JT2 Plays IBR Chicken (and Wins)
As we often point out, it can seem as if payers play a twisted game of IBR Chicken with doctors, reflexively denying bills and Second Review appeals only to change their mind once the doctor requests Independent Bill Review (IBR).
We can’t say whether JT2 Integrated Resources employs that approach. But the third-party administrator (TPA) recently blinked after the doctor requested IBR — then put on a truly embarrassing display in a panicked attempt to avoid an IBR decision (readers, get ready to cringe).
In theory, an IBR ruling in favor of the doctor would require JT2 to pay penalties, interest, and restoration of the $180 IBR filing fee to the doctor. In reality, those payments are “self-executing.” California regulators do not seem to care whether JT2 actually pays what they owe.
Pro tip for the good folks at JT2: don’t work so hard to avoid the consequences of your improper payment denials. In California workers’ comp, consequences for payer misbehavior are mythical things, spoken of but never seen.
CA Law Encourages IBR Chicken
We can’t accuse anyone of knowingly misadjudicating bills. But JT2’s actions demonstrate how California workers’ comp laws encourage payers to play IBR Chicken (yes, we purchased the domain name already).
The payer strategy is simple, and without cost or consequence: Deny payment → Deny again on Second Review →If the doctor requests IBR, reverse course and pay up.
This IBR Chicken strategy means that the payer owes the doctor no money for treating injured workers unless the doctor is willing to risk $180, the DWC allows IBR, and the doctor prevails at IBR…and even then, the payer can enjoy a good laugh as the doctor waits (and waits and waits) for the payer to “self-execute” the penalties, interest, and $180 filing fee.
To receive payment for a Supplemental Medical-Legal Report (ML106), JT2 forced the evaluator (via DaisyCollect, as the evaluator’s billing agent) to submit three bill submissions as follows:
