SCIF, EK Health Use "ODG" Guidelines to Deny Care

For injured California workers, simply getting the appropriate care can be a nightmare of bureaucratic obstacles and interminable delays.
An additional complication has now infected the process: treatment utilization guidelines that allow insurers and their Utilization Review Organizations (UROs) to deny treatment — even when the state-designated Medical Treatment Utilization Schedule (MTUS) supports the treatment.
Case in point: State Compensation Insurance Fund (SCIF) and its URO, EK Health, repeatedly reference the “Official Disability Guidelines” (ODG) in UR decisions sent in response to Requests for Authorization (RFAs) sent by physicians.
The ODG, peddled by a subsidiary of the Hearst Health Network, has not been adopted by California or the Division of Workers’ Compensation (DWC). Yet repeated references to the ODG are found throughout the word soup of SCIF and EK Health’s bloated UR decisions denying doctors’ requested treatments.
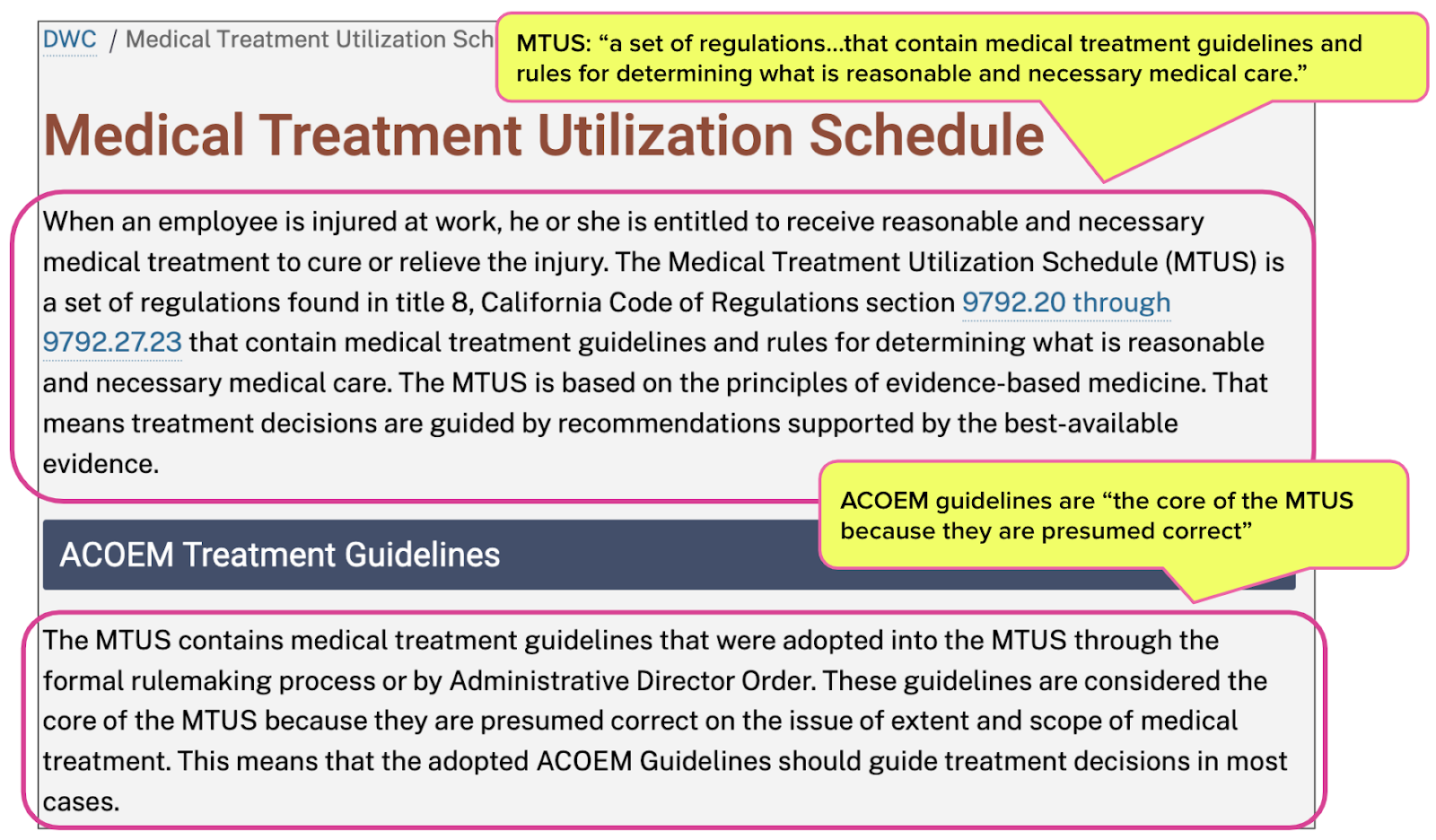
MTUS: CA’s Designated Tx Guidelines
