SCIF Inept UR #7: Truly Unbelievable Incompetence
.png)
Employees, taxpayers, and moral human beings should be outraged by Utilization Review (UR) abuse inflicted on a state employee by the State Compensation Insurance Fund (SCIF).
As detailed below, SCIF’s Utilization Review Organization (URO), EK Health, improperly denied a simple trigger point injection that costs less than $100. EK Health listed the denial reason as “Lack of Information” — even though the UR decision contained the information EK Health claimed was “lacking.”
This demonstrates (once again) that California’s broken UR system allows insurers and UROs, rather than treating physicians, to make medical decisions from which insurers ultimately profit at the expense of injured workers’ health. Moreover, this story features:
- A state employee denied appropriate treatment for debilitating work injuries
- An employer (and taxpayers) paying a URO for an inept, incorrect UR decision
- The dire plight of anyone injured at work in California
We will continue to publish these stories of indefensible behavior by insurers and UROs and to demand oversight and reform of the UR system by California’s silent, absent Division of Workers’ Compensation (DWC).
Step by step, this is how SCIF and EK Health handled a compliant, straightforward Request for Authorization (RFA) — and the mistreatment an insurer and URO inflicted on this injured employee.
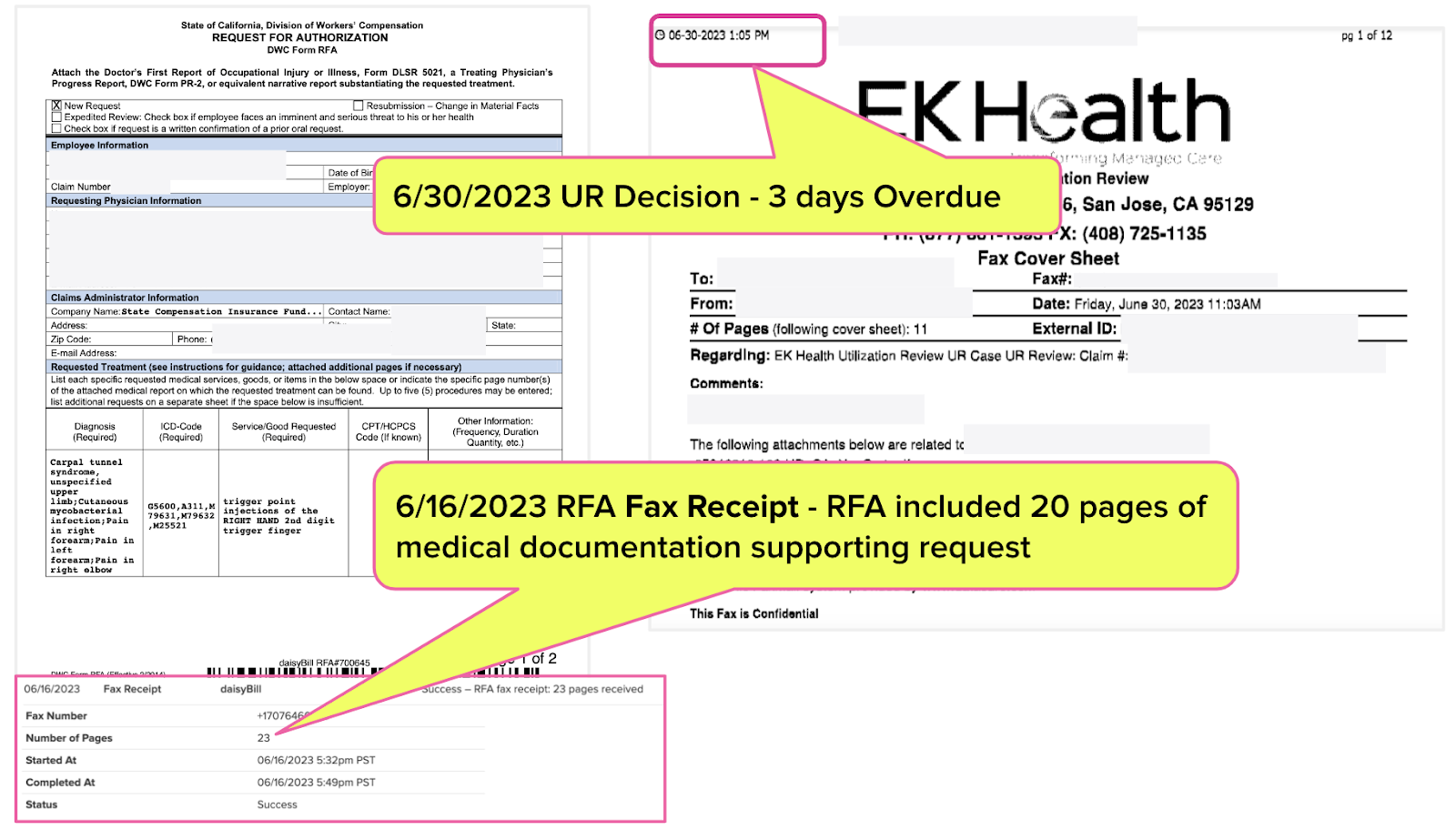
1. Physician Requests $98 Treatment
An employee of the State of California suffered an injury to the thumb and index finger from data entry work. The treating physician submitted an RFA to SCIF for a trigger point injection, a treatment that proved effective previously.
