SCIF Inept UR #2: Bungled Medical Records Strikes Again

Once again, the consequences of inept Utilization Review (UR) fall on an injured worker.
EK Health, conducting UR on behalf of State Compensation Insurance Fund (SCIF), denied a provider’s Request for Authorization (RFA) for continued cognitive therapy to address an injured worker’s head trauma.
Not for the first time, SCIF and its UR vendor somehow bungled essential medical documentation, leading to a denial of treatment that could mean the difference between recovery and a life of continued suffering from a cognitive disability.
Why did EK Health deny this treatment for an accepted injury? According to the bloated, rambling, barely comprehensible UR decision, EK Health required “an updated medical report on the patient’s progress and goals.” However, the doctor had faxed SCIF precisely that: a 9-page medical report detailing the injured worker’s progress and goals.
This treatment denial is valid for an entire year per California law (and according to Division of Workers’ Compensation (DWC) rules, this denied treatment is likely ineligible for Independent Medical Review).
That’s a year of therapy and potential progress, possibly lost irrevocably, because SCIF (or its UR vendor) failed to manage medical documentation that the physician properly faxed with an RFA.
The missing documentation led to EK Health denying treatment, which saved SCIF from paying for critical therapy. With little (read: zero) regulatory oversight of UR compliance enforcement, SCIF and EK Health have little (read: zero) incentive to get their collective act together.
As usual, the injured worker is the only one who will suffer (potentially life-altering) consequences.
Cognitive Therapy Proves Effective, MD Requests More
The worker suffered a traumatic head injury resulting in significant cognitive impairment. SCIF had previously approved cognitive therapy, which the injured worker received.
In May 2023, the Primary Treating Physician (PTP) faxed an RFA to SCIF requesting authorization for continued rehabilitative therapy. Along with the RFA form, the physician faxed a 9-page comprehensive report from the treatment center that provided the prior therapy.
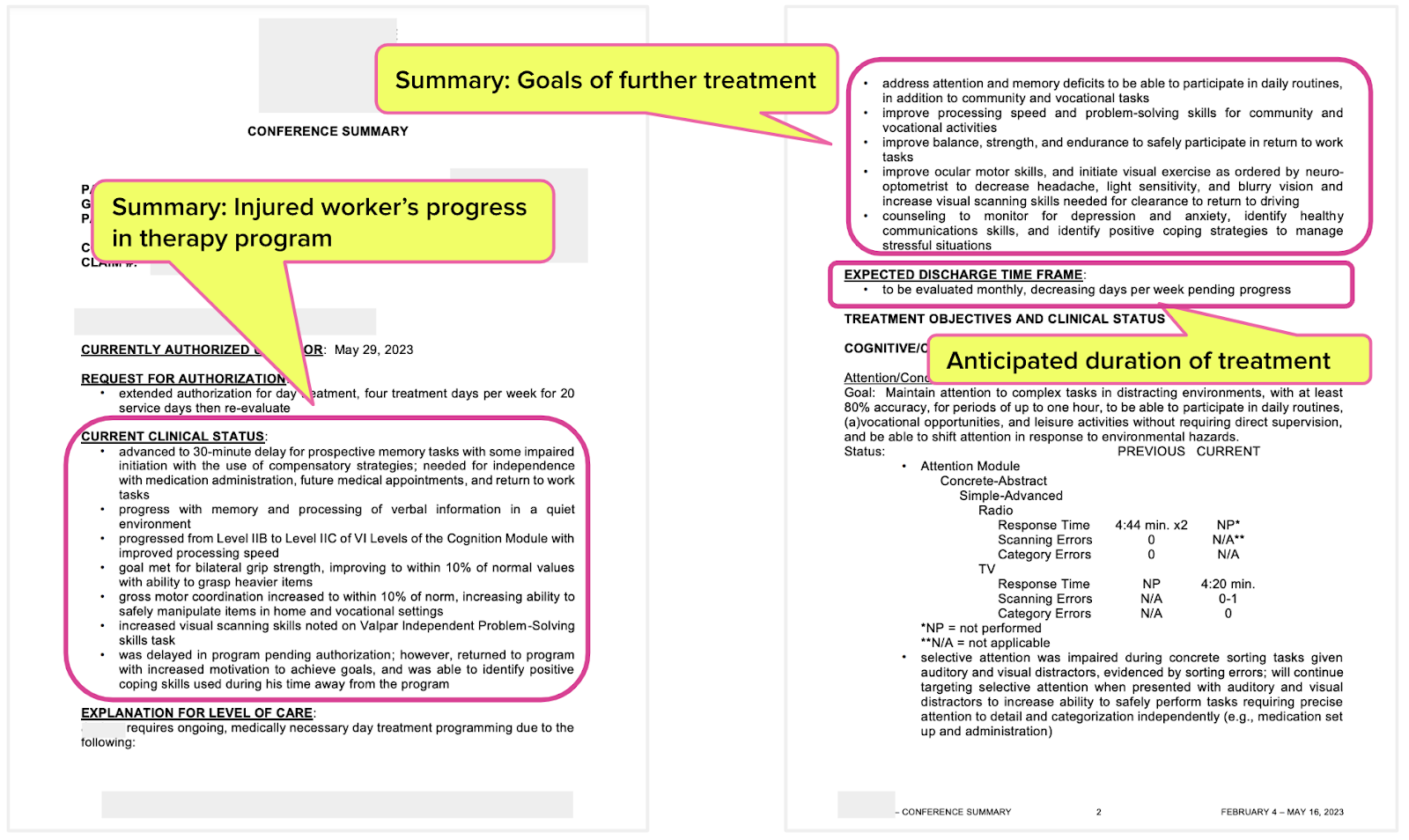
The first two pages of the report (below) offered a summary of the following:
- The injured worker’s progress in the program
- Anticipated goals of further treatment
- Anticipated duration of treatment
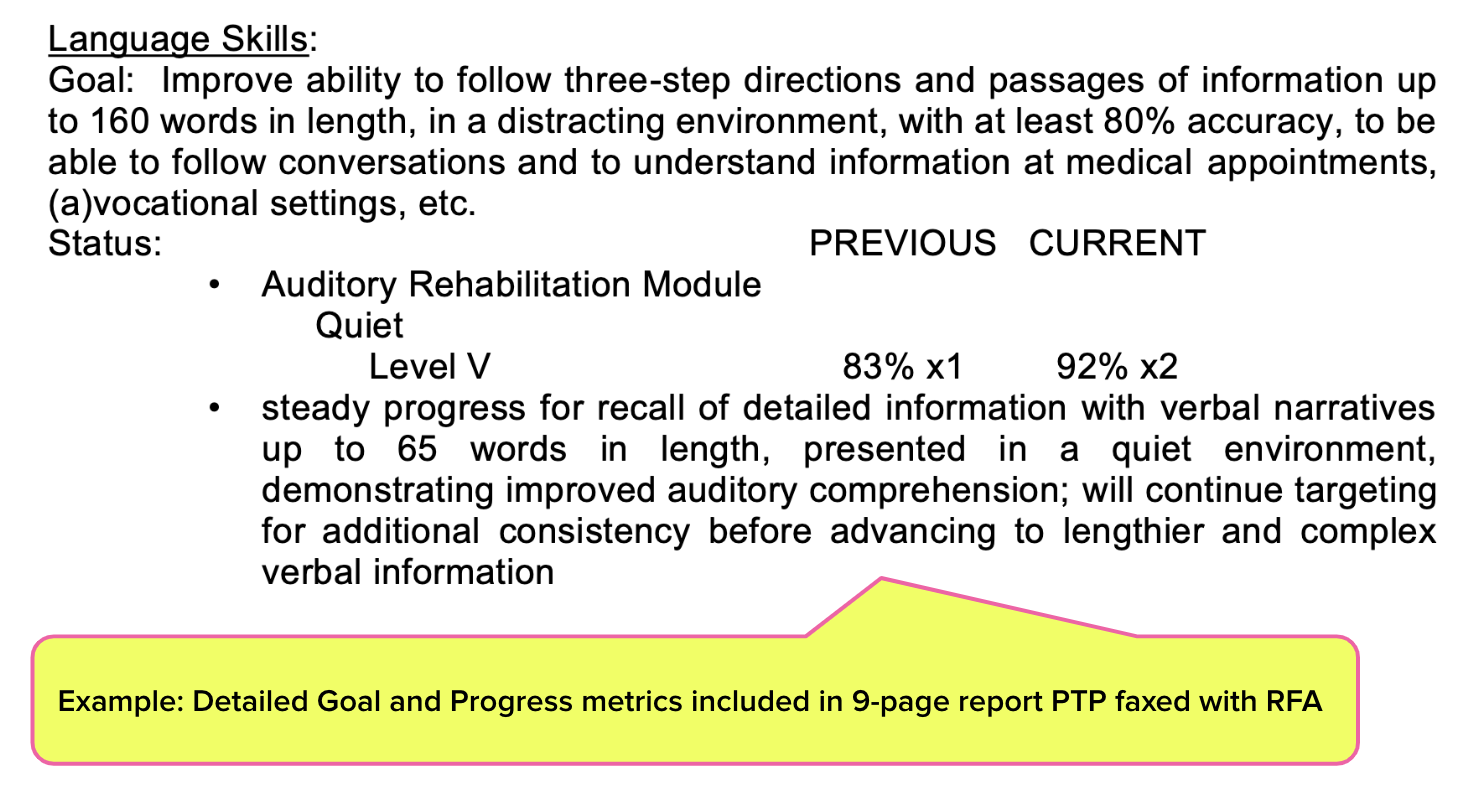
The report also included seven pages of detailed quantitative progress and goals. A sample from the report is shown below.
