLC (MCG), owned by the Hearst Health Network. Even the ODG website acknowledges that California has adopted the MTUS for treatment guidelines (not the ODG).
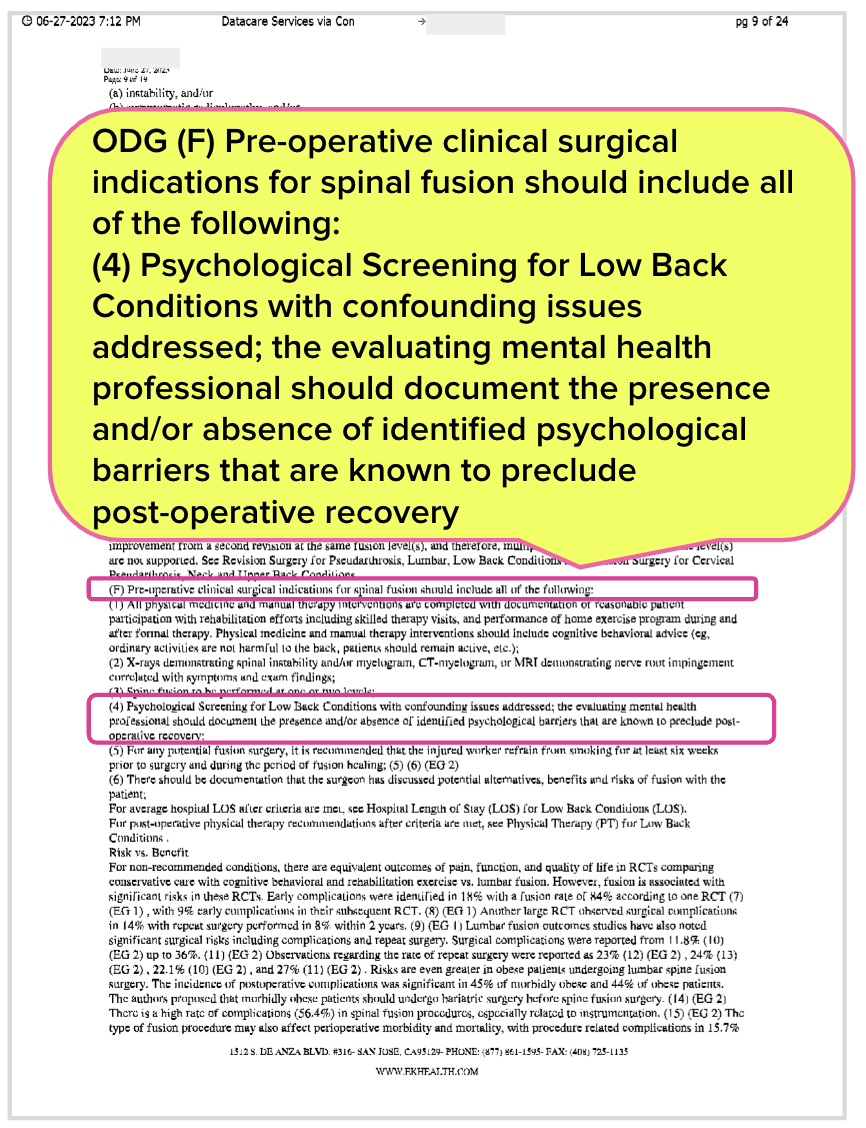
9. UR Decision: ODG Requires Psychological Screening
Page 9 of the UR decision lists that the ODG criteria for the surgery requested by the physician requires a “Psychological Screening for Low Back Conditions.”
With no regulatory oversight, EK Health and SCIF successfully used inapplicable ODG criteria to:
- Delay a timely UR decision in pursuit of an inapplicable Request for Information (RFI) based on ODG criteria
- Repeatedly hassle the physician with voicemails demanding the physician adhere to ODG requirements
- Deny the injured worker access to care deemed medically necessary, based on inapplicable ODG criteria
10. UR Decision: Pages 10 through 17 provides MTUS guidelines and (inapplicable) ODG criteria
For each of the goods and services the provider listed on the RFA, the EK Health UR decision recites both the MTUS and the inapplicable ODG criteria.
11. UR Decision: Pages 18 and 19 provide SCIF and Independent Medical Review (IMR) disclosures
California requires payers to include a form to request IMR with any decision denying the requested treatment so the injured worker can appeal. But as we know, IMR in practice has almost no value for injured workers.
12. UR Decision: Pages 20 through 23 provide the IMR sent to the injured corrections officer
In a future article, we’ll examine the IMR request form that SCIF sent to the injured worker and demonstrate that SCIF completed the form in a manner that likely precludes the injured worker from prevailing.
13: UR Decision: Page 24 Is the EK Health “Fax Cover Sheet”
The fax time EK Health lists on its cover sheet conveniently contradicts the actual fax time. As noted, EK Health claims a fax time of 5:10 PM instead of the recorded fax time of 7:12 PM on 6/27/2023.
Summary: Why is getting treatment for a work-related injury so challenging?
To a great extent, the answer is the unconscionably broken UR system, which features zero regulatory oversight. This skewed UR system allows SCIF to:
- Ignore medical documentation physicians fax with RFAs
- Fail to timely respond to UR decisions by sending inapplicable Requests For Information (RFIs)
- Burden physicians with lengthy (often unintelligible) faxed UR decisions
- Hassle physicians with repeated phone calls demanding inapplicable information
- Ignore MTUS guidelines
- Apply inapplicable ODG criteria to deny treatment
- Complete the IMR form in a manner that likely results in the DWC ruling the dispute ineligible for IMR
The plight of this corrections officer demonstrates (again) that insurers and UROs make up their own rules.
Authorization is the first hurdle in the workers’ comp obstacle course. Enjoy 30-second RFA submission and automatically tracked UR decisions with daisyAuth — request a demo below!
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.gif)
We too have a correctional officer that has been denied surgery 6 times in a 2 year period of time. He has seen a QME (twice) and another orthopedist who have all confirmed that he needs a Total Knee Replacement. The surgeon then modified his request to a partial knee replacement and again to a diagnostic arthroscopy which were all denied. The claim of lack of documentation and evidence for the procedure(s) is among the denial reasons. No matter how it was amended, it was denied. Two surgeons and a QME are all in agreement with a course of treatment which is repeatedly denied.
The patient ran out of disability and was forced to return to work in a modified capacity because of the delay. This is grossly unfair to the injured worker and is even more dangerous due to his line of work. He is now being forced back to the QME, who will again say that the patient requires surgery. EK Health will undoubtedly deny it.