Costco/Helmsman: Improper $5K Payment Denial
For California physicians, too much time, effort, and revenue are at stake to accept ludicrous payment denials for Medical-Legal evaluations.
Unfortunately, California law, in effect, incentivizes all claims administrators to improperly deny payment for services rendered to injured workers, including Medical-Legal evaluations.
Take the recent case of an Agreed Medical Evaluator (AME) who conducted a Medical-Legal evaluation for an injured Costco employee. The AME performed a comprehensive evaluation and reviewed over 1,000 pages of medical records to complete the 31-page evaluation report.
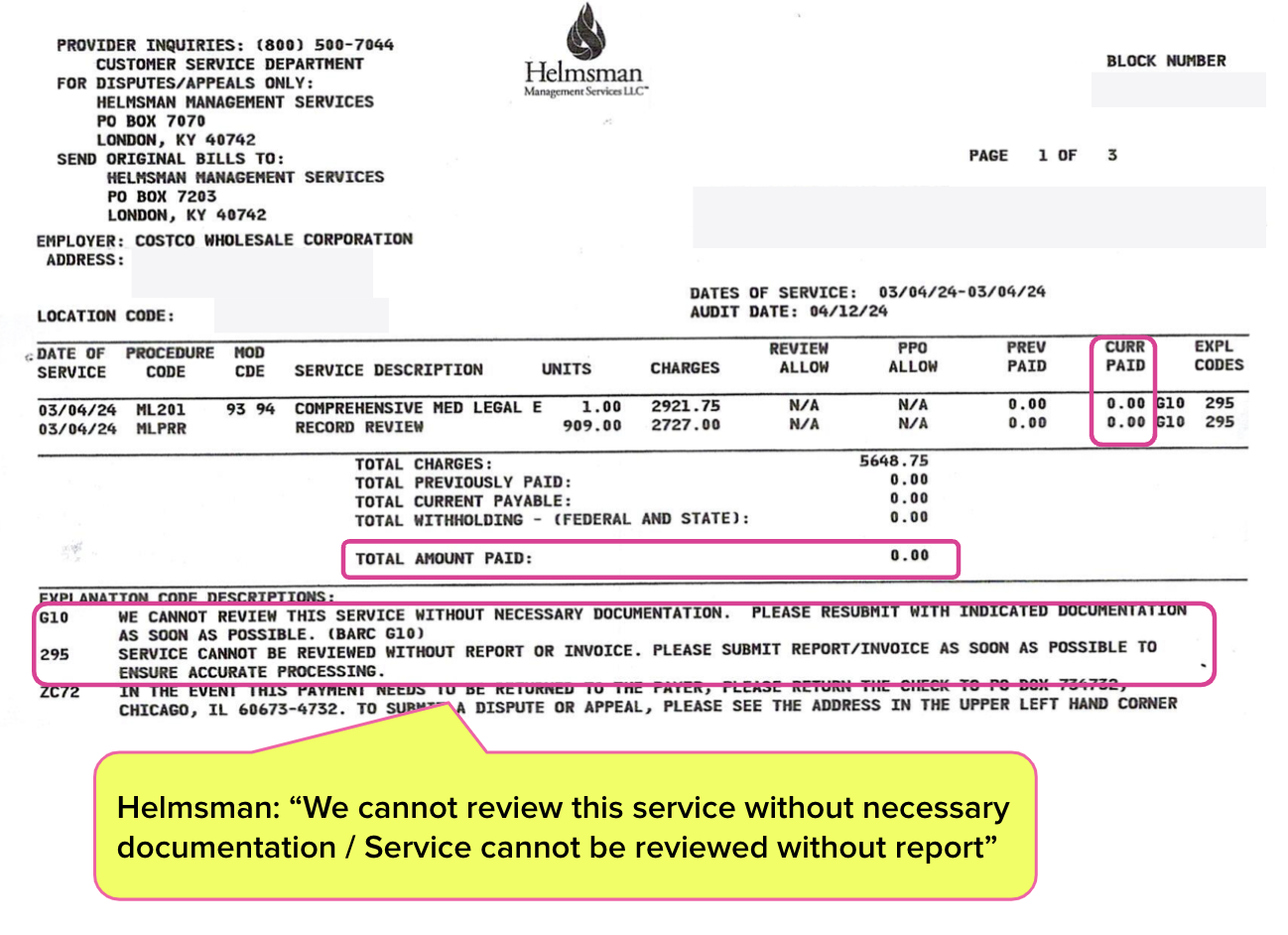
Helmsman Management Services LLC, Costco's Third-Party Administrator (TPA), denied payment for the AME’s $5,648 bill, citing demonstrably untrue denial reasons.