For each of the following areas of concern, the report offered detailed quantitative progress and goals demonstrating that the injured worker’s cognitive skills were improving with the treatment:
- Cognitive/Communication Skills
- Mobility Skills
- Basic and Instrumental Self-Care Skills
- Psychosocial Intervention
EK Health Denies for Missing Documentation
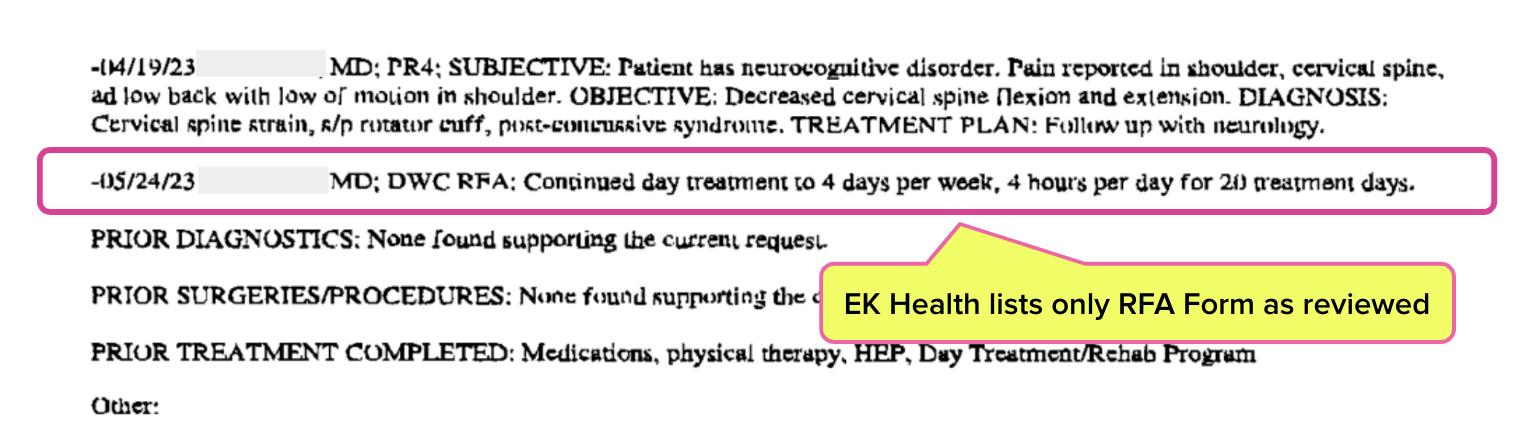
In response to the RFA for continued therapy, the doctor received an 11-page UR decision from EK Health, which included the statement:
“Without an updated medical report on the patient’s progress and goals, continued approval for the program does not appear appropriate.”
EK Health’s UR decision also noted the documents that EK Health reviewed. As shown below, the only document listed is the DWC RFA form. The EK Health UR decision did not list the doctor's detailed medical report faxed to SCIF with the RFA.
In other words, EK Health failed to acknowledge receipt of the detailed 9-page medical report shown above — even though SCIF 100% verifiably received that report.
