The $10,000 Lie California Tells Injured Workers
Lie: California workers receive immediate and continued treatment (up to $10,000) when they file a work injury claim.
Fact: California allows claims administrators to defer Utilization Review (UR) and therefore refuse treatment authorization for up to 90 days, leaving providers unable to render care and forcing injured workers to beg for treatment.
When a worker files a claim, the claims administrator can either accept liability or investigate further to determine its liability or lack thereof. If the claims administrator decides to investigate the injury, California law allows the claims administrator to defer their liability decision for 90 days and to defer authorizing care while determining liability.
Most importantly for the injured worker, while the claims administrator ponders liability, the treating physician cannot obtain authorization for recommended treatment—which means the injured worker goes without care.
Don’t take our word for it; the California Division of Workers’ Compensation (DWC) actually, unbelievably, explicitly instructs injured workers awaiting a liability determination to:
- Try to persuade their employer’s claims administrator to authorize care, or
- Use private health insurance to get care (a possible act of insurance fraud), or
- Find providers that will treat “without immediate payment”
We cannot know how many injured workers have gone without care while awaiting a liability decision, since the DWC also refuses to collect UR data as California law requires. Meanwhile, injured workers—some with serious or debilitating injuries—are left without essential treatment.
California’s Bait & Switch Treatment Authorization Process
California Labor Code Section 5402 dictates that within one working day of “knowledge of an injury,” the employer’s claims administrator shall authorize the provision of all appropriate treatment, and continue to provide treatment until either accepting or denying the claim (subject to a $10,000 cap), regardless of whether or not liability is ultimately accepted:
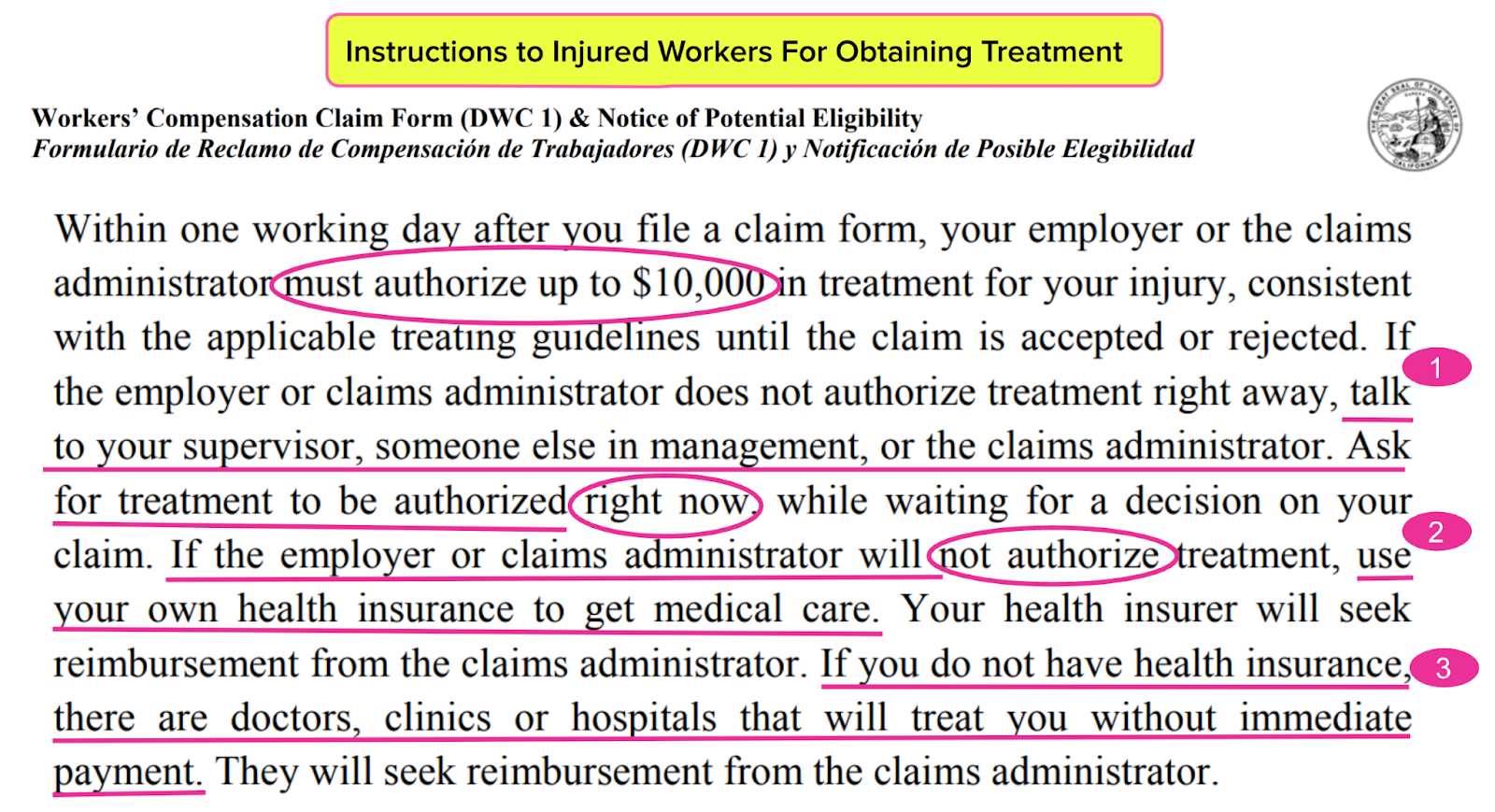
Workers must file the California Workers’ Compensation Claim Form (DWC 1) with their employer to report a work injury. This form provides instructions in English and Spanish on how to obtain care. Below, the English version of the DWC 1 instructs that claims administrators “must authorize” up to $10,000 in treatment.