The total cost of the recommended procedure per the Official Medical Fee Schedule (OMFS) is $98.03.
The medical documentation the physician faxed with the RFA noted that a previous trigger point injection significantly reduced the pain level the injured worker experienced, allowing them to “work full time with a heavier workload.” The medical report stated:
“Consequent to trigger point injection to the left dorsal forearm there has been a reduction of pain from the level of 9. Other than mild bruising to the area of injection there were no other adverse events. Functionality has increased.”
The physician faxed the RFA with 20 pages of supporting documentation on June 15, 2023. EK Health returned their UR decision on June 30 — three days after the legally mandated deadline.
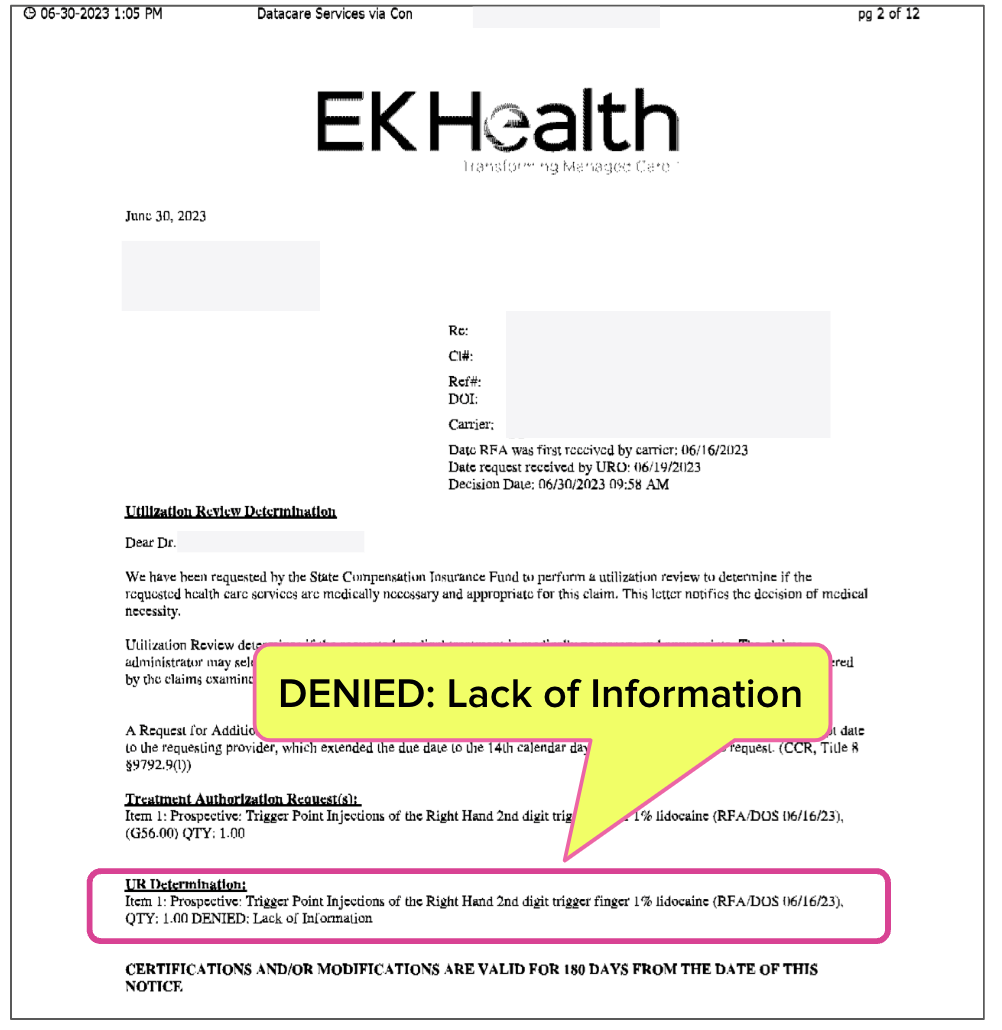
2. EK Health Denies Treatment
The 12-page late UR decision from EK Health denied the injection due to a “Lack of Information.”