The MTUS comprises treatment guidelines from the American College of Occupational and Environmental Medicine (ACOEM), as adopted by the DWC for use in California workers’ comp. The DWC provides free access to the MTUS for California doctors.
California Code of Regulations Section Section 9792.21 directs (emphases ours):
“The recommended guidelines set forth in the MTUS are presumptively correct on the issue of extent and scope of medical treatment.
The MTUS constitutes the standard for the provision of medical care in accordance with Labor Code section 4600 for all injured workers diagnosed with industrial conditions because it provides a framework for the most effective treatment of work-related illness or injury to achieve functional improvement, return-to-work, and disability prevention.
The MTUS shall be the primary source of guidance for treating physicians and physician reviewers for the evaluation and treatment of injured workers.”
The DWC website (shown below) is also resoundingly clear on the issue, stating:
- Injured workers are entitled to “reasonable and necessary medical treatment.”
- The MTUS contains the “guidelines and rules for determining what is reasonable and necessary medical care.”
There’s no question: when a treating or UR doctor considers whether treatment is medically necessary and appropriate, the MTUS is the authority.
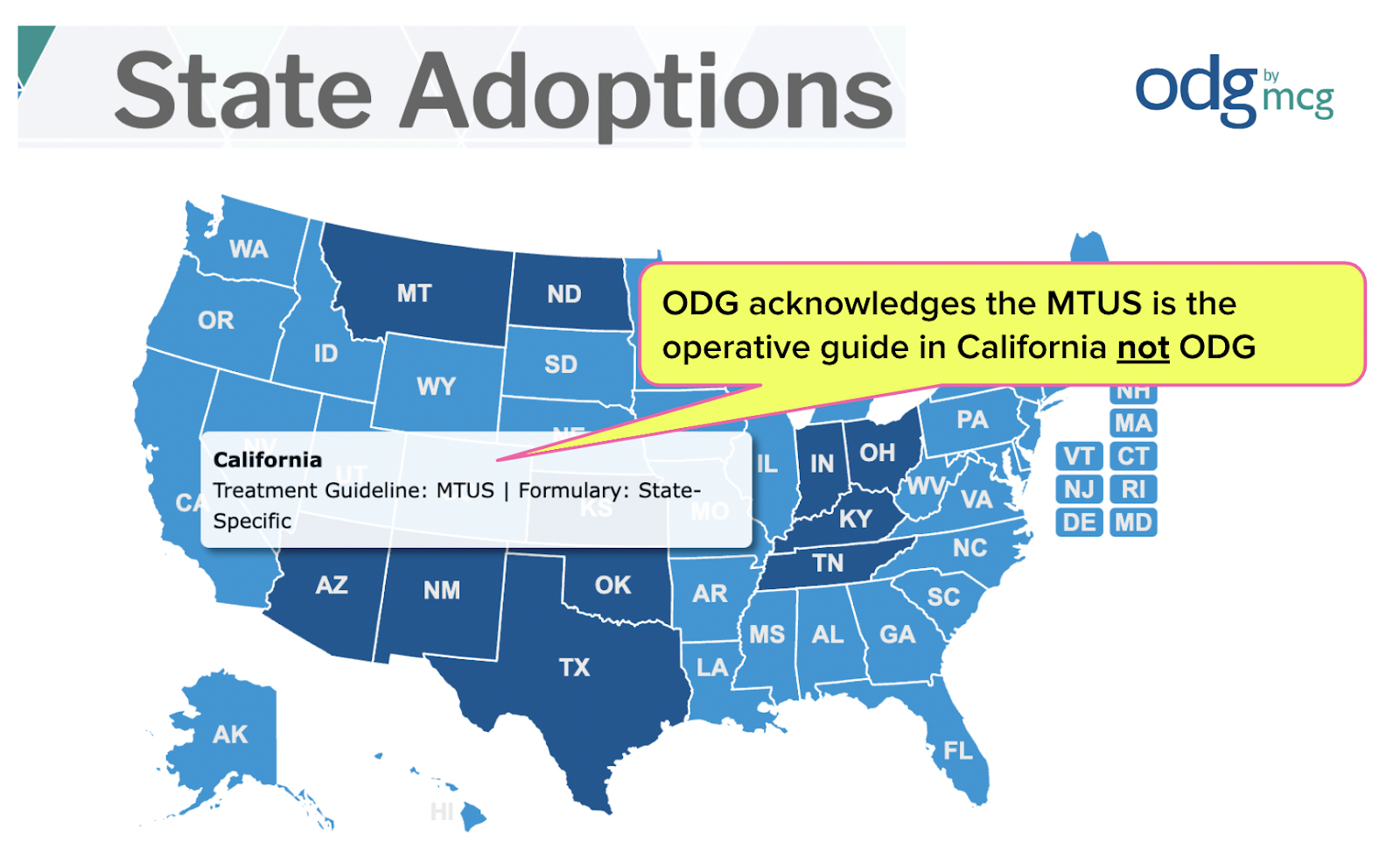
ODG: “Decision Support” for UROs
Milliman Care Guidelines, LLC (MCG), owned by the Hearst Health Network, produces the ODG, which, according to the ODG website offers:
“...highly configurable, industry-specific medical treatment and return-to-work solutions that are used for managing workers’ compensation, disability, and auto liability claim outcomes with evidence-based, data-driven decision support.”
Even the ODG website acknowledges that California uses the MTUS as its treatment guideline, not the ODG.
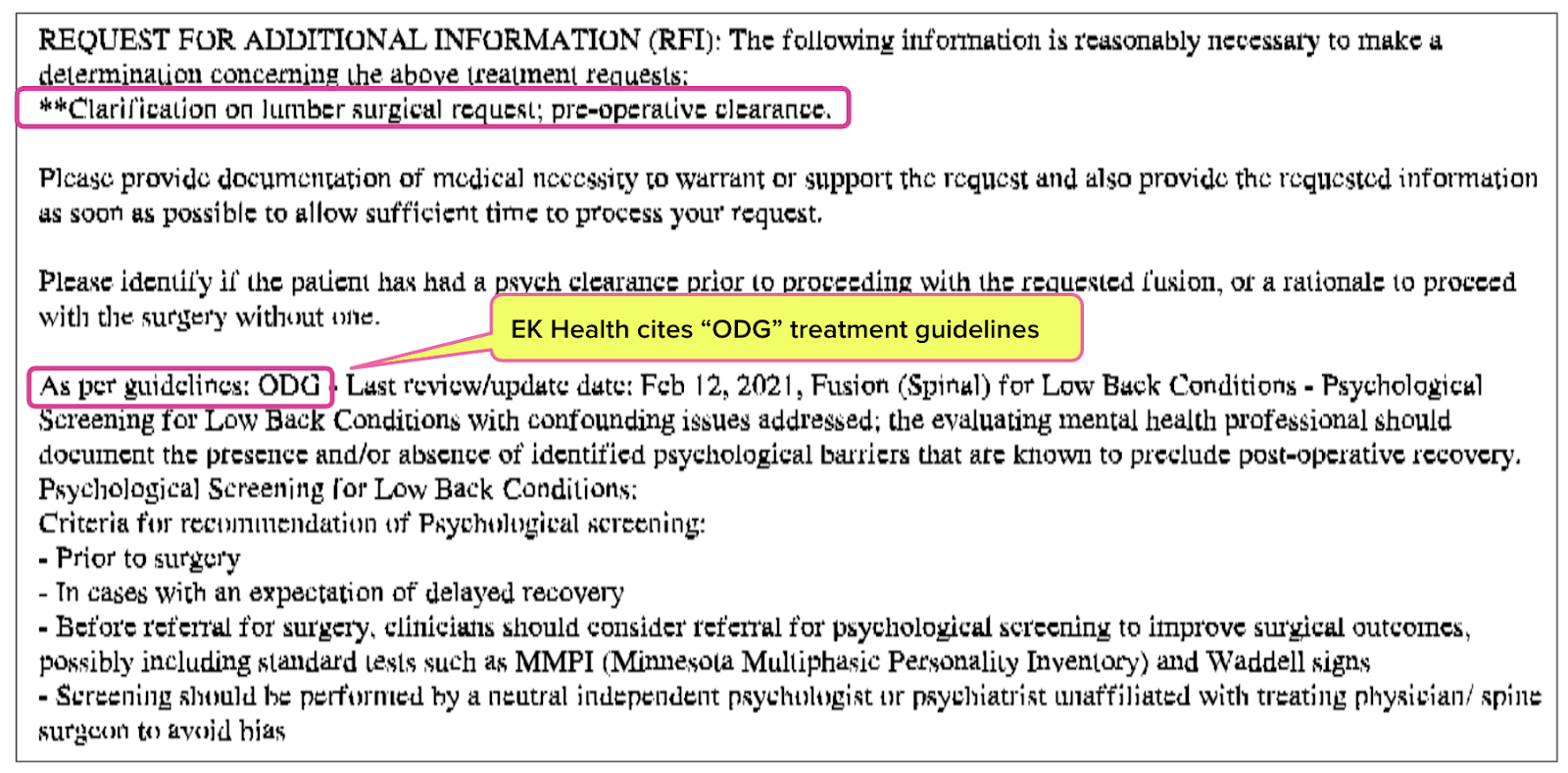
SCIF/EK Health Cite ODG
SCIF and EK Health repeatedly cite ODG guidelines in UR decisions sent to physicians. Worse, these entities have used the ODG to deny surgery recommended by physicians.
In the two UR decisions (shown below) sent in response to the treating doctor’s Request for Authorization (RFA), the insurer refused to allow surgery without a preoperative psychological screening. However, the MTUS does not require any such screening.
Yet in both cases, SCIF and EK Health refused to allow the surgery without the ODG-required screening, significantly and needlessly delaying the injured workers’ care.
We cannot comment on any treatment's actual medical necessity or appropriateness. But serious questions can (and should) be asked surrounding whether treatment guidelines should be “highly configurable” with the stated goal of “decision support” — especially when insurers and UROs choose those guidelines over the state’s designated treatment utilization schedule.
The MTUS, not the ODG, is what California physicians (including UR physicians) should be using. As attractive as the latter may be to insurers that arguably appear to be shopping for boutique treatment guidelines to cite in denials of care.
We make getting authorization for the care your patients need faster and easier. Get a free demo of daisyAuth below!
DAISYAUTH DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.png)

This tactic does not surprise me at all! The worst part about it is that this is being done by a California State employer/insurer. When you can't even be covered and receive quality care when you work for a state agency is beyond disgusting.