- An initial bill (JT2 denied payment)
- A Second Review appeal (JT2 denied payment)
- An IBR request (and $180 filing fee)
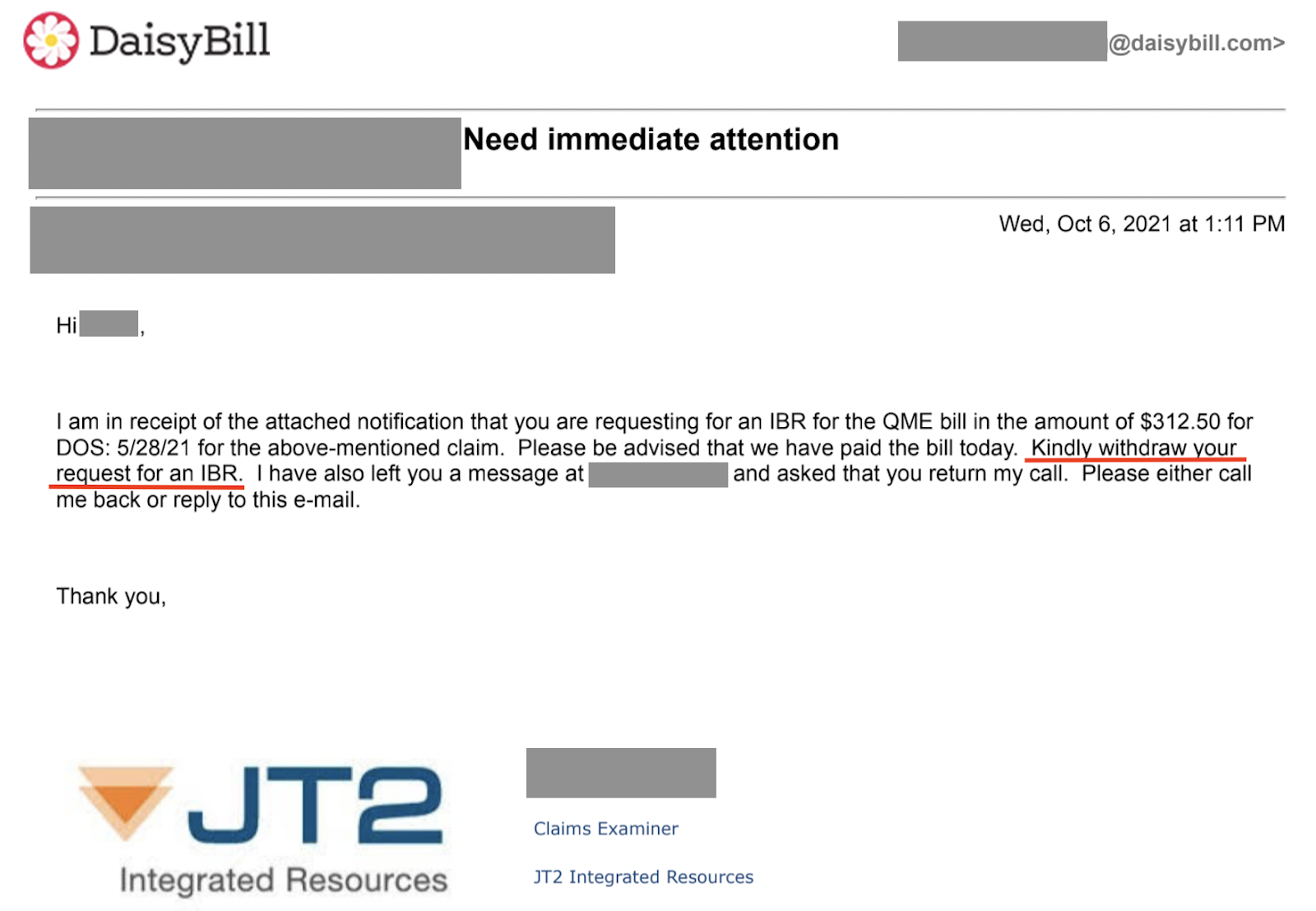
After the doctor paid $180 to file for IBR, JT2 took the following actions:
- Paid the medical-legal bill (JT2 did not wait for IBR decision)
- Contacted provider demanding the withdrawal of IBR (without reimbursing the provider for penalties, interest, or the IBR filing fee)
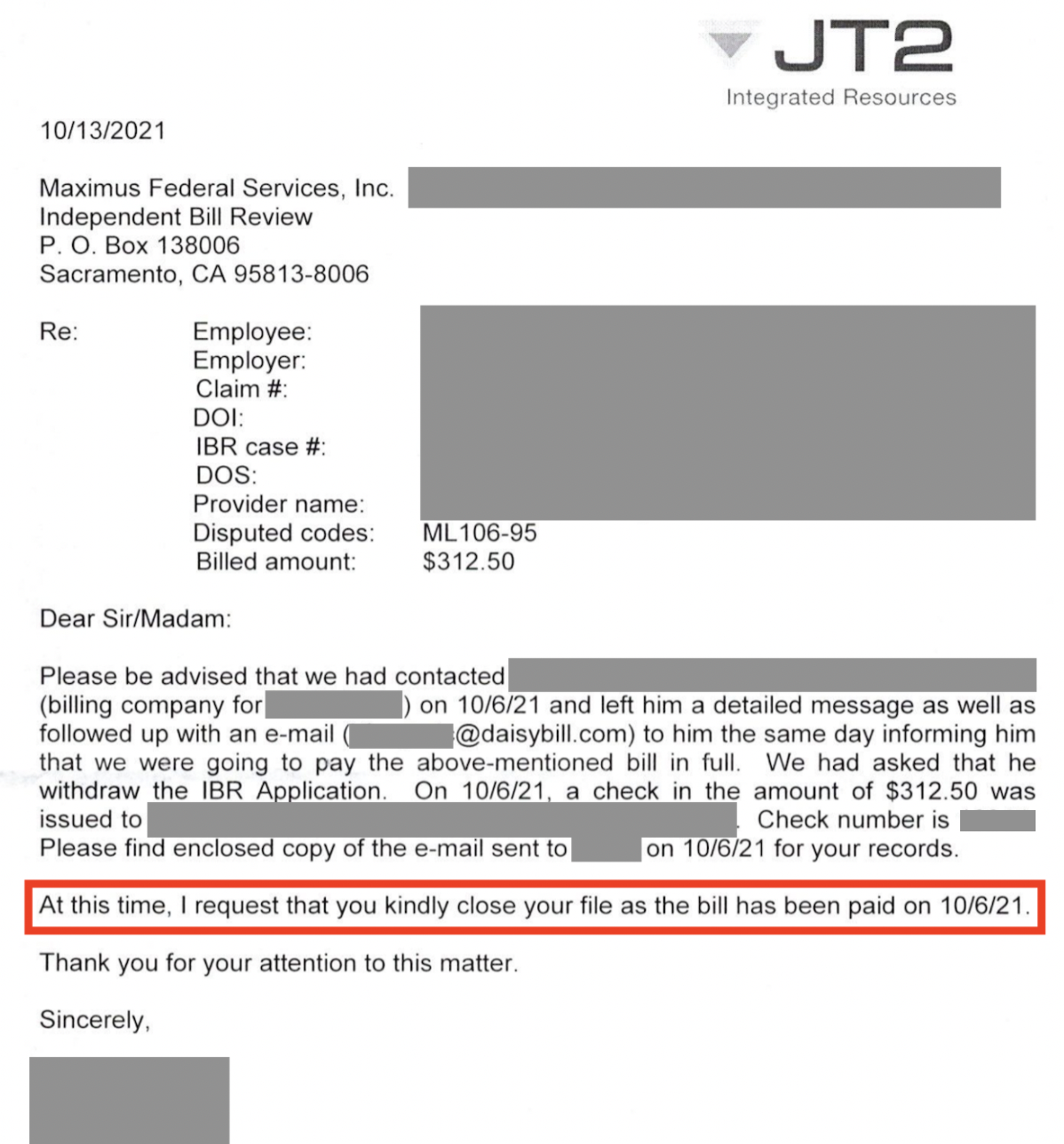
- Contacted the state’s IBR organization, Maximus, demanding they “close” the IBR case (On the grounds that JT2 capitulated and paid the doctor)
In a series of increasingly frantic emails and voicemails, JT2 insisted that the IBR request be withdrawn, since JT2 opted to pay the disputed amount. The provider refused. JT2, strangely, even asked Maximus to drop the “frivolous” case, all because JT2 blinked first.
We consider this a teachable moment. The lesson? DaisyCollect providers will not withdraw IBRs when, rather than paying the provider, claims administrators (frivolously) waste provider time and resources.
Of course, JT2 still owes this doctor penalties, interest, and the $180 IBR filing fee — not that we expect to actually see these payments, or the DWC to lift a finger in the med-legal doctor’s defense.
JT2 Attempts To Have IBR Case Dismissed
Shortly after paying $180 to file for IBR, we received an email and voicemail in which a JT2 representative agreed to pay the disputed amount, and asked DaisyBill to withdraw the IBR request.
DaisyBill also received a copy of a letter from JT2 to Maximus, in which JT2 presumed to tell Maximus to forget the whole dispute.
Unfortunately for JT2, two facts remain true (for now):
- Only at the provider’s request will Maximus “close the file” on an ongoing IBR case.