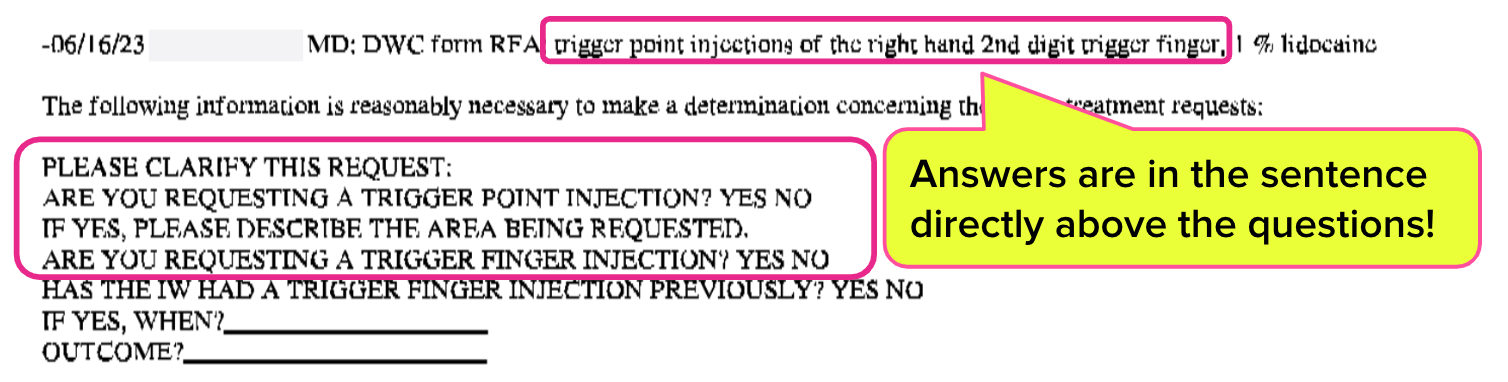
3. EK Health Requests Information (That’s Listed in the UR Decision)
Sit down for this part. Page 3 of the UR decision lists the medical treatment the physician requested on the RFA form faxed to SCIF: “trigger point injections of the right hand 2nd digit trigger finger.”
However, the UR physician, in all caps, asks the requesting physician to “clarify” the following:
ARE YOU REQUESTING A TRIGGER POINT INJECTION?
IF YES, PLEASE DESCRIBE THE AREA BEING REQUESTED.
ARE YOU REQUESTING A TRIGGER FINGER INJECTION?
You read that right. The answers the EK Health physician needed to make a medical determination were listed (directly) above the questions in the UR decision.
