CA Farce Alert: $300K to Study Nonexistent UR Data

The California Division of Industrial Relations (DIR) has outdone itself in bureaucratic absurdity—proposing to spend $300,000 on a study without any data to study.
In a Request for Proposal (RFP) (S24DWC018), the DIR claims to seek a “deep, thorough, and detailed analysis” of how Utilization Review (UR) impacts medical treatment in the first 30 days after a workers’ compensation claim is filed.
The problem with this RFP? The California DIR’s Division of Workers’ Compensation (CA DWC) has no UR data to analyze. Why? Because the agency has ignored state laws requiring them to collect it.
The CA DWC has ignored Labor Code § 4610(o), which mandates the CA DWC “develop a system for the mandatory electronic reporting of documents related to every utilization review performed by each employer.”
Additionally, the DWC has ignored Labor Code § 138.8, enacted in 2019, which requires the DWC to publicly disclose data on how often claims administrators deny or modify treatment requests from individual doctors. Those UR data—meant to be posted by January 1, 2024—remain conspicuously absent.
So, what UR data will the RFP contractor “deeply and thoroughly” analyze? The RFP suggests reviewing the Workers’ Compensation Information System (WCIS) and Electronic Adjudication Management System (EAMS), which notably do not include UR approval, modification, or denial data.
In short, the CA DIR wants to spend hundreds of thousands of taxpayer dollars on a study of an empty dataset.
Even more baffling is the RFP’s focus on so-called “automatic” treatment authorizations—an illusion in California workers’ compensation law. While Labor Code § 4610(b) theoretically allows doctors to bypass UR and provide treatment within the first 30 days post-injury, this supposed “automatic” authorization is functionally nonexistent.
Below, we explain why this RFP is (yet another) CA DIR and DWC wasteful farce.
The “Automatic” Authorization Myth
One preposterous aspect of the proposed RFP is that it requests an analysis of “automatic” treatment authorizations. Per California Labor Code § 4610(b), "automatic" authorization allows physicians to bypass the UR process so that physicians can deliver treatment rapidly in the first 30 days post-injury.
However, so-called “automatic” authorization is effectively useless due to two insurmountable conditions:
- Liability Acceptance: The claims administrator must accept liability for the specific body part or condition.
- MPN Physician: Only physicians within the employer's Medical Provider Network (MPN) or predesignated by the injured worker are eligible.
Treating doctors have no way of knowing whether a claims administrator has accepted liability for the injured worker's claim during the first 30 days of an injury. In fact, California Code of Regulations § 9812 allows a claims administrator up to 90 days (not 30 days) to decide liability.
Even worse (unbelievably), as daisyNews has thoroughly documented, the California DWC has created an MPN system where it is impossible for a doctor to determine which MPN applies to an injured worker or whether the doctor is listed in the applicable MPN. No mechanism exists to verify this condition of “automatic” authorization.
Without a way to confirm an injury’s liability status or MPN eligibility, so-called “automatic” authorization” is nothing more than a bureaucratic ruse conjured by the CA DIR and DWC.
Given these glaring contradictions, taxpayers and stakeholders should demand to know exactly what a $300,000 “study” will reveal about medical care in the first 30 days of an injury.
DIR’s Outrageous Claim: “No Significant Delays or Denials”
The most insulting part of this RFP might be the DIR’s assertion that “existing research does not support the argument of significant delays or denials due to UR.”
What research? There is none. The DWC’s refusal to collect UR data ensures that no one—not doctors, injured workers, employers, or even legislators—can quantify how often claims administrators manipulate UR to delay or deny treatment.
As demonstrated by daisyNews, claims administrators and other payer-side entities have their internal (self-serving) numbers.
For reference, Sedgwick, a Third Party Administrator, advertised on its website that it denied 54% of treatment requests while publicly boasting about delivering a 5-to-1 return on investment for employers. Sedgwick removed these statistics from its public website after we drew attention to their disgraceful denial percentage.
Will the winning contractor have access to Sedgwick and other entities’ internal UR data?
Even if they did, such numbers will, of necessity, be self-reported—and, in all likelihood, lack external oversight. Without a state-mandated UR tracking system, Sedgwick and other entities can presumably hide these denials behind layers of administrative obfuscation.
DIR RFP – Deep Misunderstanding or Intentional Disinformation?