However, in the very next sentence, the DWC 1 instructs that when the claims administrator refuses to authorize treatment, the injured worker must undertake one of three (absurd) steps to obtain care:
- “Talk to your supervisor, someone else in management or the claims administrator and ask for treatment to be authorized right now” (persuasion-while-injured-101)
- “If the employer or claims administrator will not authorize treatment, use your own health insurance to get medical care” (ignore those pesky questions about whether the reason for the visit is related to a work incident)
- “If you do not have health insurance, there are doctors, clinics or hospitals that will treat you without immediate payment” (you know, the abundant free care that is available throughout the United States for individuals without health insurance)
Read the following, and ask yourself how it’s possible that these are the instructions the DWC provides California’s injured workers.
What happened to the $10,000 authorization guaranteed by LC §5402? A bait-and-switch caveat makes the $10,000 promise a worthless lie, since other California UR laws and regulations allow claims administrators to defer authorization of recommended treatment for up to 90 days while the claims administrator determines liability.
Without treatment authorization from the claims administrator, a provider cannot receive $1 for treating an injured worker (much less $10,000).
CA Injured Workers Beg or Pay For Their Care
To summarize, the first piece of paperwork an injured worker gets from the DWC instructs them that they are owed immediate and continued treatment, regardless of liability—but also that no government official is going to enforce this obligation while waiting for a decision on their claim.
The DWC instructs injured workers to persuade, pay, or plead for care for up to 90 days. For a full three months, potentially necessary care may be out of reach, despite laws and regulations in place to protect workers in this exact situation.
None of this should surprise anyone who studies California’s workers’ comp system, where the priority is profits for claims administrators, side-kick vendors, and their private equity owners.
Now imagine tripping, falling, and hitting your head at work—then being handed the instructions above and required to navigate this contradictory, effectively ungoverned system. The results can only be as tragic as they are predictable.
Submit RFAs in 30 seconds and automatically track UR decisions with daisyAuth. Request a demo below!
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.

%20(1).gif)