RFA Fax Receipts Don’t Lie
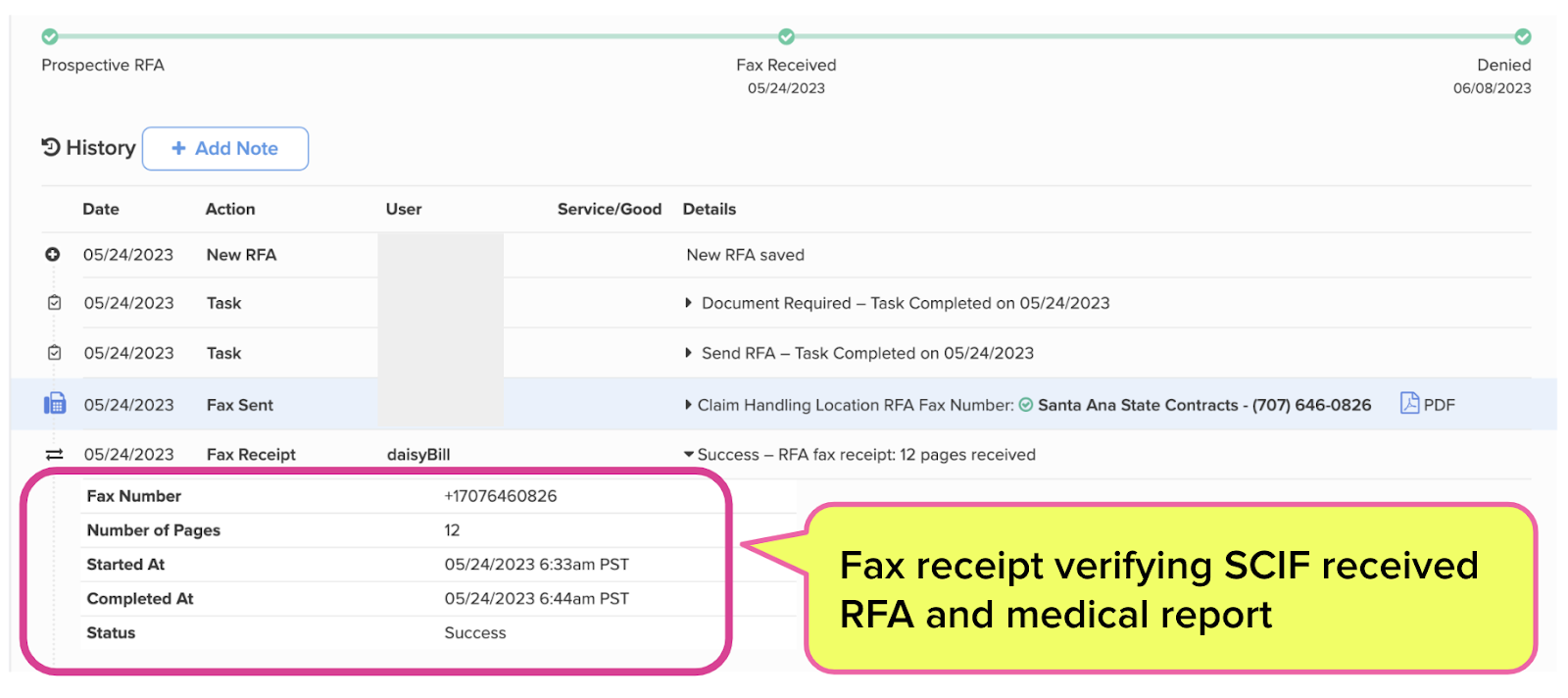
The doctor undoubtedly sent the 9-page medical report with the RFA, and SCIF indeed received the report; daisyAuth records every document sent and received with each RFA.
The screenshot below shows that SCIF received all 12 pages of the RFA submission, including the report detailing the injured worker’s progress and goals, at 6:44 AM on May 24.
What Happens Next?
As we asked in our prior article, what now?
According to California Code of Regulations Section 9792.9.1, denial of treatment stands for 365 days. By mishandling the documentation the physician faxed with the RFA, SCIF is relieved of any obligation to pay for medically necessary therapy — per the treating doctor’s recommendation — for at least a year.
As for recourse, many would direct the injured worker to file for IMR to dispute the denial.
However, DWC has established IMR rules that likely preclude this injured worker from any recourse, including IMR. In a future article, we’ll explore how this injured worker is unlikely to prevail in an IMR dispute, almost guaranteeing SCIF is off the financial hook for paying for medically necessary care.
For the injured worker, the following year will be long and difficult. For SCIF and EK Health, it appears to us like business as usual.
Authorization is the first hurdle in the workers’ comp obstacle course. Enjoy 30-second RFA submission and automatically tracked UR decisions with daisyAuth — request a demo below!
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.



.gif)


.gif)
I get a million denials based on missing documentation (that was in fact sent) from Genex. I just went through the IMR process on one of these, where MTUS guidelines make clear the patient should be provided at least 20 CBT sessions for the diagnosis involved. I faxed all session documents, the last one of which was titled "CBT session 9" with notation in bold that 10 sessions had been authorized to date. The result of the IMR? The IMR upheld the Genex denial because 1) it was not clear when the patient was first seen with this office (even though they had all the records); and 2) it was not clear to the reader how many CBT sessions were provided to date even though reader acknowledges this was "CBT session 9". For all doctors submitting IMRs, you need to be sure to include these items in your documentation - but they will find another ridiculous way to deny it, anyway. Meanwhile, patient is denied treatment (and forced to be released from care) despite MTUS guidelines so clear that a UR wasn't even really necessary.