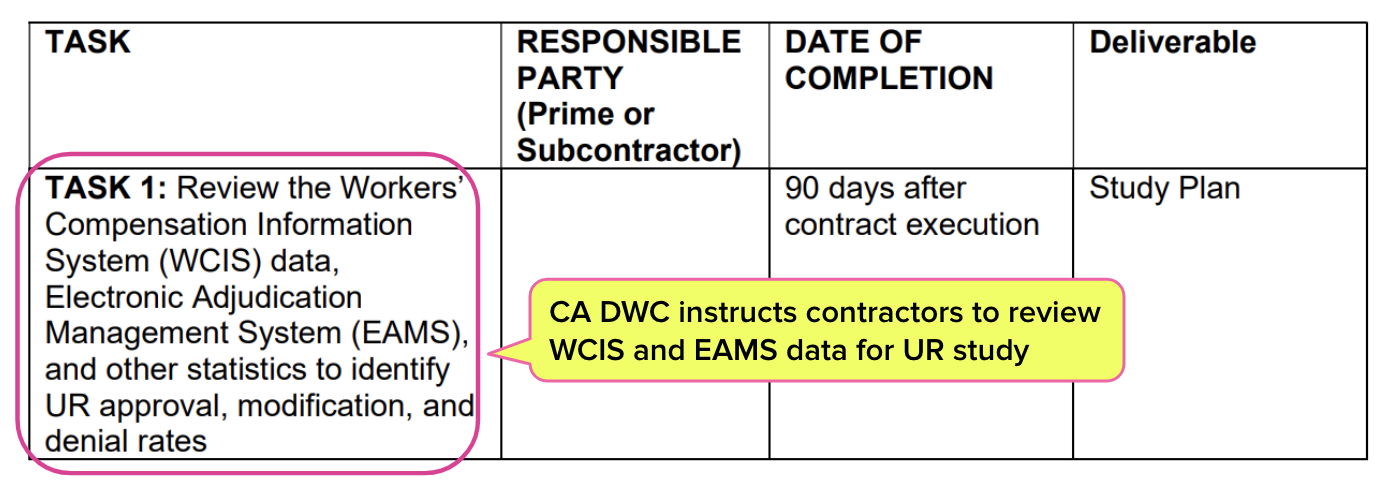
The RFP instructions (available here by clicking ‘View Event Package’) on page 17 specifically instruct potential contractors to “Review the Workers’ Compensation Information System (WCIS) data, Electronic Adjudication Management System (EAMS) data, and other statistics to identify UR approval, modification, and denial rates.”
An important fact: WCIS and EAMS data do not (not!) include UR approval, modification, or denial information. Moreover, reporting to WCIS is “voluntary” for claims administrators, according to CA DWC instructions.
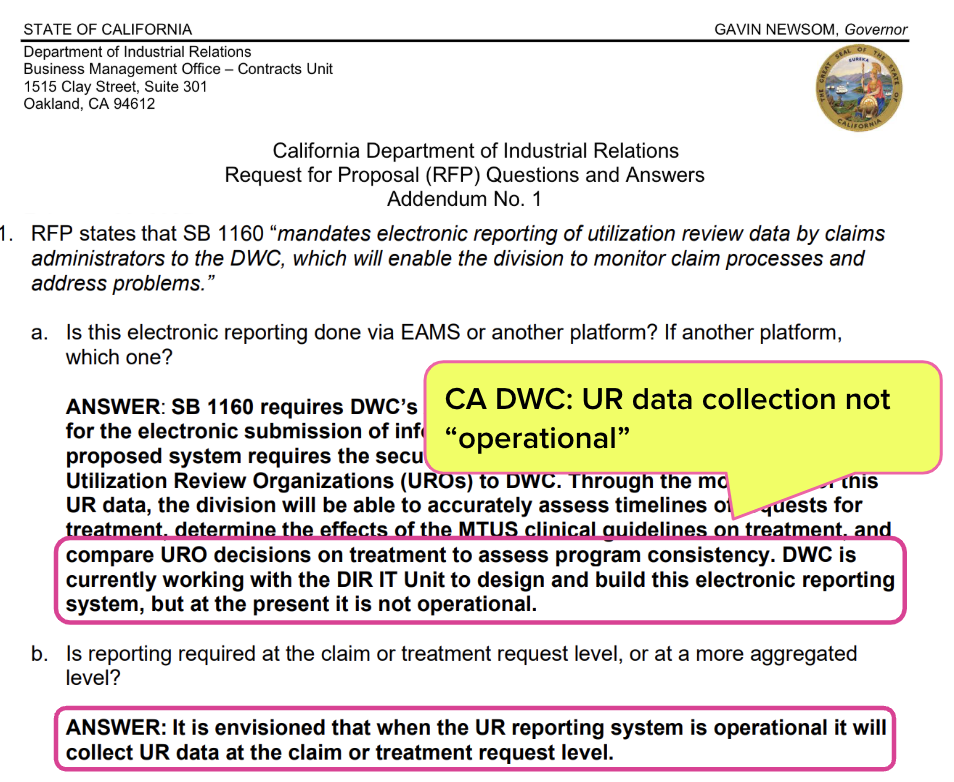
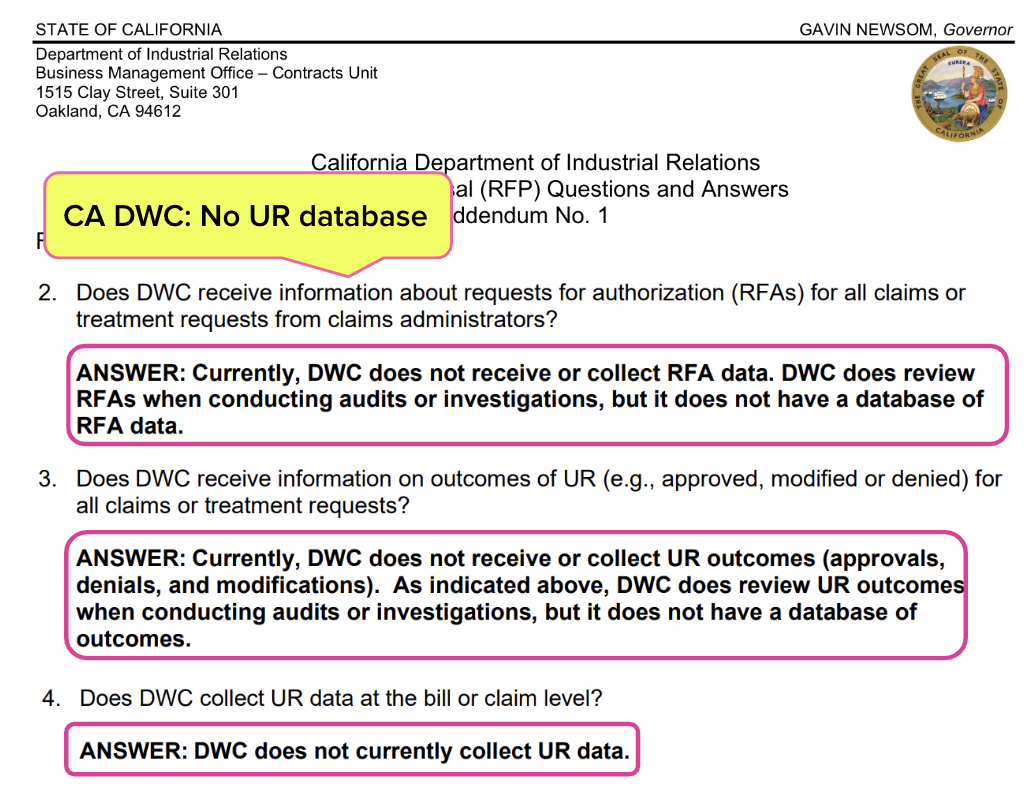
The most important fact: The RFP acknowledges that the DWC lacks UR data sources. In its Q&A-style addendum to the RFP instructions (screenshots below), the DIR repeatedly acknowledges there are zero UR data to study.
A Study Designed to Shield Claims Administrators
It’s hard not to suspect that the real purpose behind this $300,000 study is to obscure California’s UR failures while protecting claims administrators from scrutiny.
By failing to collect the necessary UR data, the DIR ensures that any contractor hired for this study cannot reach meaningful conclusions. Instead, the “findings” will be nothing more than speculation—findings that we suspect will merely uphold the status quo.
The RFP’s directive for contractors to “identify UR approval, modification, and denial rates” without providing the data needed to do so is a blatant red flag. How can a contractor analyze data that don’t exist? What else can they do besides guess—while collecting $300,000 for the effort?
It’s fair to question whether any report produced from this study will be built on anything more than fiction, speculation, and guesswork—allowing the CA DIR and DWC to pretend they are addressing systemic issues while continuing to ignore the transparency laws it is their duty to enforce.
A Simple Solution: Adhere to the CA Law
California’s UR system is fundamentally broken, but throwing taxpayer money at a contractor to conduct a data-free study will do nothing to fix it.
The real solution is obvious: the CA DWC must comply with existing law and collect the required UR data before considering any study.
