CA DWC Website Deletions Enrich Claims Administrators
Given the complexity of workers’ comp (and the myriad ways claims administrators improperly deny requests for treatment and payment), knowledge is a precious resource for providers.
For example, California's Utilization Review (UR) process is extremely convoluted, with more twists and turns than an M. Night Shyamalan movie. As a reminder, state law requires employers to pay two doctors to do the job of one:
- A treating physician to recommend the care necessary to heal the injured worker, and
- A Utilization Review physician to ration and restrict the care the treating physician recommends.
Since getting treatment approved is such a fraught process, the Division of Workers’ Compensation (DWC) publishes a webpage for “Frequently Asked Questions” about UR. However, as we’ve reported in recent articles, the DWC has quietly deleted critical information from this page.
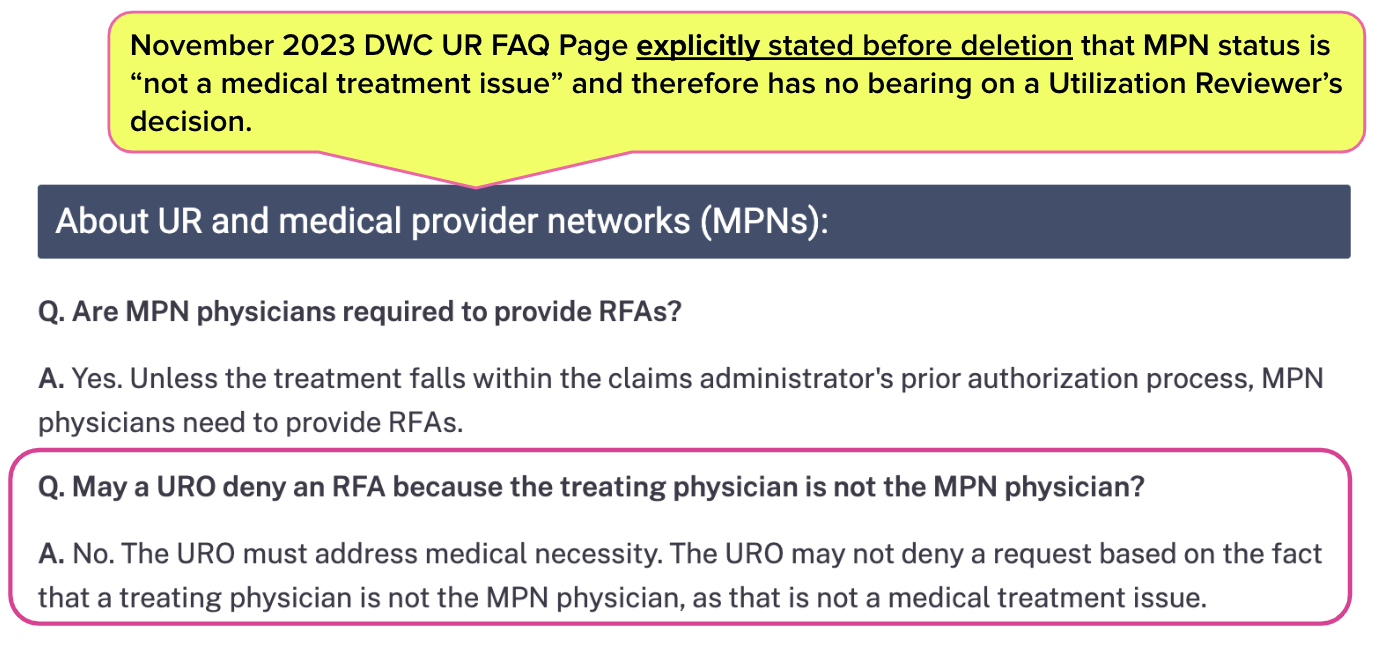
The latest vanishing FAQ explained that a Utilization Review Organization (URO) may not deny requested care by citing the requesting physician's non-participation in a Medical Provider Network (MPN).
This critical fact is no longer mentioned on the FAQ page. In fact, the current page no longer offers any instructions regarding UR obligations when the requesting physician is not in the applicable MPN. The deletion raises a Question that advocates for providers and injured workers are Asking more Frequently: Why?
Below, we offer a troubling potential answer, supported by a recent article on Managed Care Matters reporting that workers’ comp is “hugely profitable.” We must ask who profits from keeping providers in the dark, which hinders injured workers’ recovery.
Utilization Review Explained
Essentially, a physician in California cannot treat an injured worker without permission from the claims administrator.
California law requires the physician to submit a Request for Authorization (RFA) to the claims administrator for all proposed care. Upon receipt of the RFA, the claims administrator must conduct UR to determine whether the care recommended by the treating physician is medically necessary.
Or, as the DWC UR FAQ page used to state before its extreme makeover (emphasis ours):
“UR is the process used by employers or claims administrators to determine if a proposed treatment requested for an injured worker is medically necessary.”
To determine whether recommended treatment is medically necessary, claims administrators engage or operate Utilization Review Organizations (UROs). California employers pay for these UROs to review the millions of RFAs physicians send as they attempt to heal injured workers.
DWC Drops Critical UR/MPN Question
The Internet Archive’s Wayback Machine lets anyone view previous versions of various web pages, including the DWC UR FAQ page.
While the DWC may believe it can scrub essential knowledge from the site unnoticed, the Wayback Machine shows a deleted FAQ published as recently as November 2023 (shown below). This deleted FAQ instructed that UROs may not consider the provider’s inclusion in an MPN when determining whether requested treatment is medically necessary.
Unfortunately (for employers and injured workers), UR in California seemingly operates with zero regulatory oversight—as does the unregulated, abjectly broken, and corrupted MPN system.
By deleting critical FAQs, the DWC makes it even more challenging for treating physicians to care for injured workers, which delays these employees’ return to work.
DWC Opacity Profits Claims Administrators
Delaying injured workers’ return to work arguably—in the most cynical of bottom-line calculations—increases claims administrators' profits. The ugly, unspoken fact is that each untreated injured worker is a potential annuity for claims administrators; the longer an injured worker requires treatment, the more profit claims administrators can reap from:
- Additional bill review fees,
- More URO fees, and
- Endless PPO “savings”
Who benefits from shutting down access to information that facilitates speedier, less costly recovery for injured workers? Who is the beneficiary of these wild profits?
California regulators' decision to delete essential UR information adds another layer of opacity, which should be troubling to employers. When a state agency takes action that results in stakeholders being less informed of their rights, the outcome is rarely benign.
In California, a decrease in publicly available knowledge is a gift to claims administrators. It is surely not a gift to employers or their injured employees.
Submit RFAs in 30 seconds and automatically track UR decisions with daisyAuth. Schedule a demo below!
SCHEDULE DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.gif)
