The Hartford Goose Chase Ends - "Hartless" Pays Up
In a previous article, we detailed the burdensome (and unwarranted) process required for a provider to determine the reason The Hartford inexplicably failed to reimburse a QME for a Supplemental Medical-Legal evaluation properly. Mysteriously, The Hartford sent a check to the provider for less than the amount indicated on The Hartford’s Explanation of Review (EOR).
Last week, The Hartford finally paid the provider every cent owed for the bill in question and additional reimbursements for other bills that The Hartford had previously underpaid.
In theory, it’s a happy ending. But in reality, The Hartford inflicted administrative payment abuse on this provider.
In theory, The Hartford should face regulatory repercussions for its provider abuse. But in reality, California regulators allow this rampant payment friction by failing to impose substantive penalties on claims administrators who send providers on goose chases to receive payment.
It is indefensible—or as the provider put it, “Hartless”— for claims administrators to make treating injured workers this torturous.
The Hartford Demands Already-Submitted Documents
Upon receipt of the check, daisyCollect undertook an extended collections odyssey to determine the reason for the mysterious underpayment. It took multiple phone calls and emails, undue aggravation, and several weeks of a precious and finite life. Eventually, a Hartford representative explained that the missing funds were a “backup withholding” due to a missing W-9 tax form.
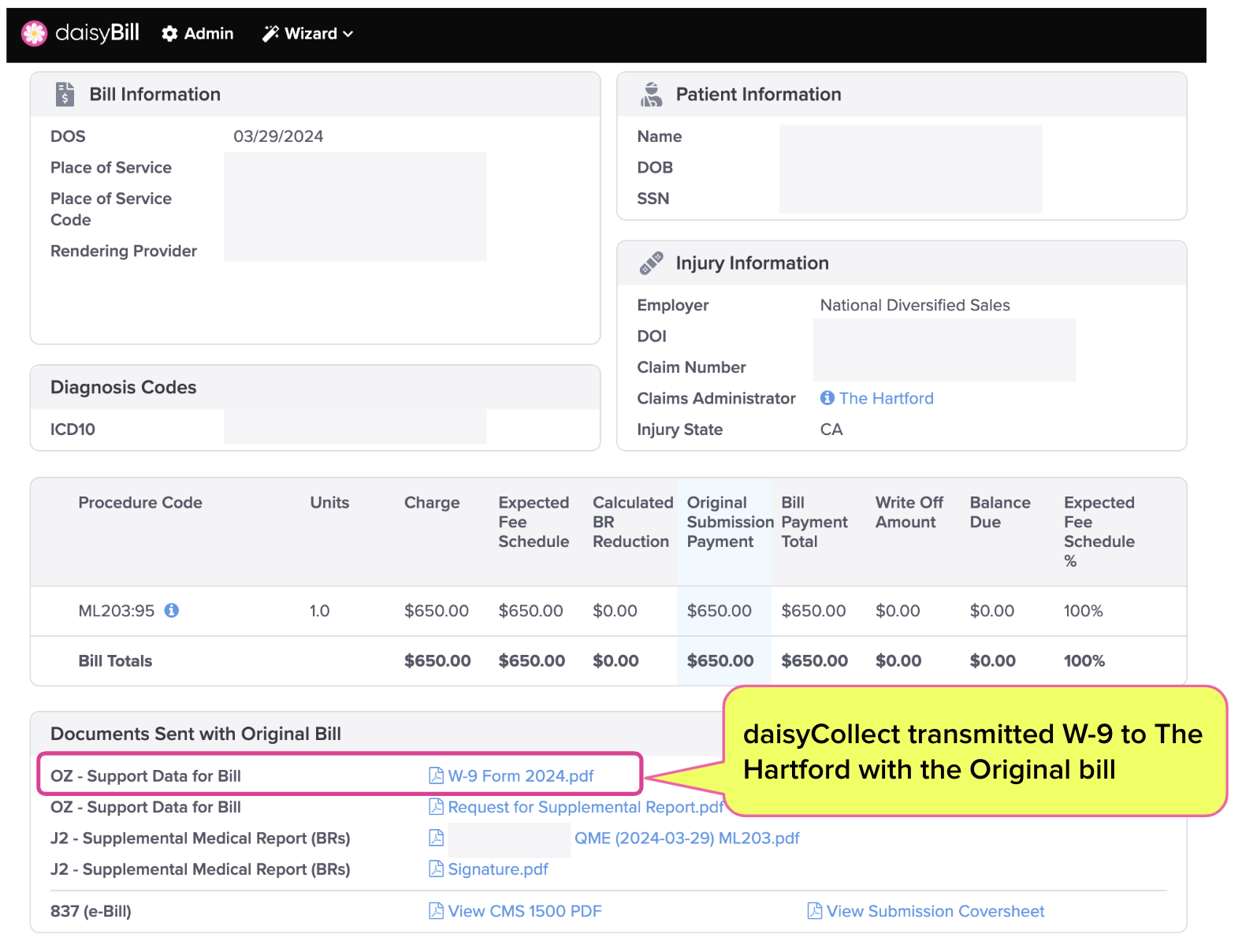
However (and of course), The Hartford’s excuse for the underpayments was goose poop, because daisyCollect sent the required W-9 with the original bill submission, as documented in the screenshot below.