Instead of a sham investigation designed to placate stakeholders while protecting claims administrators, the CA DWC should:
- Implement the mandatory electronic UR reporting system required under Labor Code § 4610(o).
- Adhere to Labor Code §138.8 requirements to publish provider-level UR data.
- Then—and only then—consider funding a study based on actual data, not fiction.
Until then, this RFP remains nothing more than a taxpayer-funded charade—a study that will probably (and conveniently) guarantee no real accountability ever reaches the claims administrators that will continue to profit off California employers’ workers' comp premiums while delaying and denying care to injured workers.
Submit RFAs in 30 seconds and automatically track UR decisions with daisyAuth. Request a demo below!
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.
.png)



Couldn't it be that the RFP Study would include the collection of the data? I've see plenty of studies and data reported on this. Your own blog reported 71% approval and 24 % denial. But, you did not follow that with IMR results. If the UR is upheld by IMR, well, there you have it. If the UR is overturned and done so frequently there is a problem. CWCI does studies which can be found on their website. They also point out that As in previous reviews, the latest data show that a small number of physicians continue to drive much of the IMR activity, with the top 1% of requesting physicians (80 doctors) accounting for 40.3% of the disputed service requests that underwent IMR in the 12 months ending on June 30 of this year. The top 10 individual physicians alone accounted for 11.6% of the disputed requests, and notably, 9 of the 10 individual providers with the highest number of IMR requests a year earlier were still on the top 10 list in the latest review. CWCI has much more data to analyze that you do. Consider that the problem may be with the doctors not following MTUS, which is mandated.
Bravo to daisyNews for once again exposing the malarkey that spews from the mouth of the DIR and the DWC -- as well as revealing the $300K spend to fund a "study" that will only profit the author(s) of that "study."
This just more of the SOS (Same Old S***)