Paradigm Network: Medicare Cuts Impact Workers' Comp Reimbursements

At first glance, recently announced Medicare payment reductions may seem to have little to do with workers’ comp. But thanks to discount reimbursement contracts, Medicare cuts can mean lower 2024 reimbursements for treating injured workers.
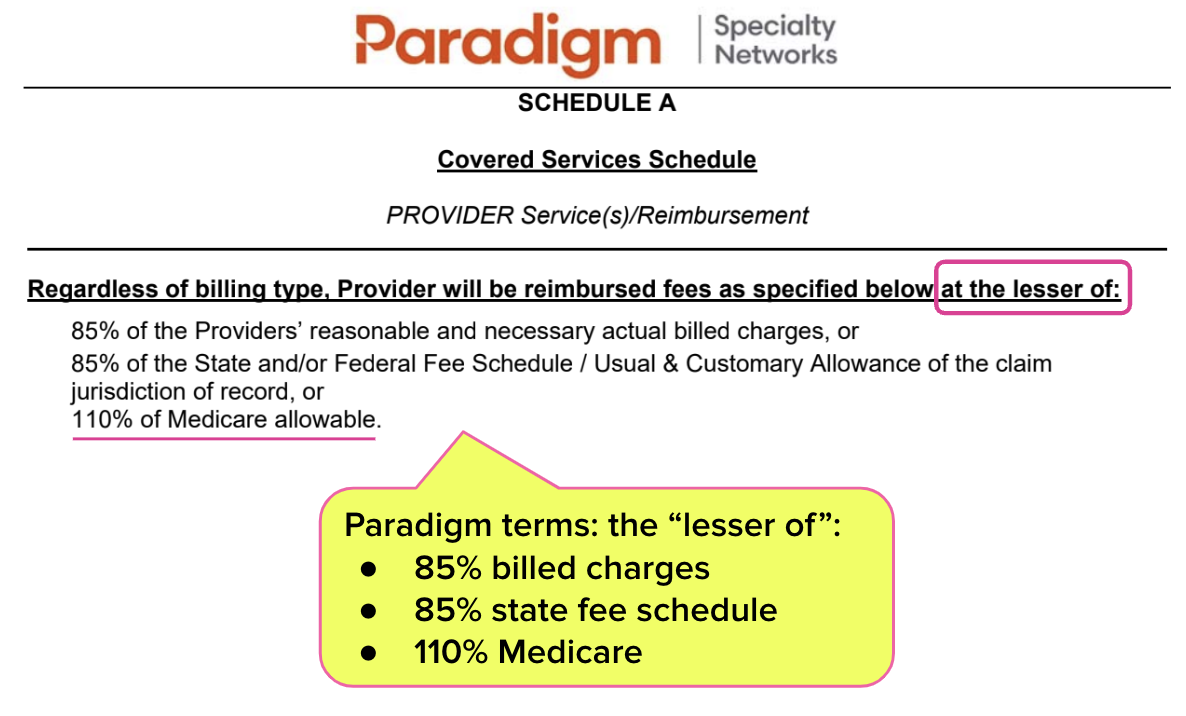
For example, the terms of discount agreements with specialty network Paradigm specify that the provider receives the “lesser of” several reimbursement options, including a percentage of the Medicare rates for the services rendered.
In other words, if a provider has signed a “lesser of” Medicare discount reimbursement contract, the reimbursements established by state workers’ comp fee schedules don’t apply. Medicare’s 2024 reduced rates will mean lower reimbursements for providers who have signed these contracts — even if the state workers’ comp fee schedule rates were to quadruple in 2024.
Paradigm: 110% of Medicare Rates for Injured Worker Treatment
Throughout the United States, many providers sign specialty network discount contracts under the impression that joining the network increases the number of injured workers who visit the practice.
In California, some providers sign these specialty network contracts under threat of exclusion from Medical Provider Networks (MPNs); if the provider refuses a contract, they’re booted from the associated MPN and rendered ineligible to treat injured workers restricted to that MPN.
However, providers are often surprised to see how much revenue they sacrifice in exchange for the vague hope of more patients. Further, they are shocked by how rapidly these contractual rates are leased, sold, or otherwise shared with multiple bill review companies, slashing workers’ comp revenue across the practice.
For example, the Paradigm contract below offers reimbursement terms using the infamous “lesser of” language. Common to network discount contracts, this language mandates the provider receive the “lesser of” several possible reimbursement amounts.
In this case, the provider receives the “lesser of”:
- 85% of the provider’s billed charges
- 85% of the state fee schedule rate
- 110% of the Medicare rate
The terms of this Paradigm contract mean that even if state regulators increase state fee schedule reimbursements, the provider would still receive only slightly above Medicare rates for treating injured workers.
The PPO & Network Discount Problem
Treating injured workers is vastly more expensive than treating Medicare patients. Nationwide, most physicians avoid treating injured workers because the administrative costs and billing complexities make workers’ comp an untenable financial proposition.
Accordingly, states try to incentivize providers to treat injured workers by increasing state workers’ comp fee schedule rates relative to Medicare rates. But with discount contracts like Paradigm’s in play, higher state fee schedules are irrelevant.
Once again, now is the time for providers to cancel or renegotiate their discount contracts (daisyBill has assisted many clients with this undertaking).
At the very least, every provider who treats injured workers should run their 2023 numbers and determine if these discount contracts deliver enough injured workers to justify even lower payments in 2024.
With services ranging from fee schedule calculators to fully managed workers’ comp billing, daisyBill can help protect and empower your practice. Reach out to learn more.
LET’S CHAT
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.gif)