The Hartford Payment Goose Chase Ends
Despite submitting the W-9 with the original bill, The Hartford representative required daisyCollect to send a second W-9. The Hartford subsequently sent the additional payment and payments for several older bills the provider submitted before becoming a daisyCollect client.
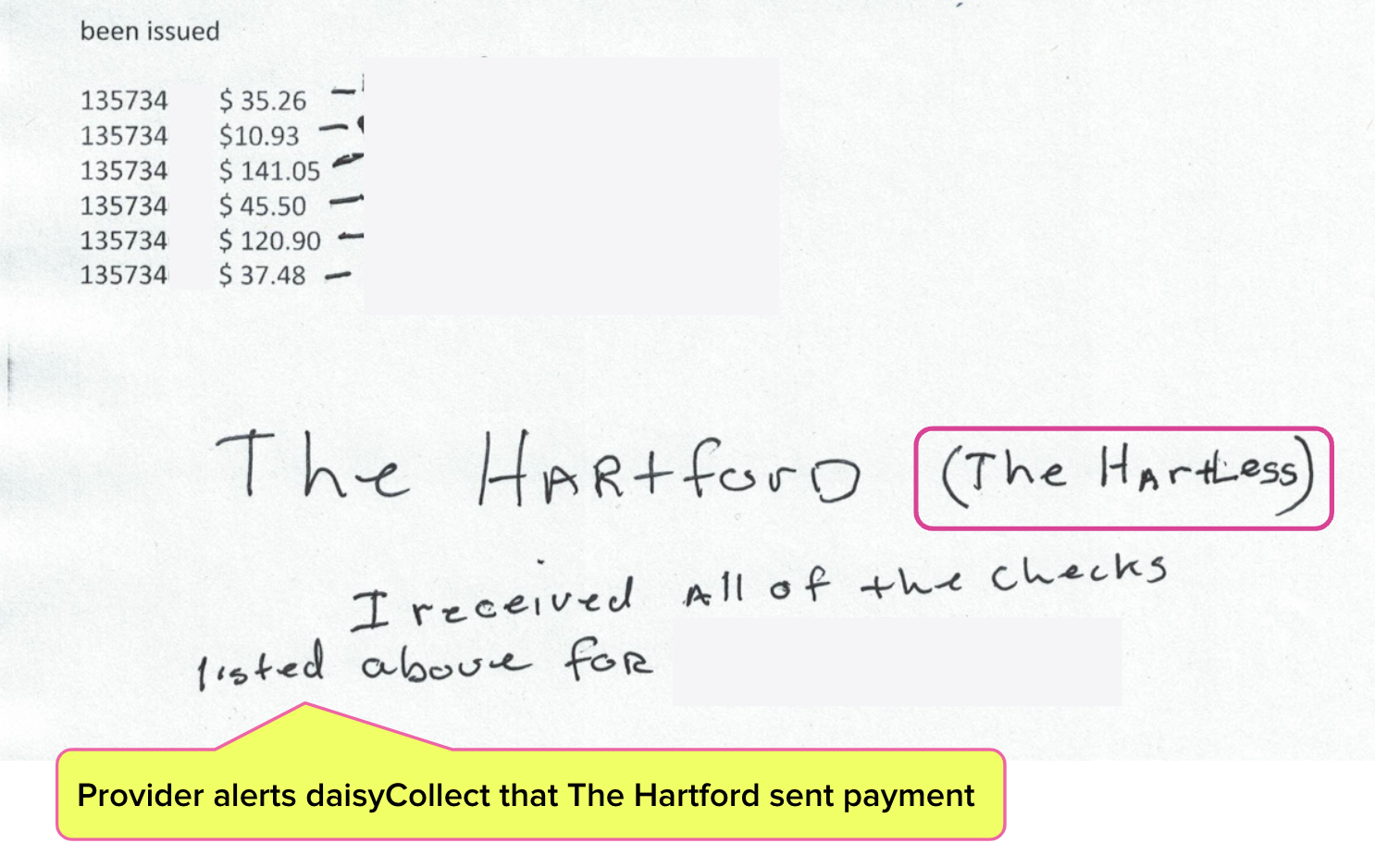
In all, The Hartford remitted $391.12 in additional reimbursement owed—funds the provider would not have recovered if not for daisyCollect agents’ willingness to push through The Hartford’s mountain of red tape and erroneous claims of lacking documentation.
In a note to daisyCollect, the provider confirmed receipt of the additional payments…and offered a new nickname for the exasperating insurer.
Expecting claims administrators to operate efficiently, competently, and in good faith is not unreasonable. A minimum performance standard by insurers, self-insured employers, and Third-Party Administrators is vital to keeping doctors in the system and getting injured workers the care they need.
Again, we’re happy to have gotten our client paid. But too often, providers are forced to bear the consequences of claims administrators’ (highly profitable) inefficiency and non-compliance.
California regulators abandon providers and injured workers by failing to incentivize efficiency and deter shoddy performance by claims administrators. Providers can only bear so much for so long before deciding workers’ compensation isn’t worth the administrative (or mental) hassle.
Let the experts handle your workers’ comp billing. daisyCollect professionals use advanced software (and years of experience) to protect your practice. Learn more and request a demo below:
LEARN MORE
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.gif)
In my 25 years as a defense attorney, I cannot possibly number the times that I have received a proof of service from another party that lists items that are not actually included with the served documents. Is it possible the W9 was not attached and would it be unreasonable for The Hartford to request another copy in order to ensure proper payment? And if providers are considering abandoning the workers' compensation system due to administrative hassles, I with them luck in avoiding the exact same hassles when dealing with Medicare, Medicai, HMOs and PPOs outside of the workers' compensation system. Unless a provider is planning on working on a cash only basis, they will end up dealing with many of the same "hassles" and far to often I see the providers failure to provide the proper and required documentation, language and supporting documents and that is typically the basis of their failure to secure the payment they are requesting as quickly as they would like. Despite the providers failure to provide required documentation, I've still heard them complain that the system is too difficult. In the end, many of the doctor providers are apparently of the impression that their medical opinion regarding required services and the payment they deserve for such services are not to be questioned. In this case, it mentions that the provider was a QME. If so, I am very sensitive to timely payment as per the ML fee schedule and advise my clients to pay quickly and in accordance with that schedule so that they can avoid them pursuing legal services and then requesting additional reimbursement for legal fees.