If this AME failed to submit the required Second Review appeal in a timely or compliant manner to dispute the improper payment denial, California law would allow Helmsman to retain the entire payment, and Helmsman would owe the AME exactly $0.
Fortunately, daisyCollect ensured a timely appeal—and this AME also took a stand. Below, see the letter the AME sent to the defense and applicant attorneys protesting Helmsman's payment abuse.
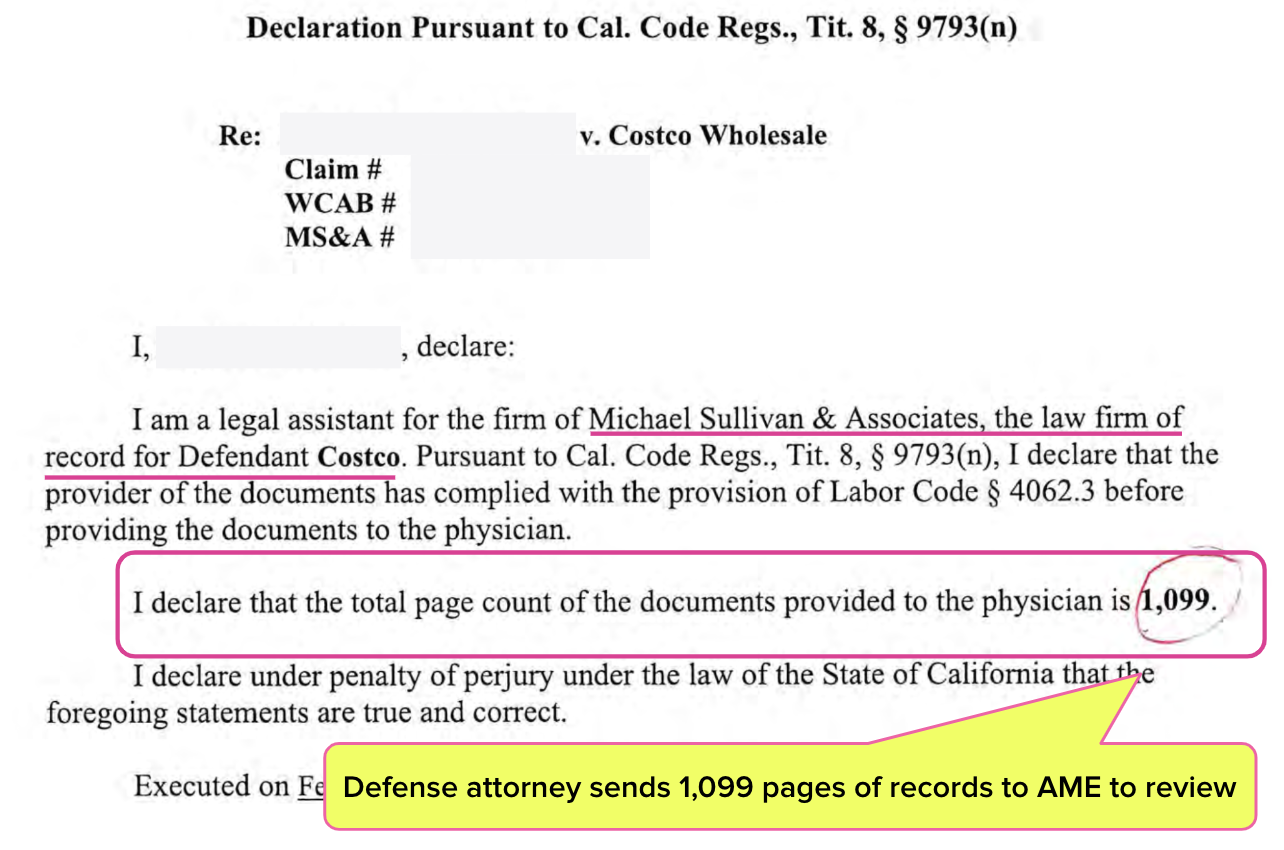
Defense Sends AME 1,099 Pages of Medical Records
Costco’s and the injured worker’s attorneys jointly requested that the AME perform a Comprehensive Medical-Legal Evaluation.