- When Maximus rules in favor of the provider, the claims administrator owes penalties, interest, and restoration of the $180 IBR filing fee in addition to the disputed amount.
Following JT2’s letter, Maximus reached out to DaisyBill to ask whether the IBR request would be withdrawn. Our agents informed Maximus that IBR would proceed — at which point JT2 escalated its tantrum.
JT2 Fails IBR 101
First came a voicemail expressing JT2’s frustration at not being let off the hook. JT2 claimed the IBR request “would be something you would have to withdraw, which [JT2] had requested because that’s wasting [Maximus’] time when it’s already been paid.”
Wait, what? Wasting Maximus’ time?
- What about the three bills the doctor was forced to submit (totaling 70 pages of bills and reports submitted)?
- What about the $180 JT2 forced the doctor to pay?
In addition to the voicemail, JT2 followed up by sending Maximus an email, stating (emphasis added):
…I wanted to make sure that Maximus is aware that this [is] now frivolous as the issue had been resolved and all parties were notified timely. I would not be liable for paying Maximus’ review fee given that the disputed amount has been paid in full.
Please respond…and advise why you would not withdraw your IBR referral and would still want to move forward with the IBR process when the matter is resolved.
Except the matter is not “resolved.” By law, JT2 owes this doctor more than just the disputed amount, as detailed above. Fortunately for JT2, California laws are only as consequential as our dormant state agencies make them.
JT2, next time, don’t panic. California IBR Chicken is a rigged game that payers always win.
Make workers’ comp a better investment. From fee schedule calculators to billing software to complete managed billing, DaisyBill has your back. Contact us to learn more.
LET’S CHAT!
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.