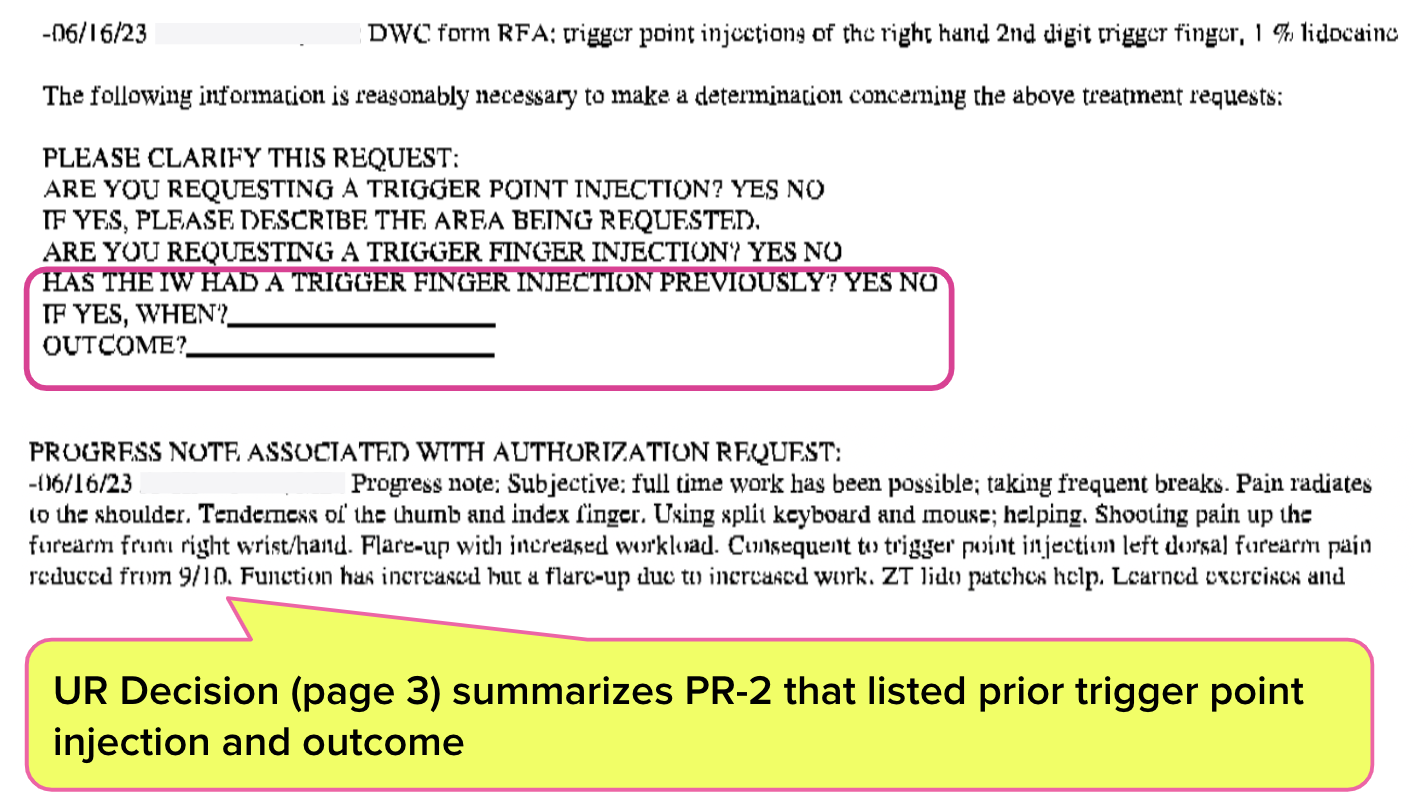
Also, on page 3, the UR decision summarizes the PR-2 report the treating physician faxed with the RFA. This summary describes both the previous injection and its outcome. However, as shown below, the UR physician requests the information already summarized in the UR decision.
HAS THE IW [injured worker] HAD A TRIGGER FINGER INJECTION PREVIOUSLY?
IF YES, WHEN?
OUTCOME?
How is this level of ineptitude possible? It’s challenging not to (rationally) wonder whether UROs are making thoughtful medical determinations, or simply trying to save insurers a buck.