The injured worker’s applicant attorney submitted 10 pages of medical records for the AME to review. The defense attorney for Costco sent the evaluator 1,099 pages of records, as shown in the page count attestation (required by California Code of Regulations Section 9793) below.
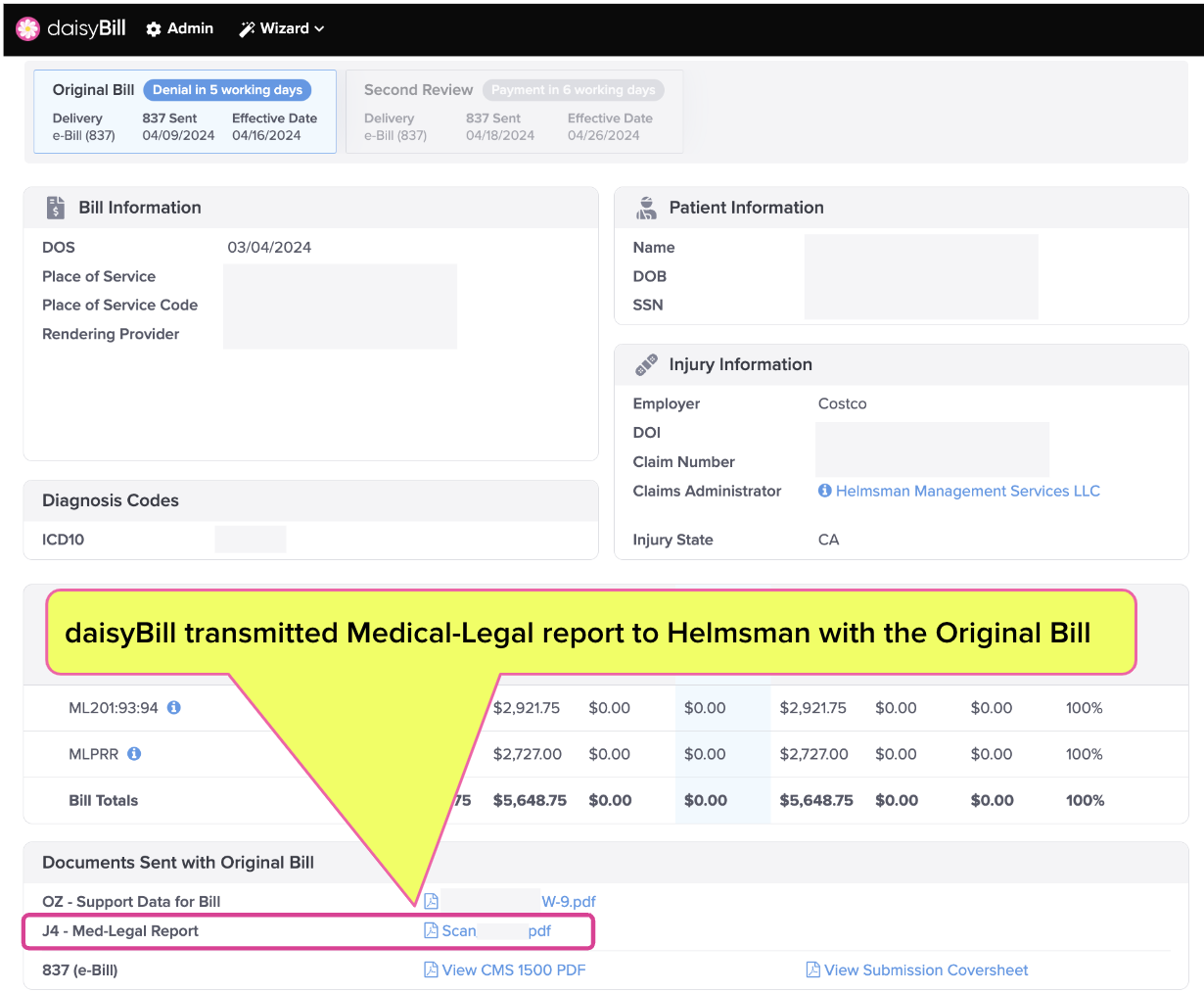
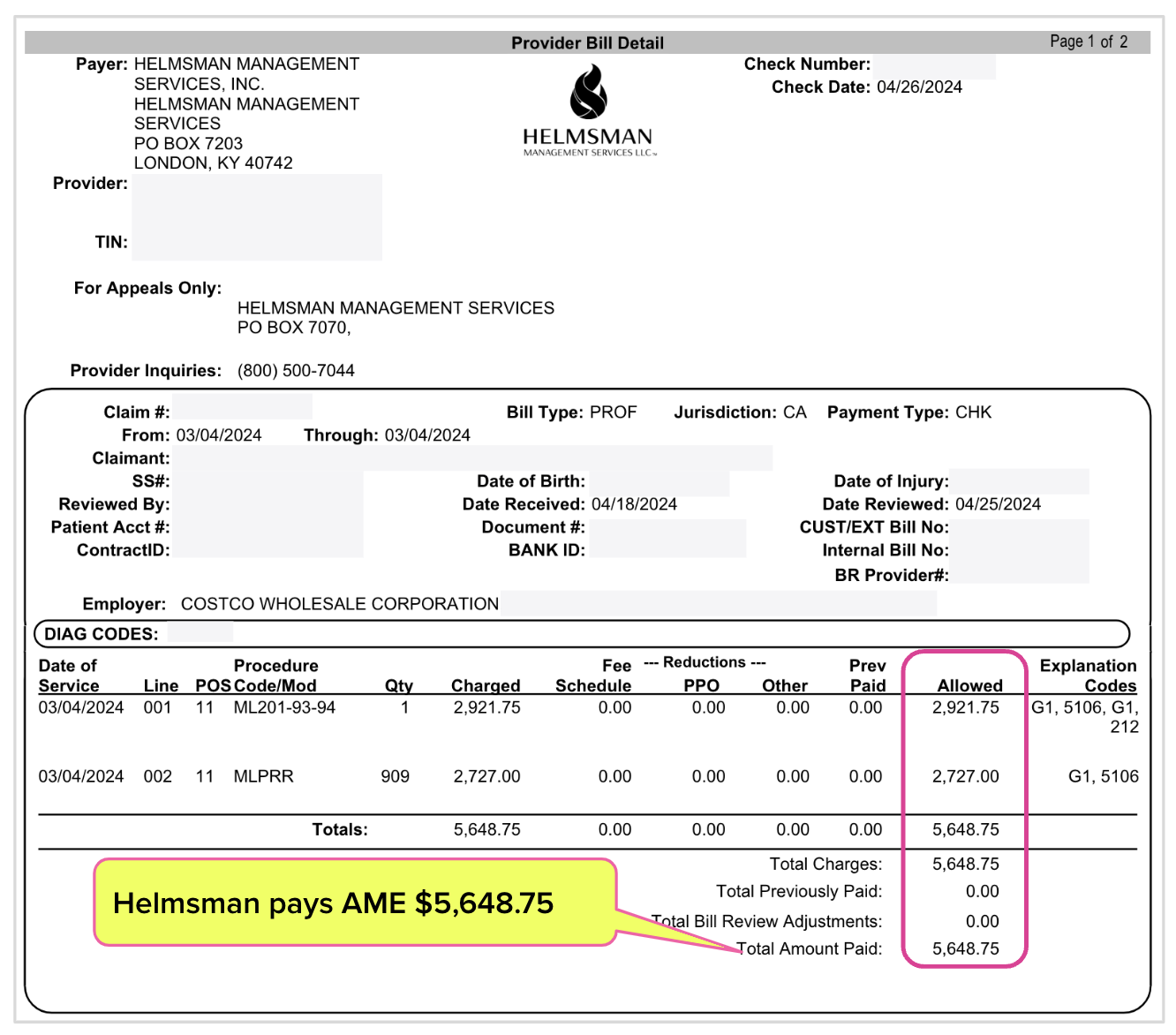
The bill for the Medical-Legal evaluation and record review totaled $5,648.75.
Helmsman Improperly Denies Payment
The screenshot from daisyBill below shows the AME’s bill was sent to Helmsman with the Medical-Legal evaluation report (and the evaluator’s W-9). Yet Helmsman denied payment for the bill, claiming they could not adjudicate the bill “without necessary documentation” or the “report/invoice”—a patently absurd excuse.
Second Review (and Indignant Letter) to the Rescue
In accordance with California law, daisyCollect promptly submitted a Second Review appeal disputing Helmsman’s blatantly improper denial. But that wasn’t the only communication sent.
