DWC Removes Critical Info From FAQ Page
.gif)
For all the ways California providers can be denied reimbursement for treating injured workers, the state offers one solid protection: a simple (if poorly enforced) legal principle: authorization is a guarantee of payment.
This principle is not ambiguous, controversial, or debatable. It remains true regardless of questions around liability, compensability, Medical Provider Network (MPN) status, or anything else short of outright fraud.
Until as recently as December 2023, the Division of Workers’ Compensation (DWC) affirmed this principle on its FAQ page, stating that once authorized treatment is rendered, payment is due regardless of any dispute (and explicitly citing the example of MPN non-participation).
This is valuable, critical information that providers need to defend their practices from all kinds of improper payment denials. daisyNews has published screenshots of this FAQ in countless articles to remind providers of their rights (and to remind claims administrators of their obligations).
But recently, the DWC removed this FAQ from its website.
The legal promise of authorization doesn’t change because the DWC removes it from their web page. The agency can change the FAQ, but not the facts.
DWC: Deleting Providers’ Rights
The DWC’s consistent failure to uphold providers’ rights and enforce claims administrators’ legal requirements is bad enough.
But for the DWC to delete an FAQ about one of the bedrock protections for providers — however loosely enforced — surely doesn’t help to preserve whatever modicum of faith providers have in the agency.
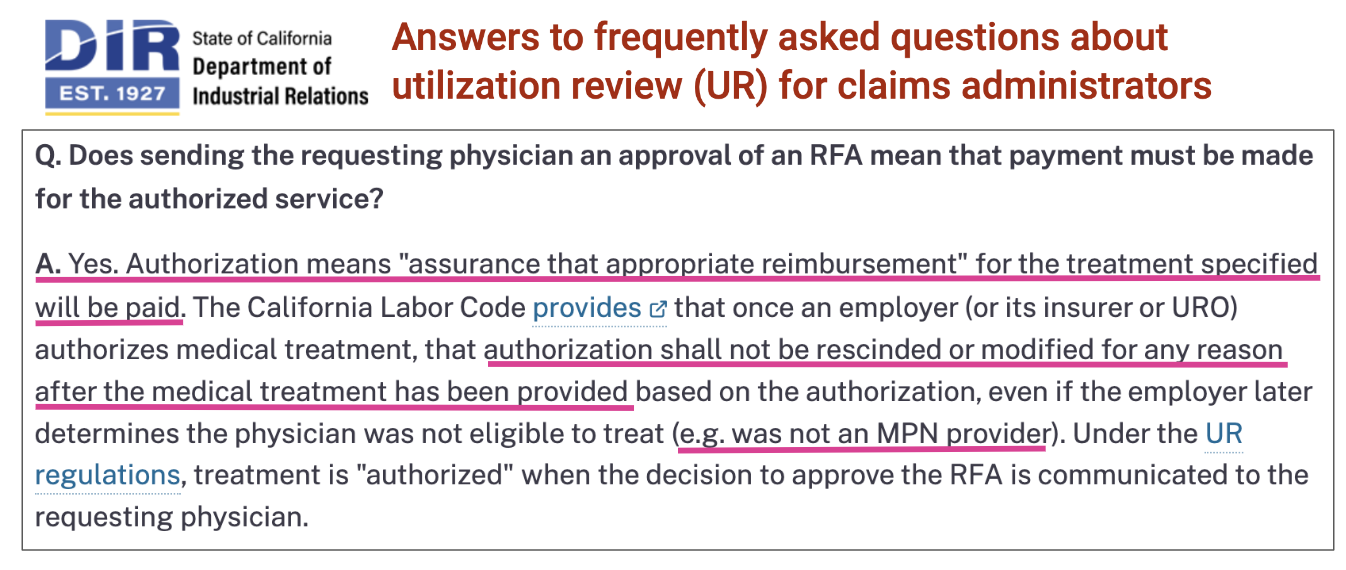
Below is the section of the DWC FAQ page that is now conspicuously absent (Relevant phrases are highlighted by our pink underlines).
This now-deleted FAQ illustrates two concepts that (when enforced) have inestimable value for providers:
- Authorization is a guarantee of payment for authorized services
- Authorization is final and irreversible once the treatment is rendered
Sadly, but not surprisingly, the DWC fails to address these two essential concepts in its new FAQ webpage.
More Than Just an FAQ
The prior FAQ was based on long-standing California law and the DWC’s own regulations. California Labor Code Section 4610.3 states:
...an employer that authorizes medical treatment shall not rescind or modify that authorization after the medical treatment has been provided based on that authorization for any reason…
California Code of Regulations Section 9792.6 states:
“Authorization” means assurance that appropriate reimbursement will be made for an approved specific course of proposed medical treatment to cure or relieve the effects of the industrial injury pursuant to section 4600 of the Labor Code…
These authorization and payment concepts are particularly important as concerns MPNs. The DWC has failed to furnish doctors with the necessary technology to determine whether an injured worker’s care is limited by an MPN. Accordingly, authorization plays a critical role in an injured worker's access to treatment.
For all the chaos, confusion, and impropriety engendered by the failed MPN system, guaranteeing that authorization equals payment is one of the few protections providers have.
Unfortunately, claims administrators routinely deny payment for authorized services rendered based on claims (factual or otherwise) of MPN non-participation. Without this now-deleted FAQ knowledge, how can California providers fight blatantly improper, often MPN-based payment denials that contravene the law and regulations?
More importantly, why would the DWC take action that makes this knowledge less accessible to providers?
We are at a loss as to what purpose this DWC decision could serve, but we are not at a loss as to who benefits: payers. To keep providers in the dark and render them even more vulnerable to payment abuse is yet another way this agency fails to carry out its role.
We make treating injured workers easier, faster, and less costly. Request a free demonstration below.
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.
.gif)
.gif)


"The agency can change the FAQ, but not the facts."-- hello 9-1-1, I would like to report a murder
I have to agree with the DWC on this one on removing the language. Authorization is NOT a guarantee of payment. Authorization means that the service is medically necessary. The URs job is to determine MEDICAL necessity. That is all. If the patient's case was denied because he caught on vacation chopping wood (true story), then the treatment shouldn't be paid even if there is an authorization. The language needs to be amended to be more specific and pertaining to admitted/accepted cases only where MPN isn't an issue. Denied claims are a different ballgame as we all already know.