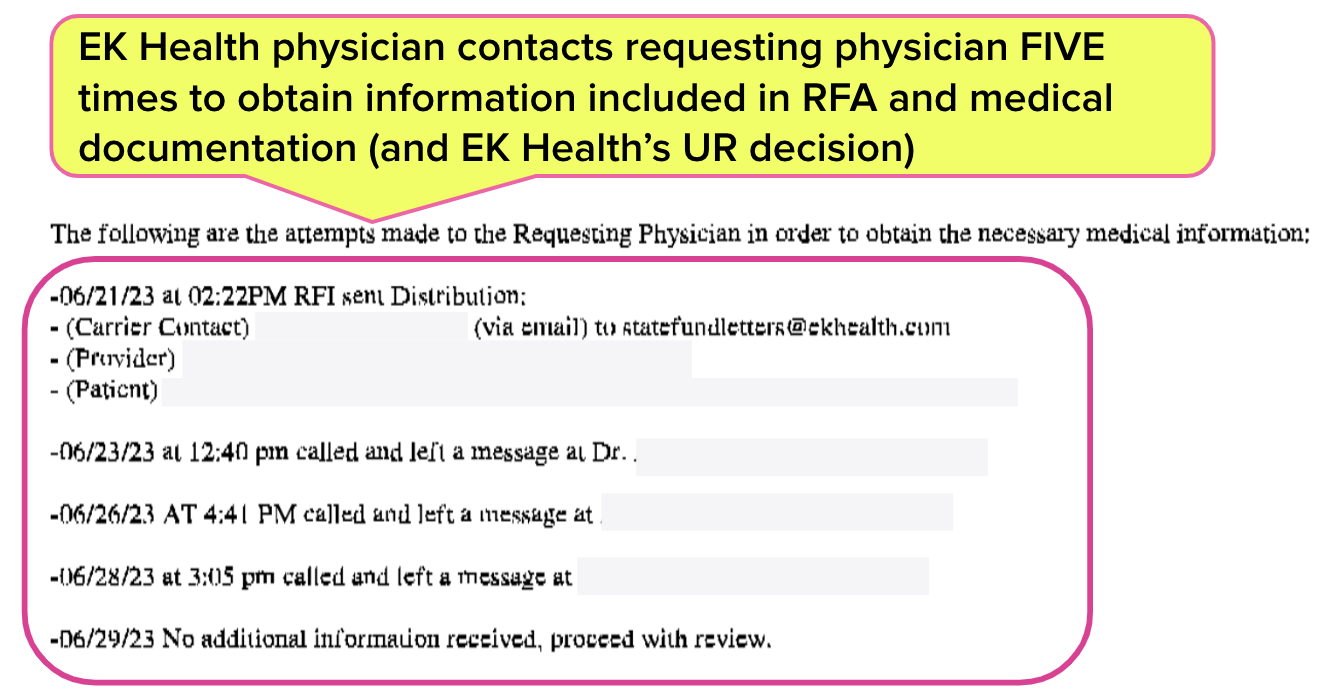
4. EK Health UR Physician Badgers Requesting MD
As shown above, the answers to the EK Health UR physician’s questions were right before their eyes. Nevertheless, EK Health pestered the doctor with repeated phone calls to obtain the information listed in the UR decision.
Remember, this is a state employee. This means, presumably, California taxpayers paid for EK Health to pointlessly hassle the requesting physician for information already in EK Health’s possession. Yes, your tax dollars are at work preventing injured state employees from receiving a $100 medical treatment that previously returned the employee to full employment.