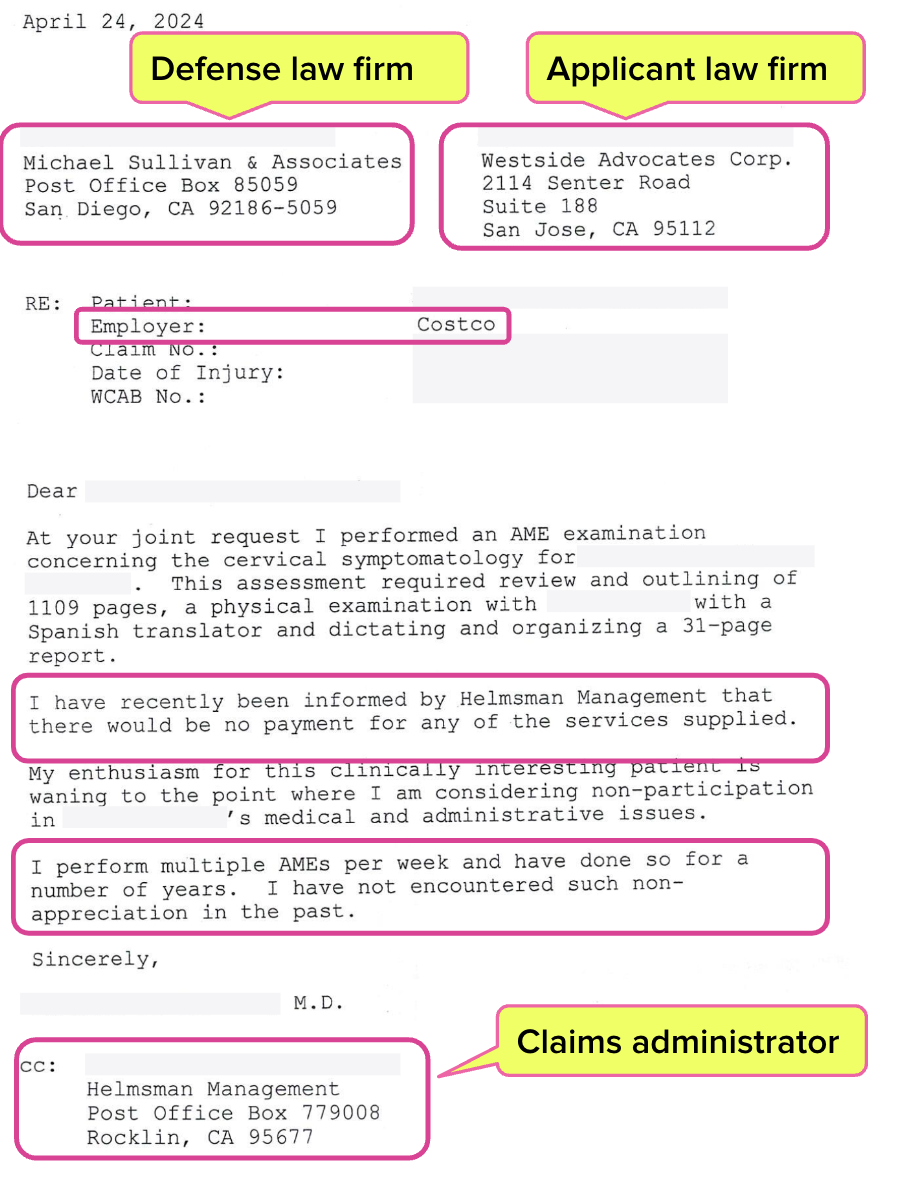
In a letter to the defense and applicant law firms (with Helmsman cc’d), the AME made his frustration clear (albeit in a restrained, entirely professional manner that’s impressive for someone being stiffed for nearly six grand) noting:
“I perform multiple AMEs per week and have done so for a number of years. I have not encountered such non-appreciation in the past.”
Helmsman Pays AME
We cannot know whether the Second Review appeal, the AME’s letter, or some combination brought Helmsman to its senses. We know only that there is little evidence of any will on the part of regulatory agencies to enforce penalties on any claims administrator that improperly denies payment.
In any case, the TPA issued full payment for the services rendered at the billed charges.
All Medical-Legal evaluators must know that unjustifiable payment denials will happen, even when you do everything right, because California law incentivizes claims administrators to deny compliant bills.
Since no enforcement of regulatory penalties occurs for Helmsman or any claims administrator’s payment errors or non-compliance, evaluators must be ready to fight back with timely, complete Second Review appeals (and a letter of protest against this payment abuse can’t hurt either).
Med-Legal billing requires specialized expertise. daisyCollect professionals use our advanced software (and years of experience) to protect your practice.
Learn More About daisyCollect
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.
.gif)