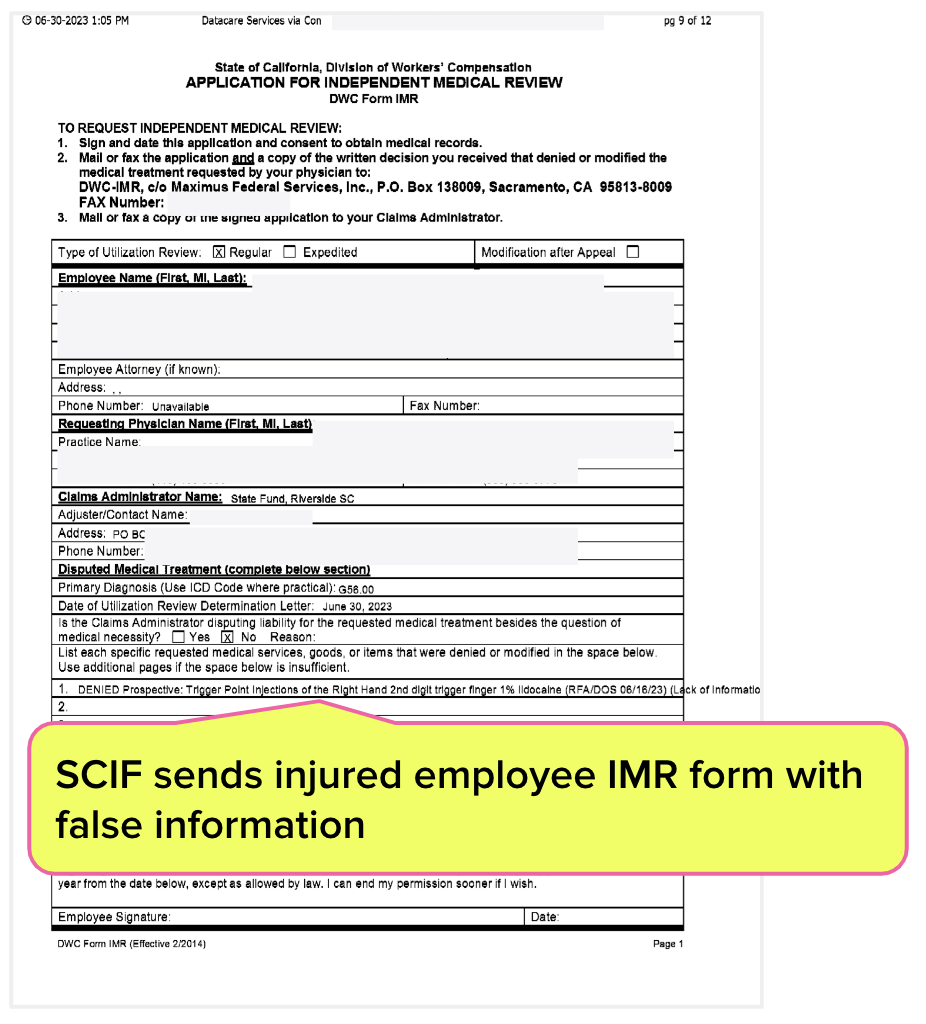
5. SCIF Sends Injured Worker IMR Form With False Information
California requires that insurers/UROs attach a completed application form for Independent Medical Review (IMR) with UR denials so the injured worker can appeal the decision (not that it will help).
Below is the IMR form SCIF completed and sent to the injured state employee, which, true to form, cited “Lack of medical informati[on]” as the denial reason.
According to DWC IMR rules, an authorization dispute is deemed ineligible for IMR if the UR decision “does not reflect a determination of medical necessity (conditional non-certification).” As further explanation, the DWC defines a “conditionally non-certified decision (CNC)” as follows [emphasis added]:
“A UR decision that has been denied because the treating physician has not provided the medical information requested by the claims administrator that is required to make a medical necessity determination on the treatment recommendation.”
DWC: MIA
The framers of the Constitution once wrote, “If men were angels, no government would be necessary.” This acknowledges that without laws, regulations, and enforcement, people and profit-seeking entities will inevitably do bad things that harm citizens.
The sentiment remains true. Insurers and UROs like SCIF and EK Health are not angels, as evidenced by the many stories we’ve published regarding their treatment of injured workers. The DWC needs to govern in order to prevent the harm these entities are inflicting.
The problem is…the DWC isn’t doing much governing at all.
UR decisions can arrive late and in any format, however dense or illegible. Worst of all, under this DWC’s administration, UR decisions don’t have to make rational sense. There are no consequences for late decisions or improper denials — except those that fall on the injured worker, who must (literally) suffer the results.
We’ve gone beyond a simple failure of regulatory enforcement and crossed over into a moral failure. The regulators are missing in action, and it’s open season on the vulnerable.
We can’t make insurers comply with laws or the DWC do its job — but we can make authorization easier and faster for providers. Get your free daisyAuth demo below.
FREE DEMO: DAISYAUTH
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.gif)
I see this everyday the Doctors who is the reviewing doctor comes up with crazy excuses, if they are getting paid more if they talk to the requesting doctor they will make every attempt to talk to the requesting doctor even if they have all the information they need to make a educated decision now who is committing fraud. Delaying care for obvious work comp patient the reviewing doctors are laughing all the way to the back, when are they held accountable.